Summary
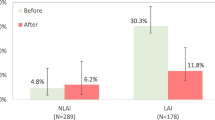
In 33 schizophrenic patients treated continuously as outpatients with perazine over two decades, the rehospitalization rate decreased from 0.58 before treatment to 0.07 during treatment. The intensity of psychopathologic symptoms and the side effects were found to be remarkably low. The high intraindividual constancy of perazine plasma levels and the tight correlation between dose and plasma levels indicated satisfactory patient compliance. Plasma levels amounted to only 25% of those under acute treatment and correlated positively with the severity of the disease. Higher plasma levels coincided with more frequent side effects such as slightly pathologic liver function and moderate impairment of oral glucose tolerance. The results suggest that low-dose maintenance treatment of schizophrenic patients with oral neuroleptics is effective and relatively safe.
Zusammenfassung
Bei 33 schizophrenen Patienten, die seit durchschnittlich 18 Jahren kontinuierlich ambulant mit Perazin behandelt wurden, sank die Rehospitalisierungsrate pro Jahr von 0,58 vor auf 0,07 während der Behandlung. Die Intensität der psychopathologischen Symptomatik sowie der Nebenwirkungen waren bemerkenswert gering. Die hohe intraindividuelle Konstanz der Perazin-Plasmaspiegels und die enge Korrelation zwischen Dosis und Plasmaspiegel sprach für eine befriedigende Compliance (Behandlungstreue) der Patienten. Die Höhe der Plasmaspiegel betrug nur etwa ein Viertel der Spiegel, die während einer Akutbehandlung gemessen werden, und sie korrelierte positiv mit der Schwere der Erkrankung. Je höher die Plasmaspiegel waren, desto häufiger waren Nebenwirkungen wie geringfügig pathologische Leberfunktion und eine mäßige Verschlechterung der oralen Glucosetoleranz.
Die Ergebnisse legen den Schluß nahe, daß eine niedrig dosierte Langzeitbehandlung schizophrener Patienten mit oralen Neuroleptika effektiv und relativ sicher ist.
Similar content being viewed by others
References
Affleck JW, Burns J, Forrest AD (1976) Long-term follow-up of schizophrenic patients in Edinburgh. Acta Psychiat Scand 53:227–237
Arbeitsgemeinschaft für Methodik und Dokumentation in der Psychiatrie (1979) Das AMDP- System; Manual zur Dokumentation psychiatrischer Befunde, 3. Auflage. Springer, Heidelberg Berlin New York
Axelsson R (1975) On the pharmacokinetics of thioridazine in psychiatric patients. In: Sedvall G et al. (eds) Antipsychotic drugs: Pharmacodynamics and pharmaco kinetics. Pergamon Press, Oxford, pp 353–358
Baumann U, Angst J (1975) Methodological development of the AMP-system. Neuropsychopharmacology Proc. IX. Cong CINP Paris 1974. Excerpta Medica, Amsterdam; American Elsevier Publishing Co, New York
Beard JH, Malamud TJ, Rossmann E (1978) Psychiatric rehabilitation and long-term rehospitalization rates: The findings of two research studies. Schizophr Bull 4:622–635
Bland RC, Parker JH, Orn H (1976) Prognosis in schizophrenia. A ten-year follow-up of first admissions. Arch Gen Psychiatry 33:949–954
Bland RC, Parker JH, Orn H (1978) Prognosis in schizophrenia. Prognostic predictors and outcome. Arch Gen Psychiatry 35:72–77
Bleuler M (1972) Die schizophrenen Geistesstörungen im Lichte langjähriger Kranken- und Familiengeschichten. Thieme, Stuttgart
Bosch G, Pietzcker A (1975) Nachbehandlung krankenhausentlassener schizophrener Patienten — Ergebnisse einer empirischen Untersuchung. Anhang zum Bericht der Lage der Psychiatrie in der Bundesrepublik Deutschland, S 344–360
