Abstract
There are new techniques which have been developed in order to assess objective functional data concerning the severity and type of abnormalities in infants and children with lung disease. In the present review some applications of the various techniques are given in connection with deductions, which can be based on such functional findings. Insight into the mechanisms leading to lung disease and the institution of appropriate therapeutic guidelines largely depend on whether the degree of pulmonary hyperinflation or restriction, of bronchial obstruction, of bronchial hyperreactivity, of ventilation inequalities and the function of gas exchange can be objectively evaluated. Recent advances in the non-invasive assessment of lung function in infants and children promises progress in this task.
Similar content being viewed by others
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- CF:
-
cystic fibrosis
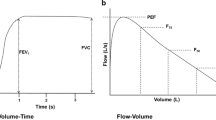
- FEV1 :
-
forced expiratory volume in 1 s
- Gaw:
-
airway conductance, plethysmographically determined
- MEF50 :
-
maximal expiratory flow at 50% expired vital capacity
- MIF50 :
-
maximal inspiratory flow at 50% inspired vital capacity
- PD65 :
-
Provocation dose inducing 65% increase of respiratory resistance
- Raw:
-
Airway resistance, plethysmographically determined
- Rint :
-
Respiratory resistance, measured by interruption technique
- TGV:
-
Thoracic gas volume; measuring end-expiratory resting level by the plethysmographic technique
References
Auld PAM, Nelson NM, Cherry RB, Rudolph AJ, Smith CA (1963) Measurement of thoracic gas volume in the newborn infant. J Clin Invest 42:476–483
Briscoe WA, Dubois AB (1958) The relationship between airway resistance, airway conductance and lung volumes in subjects of different age and body size. J Clin Invest 37:1279–1285
Clements JA, Sharp JT, Johnson RP, Elam JO (1959) Estimation of pulmonary resistance be repetitive interruption of airflow. J Clin Invest 38:1262–1270
Doershuk CF, Downs TD, Matthews LW, Lough MD (1970) A method for ventilatory measurements in subjects 1 month to 5 years of age: normal values and observation in disease. Pediatr Res 4:165–177
DuBois AB, Botelho SY, Comroe JH Jr (1956) A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest 35:327–335
DuBois AB, Botelho SY, Bedell GN, Marshall R, Comroe JH Jr (1959) A rapid plethysmographic method for measuring thoracic gas volume: a comparison with a nitrogen washout method for measuring functional residual capacity in normal subjects. J Clin Invest 35:322–326
Frey U, Kraemer R (1990) Visco-elastic properties of the lung, assessed by the flow-interruption technique in children. Am Rev Respir Dis 141:A714
Frey U, Schibler A, Kraemer R (1992) Changes in postocclusional oscillatory pressure transients after flow interruption during bronchial challenge in healthy and asthmatic children. Am Rev Respir Dis 145:A251
Gaultier CI, Allaire Y, Pappo A, Girard F, Gerbeaux J (1975) Résistance pulmonaire totale chez l'enfant sain et l'enfant asthmatique: Corrélation avec le VEMS et la compliance pulmonaire dynamique. Rév Fr Mal Respir 11:827–831
Geubelle F, Karlberg P, Koch G, Lind J, Wallgren G, Wegelius C (1959) L'aération du poumon chez le noveau-né. Biol Neonat 1:169–172
Godfrey S (1983) The “wheezy baby” syndrome. In: Clork TJH, Godfrey S (eds) Asthma, 2nd edn. Chapman and Hall Medical, London, pp 416–418
Hatch DJ, Tayler BW (1976) Thoracic gas volume in early childhood. Arch Dis Child 51:859–864
Holmann JC, Schibler A, Kraemer R (1989) Charakteristika der inspiratorischen Fluss-Volumen-Kurven bei Kindern mit Asthma bronchiale und Patienten mit zystischer Fibrose. Schweiz Med Wochenschr 119:1713–1718
Jackson AC, Milhorn HT, Norman JR (1974) A reevaluation of interrupter technique for airway resistance measurements. J Appl Physiol 36:264–268
Klaus M, Tooley WH, Weaver KH, Clements JA (1962) Lung volumes in the newborn infant. Pediatrics 30:111–116
