Summary
We have examined the behavior of several variables which are related to respiratory control in 114 infants (up to 6 months of age) in order to assess the risk for the sudden infant death syndrome (SIDS). 23 of the infants had already had demonstrable serious or life threatening apneas or respiratory problems during surgical anesthesia. These infants were assigned as a risk group, and the rest of the investigated babies was taken as a control group.
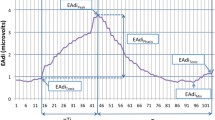
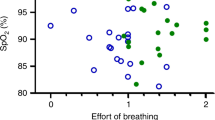
We found that practically all infants of the risk group had apneas during sleep, which lasted longer than 8 s each. Only 22% of the infants of the control group had apneas of such a duration. As a statistical parameter, calculated from at least 1 hour recording of respiration, we defined the mean apnea duration (MA-value) as average value of apnea duration time in seconds per minute of recording. The MA-value proved to be significantly elevated in the infants of the risk group. The trend to hypoxia in the infants of the risk group was also indicated by the observation of lower transcutaneous\(P_{O_2 } \)-values (tc-\(P_{O_2 } \)) during sleep, when compared with control infants. In agreement with this observation is the increase of the 2,3-DPG concentration and the decrease of the density of erythrocytes of the infants of the risk group.
Breathing hypoxic gas mixtures tended to depress respiration in all infants tested, and, especially in the risk group, to elicit irregular respiratory patterns. On the other hand, we observed that inhalation of pure oxygen markedly stimulated respiration in all infants investigated.
We conclude from these observations that a risk for SIDS may be related to a particular response pattern of the respiratory center during the early postnatal life. We are able to distinguish infants with a higher risk for SIDS from other children by determination of the MA-value during sleep.
Zusammenfassung
Wir untersuchten das Verhalten verschiedener Variabler, die mit der Atemregulation bei Säuglingen bis zu einem Alter von 6 Monaten in Verbindung stehen, um ein eventuelles Risiko für das Auftreten eines SIDS-Ereignisses (sudden infant death syndrome) identifizieren zu können. Bei 23 von insgesamt 114 untersuchten Säuglingen waren bereits ernste oder lebensbedrohende Apnoeanfälle während chirurgischer Eingriffe unter Narkose beobachtet worden. Diese Babies wurden als Risikogruppe bezeichnet, während die restlichen untersuchten Säuglinge als Kontrollgruppe galten.
Wir konnten zeigen, daß praktisch alle Risikosäuglinge Apnoen während des Schlafes hatten, die eine Länge von 8 s überschritten. Lediglich 22% aller Kontrollsäuglinge hatten Apnoen dieser Länge. Von den aufgezeichneten Atemkurven berechneten wir als statistischen Parameter den mittleren Atemsausfall in s pro min (MA-Wert). Dieser MA-Wert war bei der Risikogruppe im Vergleich mit der Kontrollgruppe statistisch signifikant erhöht. Durch kontinuierliche Aufzeichnungen der transkutanen\(P_{O_2 } \)-Werte konnte darüber hinaus noch gezeigt werden, daß die Babies der Risikogruppe zu einer Hypoxämie während des Schlafes neigen. Übereinstimmend mit dieser Beobachtung ist auch der Anstieg der 2,3-DPG-Konzentration und der Abfall der Dichte der Erythrocyten bei Risikosäuglingen. Verabreichung leicht hypoxischer Gasgemische führte besonders bei der Risikogruppe
Similar content being viewed by others
References
Albersheim S, Boychuk R, Seshia MMK, Cates D, Rigatto H (1976) Effects of CO2 on immediate ventilatory response to O2 in preterm infants. J Appl Physiol 41:609–611
Avery ME, Frantz ID (1977) To breathe or not to breathe. N Engl J Med 297:781–782