Breyer U, Müller-Oerlinghausen B, Mauruschat W (1977) Phenothiazines with piperazine side chain. In: Forrest IS, Usdin E (eds) Psychotherapeutic drugs. Marcel Dekker, New York
Davis JM (1975) Overview: Maintenance therapy in psychiatry: I. Schizophrenia. Am J Psychiatry 132:1237–1245
Degkwitz R, Consbruch U, Haddenbrock S, Neusch B, Oehlert W, Unsöld R (1976) Therapeutische Risiken bei der Langzeitbehandlung mit Neuroleptika und Lithium. Nervenarzt 47:81–87
Dimroth G, Gebhardt R, Langer C, Müller-Oerlinghausen B, Renfordt E, Schley J (1980) The influence of anticholinergic medication on the state of well-being, psychomotoric performance, EPMS, and psychopathology of acute psychotic patients under neuroleptic treatment. Arzneim Forsch (Drug Res) 30:1202–1203
EDESG (1970) Report of the European Diabetes Epidemiology Study Group. Diabetologia 6:646–647
Giel R, Duk S, van Weerden-Dukstra JR (1978) Mortality in the long-stay population of all Dutch mental hospitals. Acta Psychiat Scand 57:361–368
Gonçalves N (1978) „Schwund“ bei ambulant behandelten Schizophrenen. Nervenarzt 49:58–64
Goncalves N, Grüneberg F (1975) Einseitige orale Glukosebelastung bei langfristig neuroleptisch behandelten Schizophrenen. Pharmakopsychiatrie 8:289–295
Hansen LB, Larsen NE (1977) Plasma concentrations of perphenazine and its sulphoxide metabolite during continuous oral treatment. Psychopharmacology 53:127–130
Helmchen H (1978) Forschungsaufgaben bei psychiatrischer Langzeitmedikation. Nervenarzt 49:534–538
Helmchen H, Hippius H, Tiling P (1967) Die Zusammenarbeit von Klinik und Praxis bei der langfristigen medikamentösen Behandlung von Psychose-Kranken. Internist 9:328–331
Hippius H, Selbach H (1961) Zur medikamentösen Dauertherapie bei Psychosen. Neuropsychopharmakologie, 2. Symposium, Nürnberg 1961. Med Exp 5:298–305
Hippius H, Tiling P (1967) Möglichkeiten einer Zusammenarbeit von Klinik und Praxis bei medikamentöser Dauertherapie klinikentlassener psychotischer Kranken. In: Heinrich K (ed) Der entlassene Anstaltspatient in der psychiatrischen Rehabilitation. Alma-Mater, Konstanz
Hogarty GE, Goldberg SC, Schooler NR, Ulrich RF (1974) Drug and sociotherapy in the aftercare of schizophrenic patients: Two-year relapse rates. Arch Gen Psychiatry 31:603–608
Hogarty GE, Ulrich RF, Mussare F, Arishgueta N (1976) Drug discontinuation among long term, successfully maintained schizophrenic outpatient. Dis Nerv Syst 37:494–500
Köbberling J, Creutzfeldt W (1970) Comparison of different methods for the evaluation of the oral glucose tolerance test. Diabetes 19:870–877
Levine J, Schooler NR, Cassano GB (1979) The role of depot neuroleptics in the treatment of schizophrenic patients. Psychol Med 9:383–386
Linden M (in press) Definition of compliance. Int J Clin Pharmacol Biopharm
Lonowski DJ, Sterling FE, Kennedy JC (1978) Gradual reduction of neuroleptic drugs among chronic schizophrenics. A double-blind controlled study. Acta Psychiat Scand 57:97–102
March JE, Donato D, Turano P, Turner WJ (1972) Interpatient variation and significance of plasma levels of chlorpromazine in psychotic patients. J Med 3:146–162
Müller P, Kind J, Lohrengel S, Steuber H, Hartmann W, Jung F, Pudel V (1977) Die neuroleptische Rezidivprophylaxe schizophrener Psychosen. Vorläufige Mitteilung. Nervenarzt 48:560–561
Müller-Oerlinghausen B (1980a) Antipsychotics. (Clinical pharmacology—pharmacokinetics) In: Hoffmeister F, Stille G (eds) Handbook of experimental pharmacology. Vol: Psychotropic agents; Part: Antipsychotics and antidepressants. Springer, Berlin Heidelberg New York, pp 267–285