Kraemer R (1990) Intrasubject variability and interindividual sensitivity of whole-body plethysmographic measurements in wheezy infants. Am Rev Respir Dis 141:A286
Kraemer R, Meister B (1985) Fast real-time moment-ratio analysis of multibreath nitrogen washout in children. J Appl Physiol 59:1137–1144
Kraemer R, Schöni MH (1990) Ventilatory inequalities, pulmonary function and blood oxygenation in advanced states of cystic fibrosis. Respiration 57:318–324
Kraemer R, Heinzen P, Röli HJ, Meister B, Rossi E (1982) Klinische Formen und lungenphysiologische Veränderungen bei Kindern mit Asthma bronchiale. Schweiz Med Wochenschr 112:12—73—79
Kraemer R, Meister B, Schaad UB, Rossi E (1983) Reversibility of lung function abnormalities in children with perennial asthma. J Pediatr 102:347–350
Kraemer R, Zehnder M, Meister B (1986) Intrapulmonary gas distribution in healthy children. Respir Physiol 65:127–137
Kraemer R, Birrer P, Schöni MH (1988) Dose-response relationship and time course of the response to systemic beta adrenoreceptor agonists in infants with bronchopulmonary disease. Thorax 43:770–776
Kraemer R, Frey U, Wirz Sommer C, Russi E (1991) Shortterm effect of albuterol, delivered via a new auxiliary device, in wheezy infants. Am Rev Respir Dis 144:347–351
Kraemer R, Birrer P, Modelska K, Casaulta Aebischer C, Schöni MH (1992) A new baby-spacer-device for aerosolized bronchodilator administration in infants with bronchopulmonary disease. Eur J Pediatr 151:57–60
Kraemer R, Casaulta Aebischer C, Frey U, Rüdeberg A (1992) Interrelationship between biometric and lung funciton data in infants with cystic fibrosis (CF). Am Rev Respir Dis 145:A115
Mead J, Whittenberger JL (1954) Evaluation of the airway interruption technique as method for measuring pulmonary airflow resistance. J Appl Physiol 6:408–416
Nelson NM, Prodhom LS, Cherry RB, Lipsitz PJ, Smith CA (1963) Pulmonary function in the newborn. V. Trapped gases in the normal infant's lung. J Clin Invest 42:1850–1858
Phelan DP, Williams HE (1969) Ventilatory studies in healthy infants. Pediatr Res 3:425–432
Radford M (1974) Measurements of airway resistance and thoracic gas volume in infancy. Arch Dis Child 49:611–615
Rossier PH (1966) Préface. In: Geubelle F (ed) Contribution à l'étude functionnelle du poumon de l'enfant sain et de l'enfant asthmatique. Editions J. Duculot, S.A. Gembloux, Belgique
Stocks J (1977) The functional growth and development of the lung during the first year of life. Early Hum Dev 1:285–309
Stocks J, Godfrey S (1977) Specific airway conductance in relation to postconceptional age during infancy. J Appl Physiol 43:144–154
Stocks J, Levy NM, Godfrey S (1977) A new apparatus for the accurate measurement of airway resistance in infancy. J Appl Physiol 43:155–159
Thomson AH, Beardsmore CS, Firmin R, Leanage R, Simpson H (1990) Airway function in infants with vascular rings: preoperative and postoperative assessement. Arch Dis Child 65: 171–174
Wall MA (1985) Moment analysis of multibreath nitrogen washout in young children. J Appl Physiol 49:274–279
Woolcock AJ, Read J (1965) Improvement in bronchial asthma not reflected in forced expiratory volumes. Lancet 21:134–136
Zaplethal A (1987) Lung function in children and adolescents-methods, reference values. Progr Respir Res No 22, Karger, Basel
Zeltner S, Sennhauser FH, Kraemer R (1986) Epidemiologische Aspekte des Asthma bronchiale im Kindesalter. Schweiz Med Wochenschr 116:1210–1216
Author information
Authors and Affiliations
Additional information
In part presented at the Annual Meeting of the European Society for Pediatric Research, Zürich, September 1–4th, 1991 and at the Postgraduate course on infant lung function testing of the American Thoracic Society, Miami, May 16–21th 1992
Rights and permissions
About this article
Cite this article
Kraemer, R. Practical interest in the detection of functional abnormalities in infants and children with lung disease. Eur J Pediatr 152, 382–386 (1993). https://doi.org/10.1007/BF01955891
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01955891