Abstract
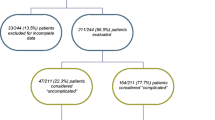
The aim of the study was to determine the possibility of establishing a genuine stress urinary incontinence severity grading from the combination of historical clinical and urodynamic parameters. Four hundred and eighty-three patients underwent complete investigation, including a questionnaire, clinical evaluation and multichannel urodynamic testing. They were then divided into four groups on the basis of the presence of only a SUI history (group 1,n=65); positive urine loss with a ‘continent’ stress urethral pressure profile (SUPP) (group 2,n=61); positive urine loss with an ‘incontinent’ SUPP (group 3,n=231); or no urine loss with an ‘incontinent' SUPP (group 4,n=126). Compared to group 1 the severity of incontinence was significantly greater in groups 2 and 3. and maximal urethral closure pressure and pressure transmission ratio were significantly reduced in group 3 and 4. Otherwise, history, clinical and urodynamic parameters showed no significant differences between the four groups. It was concluded that a scoring severity can be established when considering all the parameters of a woman suffering from GSI.
Similar content being viewed by others
References
Diokno AC, Brock BM, Brown MB et al. Prevalence of urinary incontinence and other urological symptoms in the non institutionalised elderly.J Urol 1986;136:1022–1025.
Hording U, Pedersen K, Sidenmius K et al. Urinary incontinence in 45-year-old women.Scand J Urol Nephrol 1986;20:183–187.
JC. Stress incontinence in nulliparous women.J Report Med 1969;2:96–99
Summit RL, Bent AE, Ostergard DR. The pathophysiology of genuine stress incontinence.Int Urogynecol J 1990;1:12–18
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence. The urogenital distress inventory and the incontinence impact questionnaire.Quality Life Res 1994;3:291–306.
Wyman JF, Harkins SW, Choi SC, Taylor JR, Fantl JA. Psychosocial impact of urinary incontinence in women.Obstet Gynecol 1987;70:378–381.
Uebersax JS, Wyman JF, Shumaker S, McClish DK, Fantl JA. Short form to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory.Neurourol Urodyn 1995;14:131–139
Ingelmann-Sundberg A. Urinary incontinence in women, excluding fistulae.Acta Obstet Gynecol Scand 1951;31:266–269
Crystle CD, Charme LS, Copeland WE. Q-Tip test in female urinary incontinence.Obstet Gynecol 1971;38:313–315
Montz FJ, Stanton SL. Q-Tip test in female urinary incontinence.Obstet Gynecol 1986;67:258–260
Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function recommended by the International Continence Society. Int Urogynecol J 1990;1:45–48
MacGuire EJ, Adult female urology. In Blaivas JG, Elbadawi A, McGuire EJ, Yalla SV, eds Neurourology and urodynamics, principles and pratice. New York: MacMillan 1988;264–273
Eberhard J. Die Integration de urodynamik im diagnostik und therapiekonzept der stressinkontinenz der Frau. Habilitationsschrift, Zürich 1988
Green TH. Urinary stress incontinence: differential diagnosis, pathophysiology and management.Am J Obstet Gynecol 1975;122:368–372
Blaivas JG. Pathophysiology of lower urinary tract dysfunction.Urol Clin North Am 1985;12:215–224
Blaivas JG. Pathophysiology of lower urinary tract dysfunction.Clin Obstet Gynecol 1985;12:295–309
Cardozo LD, Stanton SL. Genuine, stress incontinence and detrusor instability — a review of 200 patients,Br J Obstet Gynaecol 1980;87:184–190
Benson JT. Gynecologic and urodynamic evaluation of women with urinary incontinence.Obstet Gynecol 1985;66:691–694
Summit RL, Stovall TG, Bent AE, Ostergard DR. Urinary incontinence: correlation of history and brief office evaluation with multichannel urodynamic testing.Am J Obstet Gynecol 1992;166:1835–1840
Fischer-Rasmussen W, Hansen RI, Stage P. Predictive values of diagnostic tests in the evaluation of female stress urinary incontinence.Acta Obstet Gynecol Scand 1986;65:291–294
Hilton P, Stanton SL. Urethral pressure measurement by microtransducer: the results in symptom free women and in those with genuine stress incontinence.Br J Obstet Gynaecol 1983;90:919–933
Author information
Authors and Affiliations
Additional information
Editorial Comment: This article emphasizes that GSI is a complex phenomenon with multiple factors playing a role in the production of urine loss. Due to this multifactorial etiology there has been great difficulty in developing a grading system that can take all factors into account. Certainly there are other factors that we know nothing about at the present time that also play a role. This is an excellent attempt to categorize, patients into four groups based on a combination of historical, clinical and urodynamic findings. Further simplification may be necessary to allow its routine use in the clinical setting.
Rights and permissions
About this article
Cite this article
Meyer, S., de Grandi, P. & Caccia, G. The correlation between historical, clinical and urodynamic parameters in patients suffering from genuine stress urinary incontinence: Can a severity grading be considered?. Int Urogynecol J 6, 337–342 (1995). https://doi.org/10.1007/BF01892739
Issue Date:
DOI: https://doi.org/10.1007/BF01892739