Müller-Oerlinghausen B (1980b) Schäden nach langfristiger Behandlung mit Psychopharmaka. AMI-Bericht I/1980, Berlin
Müller-Oerlinghausen B, Passoth PM, Poser W, Pudel V (1979) Impaired glucose tolerance in long-term lithium-treated patients. Int Pharmacopsychiatry 14:350–362
Müller-Oerlinghausen B, Passoth PM, Poser W, Schlecht W (1978 Zum Einfluß langfristiger Behandlung mit Neuroleptika oder Lithiumsalzen auf den Kohlenhydratstoffwechsel. Arzneim Forsch (Drug Res) 28:1522–1524
Müller-Oerlinghausen B, Riedel R, Schley J (1977) TLC and GLC procedures for the determination of perazine and its metabolites in human body fluids. Int J Clin Pharmacol 15: 366–372
Muusze RG, Vanderheeren FA (1977) Plasma levels and half lives of thioridazine and some of its metabolites. II. Low doses in older psychiatric patients. Eur J Clin Pharmacol 11:141–147
Pietzcker A, Gebhardt R, Freudenthal K (1977) Ein vergleich nosologisch-diagnostischer mit cluster-analytisch gefundenen Gruppen anhand AMP-dokumentierter psychopathologischer Befunde. Nervenarzt 48:276–282
Pietzcker A (1978) Langzeitmedikation bei schizophrenen Kranken. Nervenarzt 49:518–533
Rifkin A, Quitkin F, Rabiner CJ, Klein DF (1977) Fluphenazine decanoate, fluphenazine hydrochloride given orally and placebo in remitted schizophrenics. I. Relapse rates after one year. Arch Gen Psychiatry 34:43–47
Scharfetter Ch (1971) Das AMP-System. Manual zur Dokumentation psychiatrischer Befunde. Springer, Berlin Heidelberg New York
Schley J, Riedel F, Müller-Oerlinghausen B (1978) Determination of perazine (Taxilan®) serum levels by GLC under clinical routine conditions. J Chem Clin Biochem 16:307–311
Schwalb H, Hanika R, Meier G, Gruber E, Reinhold H (1974) Kardiologische Risikofaktoren bei Patienten eines Psychiatrischen Krankenhauses. Nervenarzt 45:544–547
Serban G, Thomas A (1974) Attitudes and behaviors of acute and chronic schizophrenic patients regarding ambulatory treatment. Am J Psychiatry 131:991–995
Stephens JH, Astrup Ch (1963) Prognosis in “Process” and “Non-Process” schizophrenia. Am J Psychiatry 119:945–953
Stephens JH (1978) Long-term prognosis and follow-up in schizophrenia. Schizophr Bull 4: 25–47
Strauss JS, Carpenter WT Jr (1974) The prediction of outcome in schizophrenia. II. Relationship between predictor and outcome variables: A report from the WHO international pilot study of schizophrenia. Arch Gen Psychiatry 31:37–42
Strauss JS, Carpenter WT (1977) Prediction of outcome in schizophrenia. III. Five-year out-come and its predictors. Arch Gen Psychiatry 34:159–163
Studer E, Cikes M, Widmer LK (1969) Blutzucker und Alter. Beobachtungen an 1060 Männern in der Basler Studie II. Dtsch Med Wochenschr 94:1179–1182
Wiles DH, Kolakowska T, McNeilly AS, Mandelbrote BM, Gelder MG (1976) Clinical significance of plasma chlorpromazine levels. I. Plasma levels of the drug, some of its metabolites and prolactin during acute treatment. Psychol Med 6:407–415
Woggon B, Angst J, Margoses N (1975) Gegenwärtiger Stand der neuroleptischen Langzeit-behandlung der Schizophrenie. Nervenarzt 46:611–616
Author information
Authors and Affiliations
Additional information
Supported by Deutsche Forschungsgemeinschaft, Bonn-Bad-Godesberg (He 916/2 Clinical Pharmacology)
Rights and permissions
About this article
Cite this article
Pietzcker, A., Poppenberg, A., Schley, J. et al. Outcome and risks of ultra-long-term treatment with an oral neuroleptic drug. Arch. F. Psychiatr. U. Z. Neur. 229, 315–329 (1981). https://doi.org/10.1007/BF01833160
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF01833160