Summary
The effects of oral pretreatment with mioflazine (2.5 mg·kg−1) on regional myocardial reflow, infarct size reduction and hemodynamic recovery were studied in 24 anesthetized open-chest dogs undergoing 90 minutes of acute left anterior descending coronary artery (LAD) occlusion followed by 150 minutes of reperfusion.
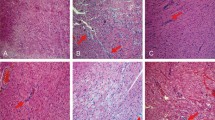
Regional myocardial blood flow was measured with tracer microspheres, and infarct size was determined by triphenyl tetrazolium chloride staining. Pretreatment with mioflazine resulted in a reduced diastolic aortic pressure (p<0.05) and an elevated cardiac output and LV dpdt max (p<0.05). These effects persisted throughout the experiment. In control animals (n=12) a hyperemic reflow response was found in the perfusion area of the LAD during the first minutes of reperfusion. After 150 min of reperfusion, however, the viable myocardium of the LAD area became underperfused, and almost no reflow was found in the infarcted zones.
In the animals pretreated with mioflazine (n=12) the hyperemic response persisted throughout the reperfusion phase and the no-reflow phenomenon was prevented. Infarct size (expressed as percentage of perfusion area) tended to be smaller in this group: 23.7±12.4% versus 33.7±19.2% (p>0.05).
Left atrial pressure increased during LAD occlusion in both groups but normalized completely in the drug-pretreated animals (p<0.05).
It is concluded that pretreatment with mioflazine prevents the no-reflow phenomenon after reperfusion of an evolving infarction, tends to reduce infarct size and improves hemodynamic recovery.
Similar content being viewed by others
References
Meyer J, Merx W, Schmitz H, Erbel R, Kiesslich T, Dorr R, Lambertz H, Beithge C, Krebs W, Bardos P, Minale C, Messmer BJ, Effert S (1982) Percutaneous transluminal coronary angioplasty immediately after inter-coronary streptolysis of transmural myocardial infarction. Circulation 66 (Suppl 5):905–916
Philips SJ, Kongtahworn C, Skinner JR, Zeff RH (1983) Emergency coronary artery reperfusion: A choice therapy for evolving myocardial infarction. J Thorac Cardiovasc Surg 86:679–688
Maroko PR, Libly P, Finks WR, Bloor CM, Shell WE, Sobel BE, Ross J Jr (1972) Coronary artery reperfusion I. Early effects on local myocardial function and the extent of myocardial necrosis. J Clin Invest 51:2710–2716
Geary GG, Smith GT, McNamara JJ (1982) Quantitative effect of early coronary artery reperfusion in baboons. Extent of salvage of the perfusion bed of an occluded artery. Circulation 66:391–396
Lang TW, Corday E, Gold H, Meerbaum S, Rubins S, Constantin C, Hirose S, Osher J, Rosen V (1974) Consequences of reperfusion after coronary occlusion. Effects of hemodynamics and regional myocardial metabolic function. Am J Cardiol 33:69–81
Bresnahan GR, Roberts R, Shell WE, Ross J Jr, Sobel BE (1974) Deleterious effects due to hemorrhage after myocardial infarction. Am J Cardiol 33:82–86
Majro G, Ames A, Chiang J, Wright RL (1967) No reflow after cerebral ischemia. Lancet 2:569–570
Summers WK, Janison RL (1971) The no reflow phenomenon in renal ischemia. Lab Invest 25:635–643
Kloner RA, Ganote CE, Jennings RB (1974) The “no-reflow” phenomenon after temporary coronary occlusion in the dog. J Clin Invest 54:1496–1508
Kloner RA, Ganote CE, Whalen DA Jr, Jennings RB (1974) Effects of transient periods of ischemia on myocardial cells. Fine structure during the first few minutes of reflow. Am J Pathol 74:399
Leaf A (1973) Cell swelling: A factor in ischemic tissue injury. Circulation 48:455–458
Cobb FR, McHale PA, Rembert JC (1978) Effects of acute cellular injury on coronary vascular reactivity in awake dogs. Circulation 57:962–968
Hellstrom HR (1971) Coronary artery stasis after induced myocardial infarctions in the dog. Cardiovasc Res 5:371
Flameng W, Daenen W, Borgers M, Thoné F, Xhonneux R, Van de Water A, Van Belle H (1981) Cardioprotective effects of lidoflazine during 1-hour normothermic global ischemia. Circulation 64:796–807
Flameng W, Xhonneux R, Van Belle H, Borgers M, Van de Water A, Wynants J, Thoné F, Van Daele P, Janssen P (in press) Cardioprotective effects of mioflazine during one hour normothermic global ischemia in the canine heart. Cardiovasc Res
Van Belle H, Xhonneux R, Borgers M, Flameng W (1983) Cardioprotective effects of adenosine, lidoflazine and R51469. In: Berne RM, Rall TW, Rubio R (eds) Regulatory functions of adenosine. Martinus Nyhoff Publishers
Schaper W, Flameng W, Winkler B, Neugebauer G, Carl M, Pasyk S (1976) Quantification of collateral resistance in acute and chronic experimental coronary occlusion in the dog. Circ Res 39:371–377
Grayson JW, Irvine M, Parratt JR, Cunningham J (1968) Vasospastic elements in myocardial infarction following coronary occlusion in the dog. Cardiovasc Res 2:54
Flameng W: unpublished results
Willerson JT, Watson JT, Hutton I, Templeton GH, Fixler D (1975) Reduced myocardial reflow in increased coronary vascular resistance following myocardial ischemia in the dog. Circ Res 36:771–781
Humphrey SM, Seelye RN, Gavin JB (1982) The influence of adenosine on the no reflow phenomenon in anoxic and ischaemic hearts. Pharmacology 14:129–133
Humphrey SM, Seelye RN (1982) Improved functional recovery of ischemic myocardium by suppression of adenosine catabolism. J Thorac Cardiovasc Surg 84:16–22
Van Belle H (1970) The disappearance of adenosine in dog blood after low oral doses of lidoflazine (0.31–5 mg/kg). Europ J Pharm 10:290–292
Spieckermann PG, Fuchs C, Gehtmann JW, Knoll D, Kübler W, Bretschneider HJ (1972) Einfluß des Koronardilatators Lidoflazine auf den Adenosinstoffwechsel des Myocards während Ischämie und Anoxie. Arzneim Forsch (Drug Res) 22:1869–1874
Jageneau AHM, Schaper WKA, Van Gerven W (1969) Enhancement of coronary reactive hyperemia in unanaesthetized pigs by an adenosine-potentiator (lidoflazine). Naunyn-Schmiedebergs Arch Pharmak 265:16–23
Author information
Authors and Affiliations
Additional information
In part supported by a grant from I.W.O.N.L.
Rights and permissions
About this article
Cite this article
Flameng, W., Xhonneux, R., Vanhaecke, J. et al. Prevention of the “no reflow” phenomenon in the canine heart by mioflazine. Basic Res Cardiol 80, 27–36 (1985). https://doi.org/10.1007/BF01906741
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF01906741