Bednarek FJ, Roloff DW (1976) Treatment of apnea of prematurity with aminophylline. Pediatrics 58:335–339
Bergmann AB, Beckwith JB, Ray CG (1970) Sudden infant death in Copenhagen 1956–1971. II. Social factors and morbidiference on causes of sudden death in infants. University of Washington Press, Seattle
Biering-Sørensen F, Jørgensen T, Hilden J (1979) Sudden infant death in Copenhagen 1956–1971. II. Spcial factors and morbidity. Acta Paediatr Scand 68:1–9
Brady JP, Ariagno RL, Watts JL, Goldman SL, Dumpit FM (1978) Apnea, hypoxemia, and aborted sudden infant death syndrome. Pediatrics 62:686–691
Bryan AC, Bryan MH (1978) Control of respiration in the newborn. Clin Perinatol 5:269–281
Carpenter RG, Gardner A, McWeeny PM, Emery JL (1977) Multistage scoring system for identifying infants at risk of unexpected death. Arch Dis Childh 52:606–612
Cornwell AC, Weitzman ED, Marmarou A (1978) Ambulatory and in-hospital continuous recording of sleep state and cardiorespiratory parameters in “near miss” for the sudden infant death syndrome and control infants. Biotelemetry 5:113–122
Davi MJ, Sankaran K, Simons KJ, Simons FER, Seshia MM, Rigatto H (1978) Physiologic changes induced by theophylline in the treatment of apnea in preterm infants. J Pediatr 92:91–95
Davi M, Sankaran K, MacCallum M, Cates D, Rigatto H (1979) Effect of sleep state on chest distortion and on the ventilatory response to CO2 in neonates. Pediatr Res 13:982–986
Frisch H, Mueller W, Irnberger E (1978) Apnoeprophylaxe bei Frühgeborenen mit Theophyllin. Mschr Kinderheilkd 126:684–686
Gabriel M, Albani M, Schulte FJ (1976) Apneic spells and sleep states in preterm infants. Pediatrics 57:142–147
Gabriel M, Witolla C, Albani M (1978) Sleep and aminophylline treatment of apnea in preterm infants. Eur J Pediat 128:145–149
Gerhardt T, McCarthy J, Bancalari E (1978) Aminophylline therapy for idiopathic apnea in premature infants: effects on lung function. Pediatrics 62:801–804
Gerhardt T, McCarthy J, Bancalari E (1979) Effect of aminophylline on respiratory center activity and metabolic rate in premature infants with idiopathic apnea. Pediatrics 63:537–542
Giacoia G, Jusko WJ, Menke J, Koup JR (1976) Theophylline pharmacokinetics in premature infants with apnea. J Pediatr 89:829–832
Guilleminault C, Peraita R, Souquet M, Dement WC (1975) Apneas during sleep in infants: Possible relationships with sudden infant death syndrome. Science 190:677–679
Guilleminault C, Ariagno RL, Forno LS, Nagel L, Baldwin R, Owen M (1979) Obstructive sleep apnea and near miss for SIDS: I. Report of an infant with sudden death. Pediatrics 63:837–843
Guthrie RD, Standaert TA, Hodson WA, Woodrum DE (1980) Sleep and maturation of eucapnic ventilation and CO2 sensitivity in the premature primate. J Appl Physiol 48:347–354
Haidmayer R, Kurz R, Kenner T (1979) Zum Problem des plötzlichen Kindestodes. Wien Med Wochenschr 129:201–207
Haidmayer R, Kenner T, Kurz R (1980) Verschiebung der Dichteverteilung von Erythrocyten bei Säuglingen mit Atemregulationsstörungen. Paediat Paedol 15:47–52
Jørgensen T, Biering-Sørensen F, Hilden J (1979) Sudden infant death in Copenhagen 1956–1971. III. Perinatal and perimortal factors. Acta Paediatr Scand 68:11–22
Kuzemko JA, Paala J (1973) Apnoeic attacks in the newborn treated with aminophylline. Arch Dis Childh 48:404–406
Latini R, Assael BM, Bonati M, Caccamo ML, Gerna M, Mandelli M, Marini A, Sereni F, Tognoni G (1978) Kinetics and efficacy of theophylline in the treatment of apnea in the premature newborn. Eur J Clin Pharmacol 13:203–207
Lewak N, Van den Berg BJ, Beckwith JB (1979) Sudden infant death syndrome risk factors. Prospective data review. Clin Pediatr 18:404–411
Naeye RL (1973) Pulmonary arterial abnormalities in the sudden infant death syndrome. N Engl J Med 289:1167–1170
Naeye RL (1974) Hypoxemia and the sudden infant death syndrome. Science 186:837–838
Naeye RL (1977) The sudden infant death syndrome. A review of recent advances. Arch Pathol Lab Med 101:165–167
Plouin P, Monod N, Chabrolle JP, Lerique A (1978) Troubles respiratoires et hypothyroidie post-natale. Étude polygraphique d'une observation. Rev EEG Neurophysiol 8:321–325
Purcell M (1976) Response in the newborn to raised upper airway resistance. Arch Dis Childh 51:602–607
Rigatto H, Brady JP (1972) Periodic breathing and apnea in preterm infants. II. Hypoxia as a primary event. Pediatrics 50:219–228
Rigatto H, de la Torre Verduzco R, Cates DB (1975) Effects of O2 on the ventilatory response to CO2 in preterm infants. J Appl Physiol 39:896–899
Rigatto H, Brady JP, de la Torre Verduzco R (1975) Chemoreceptor reflexes in preterm infants. I. The effect of gestational and postnatal age on the ventilatory response to inhalation of 100% and 15% oxygen. Pediatrics 55:604–613
Rigatto H (1977) Respiratory control and apnea in the newborn infant. Crit Care Med 5:2–9
Sankaran K, Wiebe H, Seshia MMK, Boychuk RB, Cates D, Rigatto H (1979) Immediate and late ventilatory response to high and low O2 in preterm infants and adult subjects. Pediatr Res 13:875–878
Schiffman PL, Westlake RE, Santiago TV, Edelman NH (1980) Ventilatory control in parents of victims of sudden infant death syndrome. N Engl J Med 302:486–491
Shannon DC, Kelly DH, O'Connell K (1977) Abnormal regulation of ventilation in infants at risk for sudden infant death syndrome. N Engl J Med 297:747–750
Shannon DC, Kelly DH (1978) Abnormal ventilatory response to CO2 during quiet sleep in aborted SIDS. Chest 73 [Suppl]:301
Steinschneider A (1972) Prolonged apnea and the sudden infant death syndrome: clinical and laboratory observations. Pediatrics 50:646–654
Valdes-Dapena MA (1967) Sudden and unexpected death in infancy: a review of the world literature 1954–1966. Pediatrics 39:123–138
Valdes-Dapena MA (1970) Progress in sudden infant death research, 1963–69. In: Bergmann AB, Beckwith JB, Ray CG (eds) Proceedings of the Second International Conference on Causes of Sudden Death in Infants. University of Washington Press, Seattle, pp 3–13
Valdes-Dapena MA (1977) Sudden unexplained infant death, 1970 through 1975. An evolution in understanding. Pathol Ann 12:117–145
Williams A, Vawter G, Reid L (1979) Increased muscularity of the pulmonary circulation in victims of sudden infant death syndrome. Pediatrics 63:18–23
Author information
Authors and Affiliations
Additional information
This study was supported by the Austrian Research Fund zu einer Atemdepression sowie auch zum Auftreten unregelmäßiger Atemmuster. Andererseits aber konnten wir den interessanten Befund erheben, daß reiner Sauerstoff bei allen Säuglingen zu einer Atemstimulation beitrug.
Aus unseren Beobachtungen schließen wir, daß ein Risiko für das SIDS möglicherweise im Zusammenhang mit bestimmten Antwortmustern des Atemzentrums während des frühen postnatalen Lebens steht. Wir können nun zwischen Kindern mit einem hohen und einem geringeren Risiko für das SIDS unterscheiden, indem wir ihre MA-Werte während des Schlafes bestimmen.
Rights and permissions
About this article
Cite this article
Haidmayer, R., Kurz, R., Kenner, T. et al. Physiological and clinical aspects of respiration control in infants with relation to the sudden infant death syndrome. Klin Wochenschr 60, 9–18 (1982). https://doi.org/10.1007/BF01721582
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01721582