Abstract
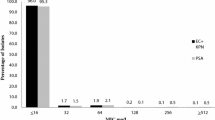
As part of the Artemis project, 11 500 isolates (3000 from patients with respiratory tract infections) were collected throughout six European countries between 1994 and 1996. Twenty-seven hospitals or laboratories participated in this first phase of the study. The activities of three classes of antimicrobial agents (fluor-oquinolones,β-lactam agents, macrolides) are presented for the six most frequently isolated pathogens (Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, Pseudomonas aeruginosa, Klebsiella pneumoniae). Overall, trovafloxacin and ciprofloxacin activities were similar forHaemophilus influenzae, Moraxella catarrhalis andKlebsiella pneumoniae isolates. Of theStreptococcus pneumoniae isolates, 6% were resistant to penicillin. Trovafloxacin had the highest activity against theStreptococcus pneumoniae isolates, with a minimum inhibitory concentration of 0.25 mg/l for 90% of isolates (MIC90); all strains tested were susceptible to trovafloxacin. The MIC90 of ciprofloxacin forStreptococcus pneumoniae was 3 mg/l, and overall 52% of the strains were susceptible; 9% were resistant. Azithromycin and clarithromycin exhibited similar activity against all collected pathogens, exceptHaemophilus influenzae. All strains ofHaemophilus influenzae were susceptible to azithromycin compared with 79% for clarithromycin, with respective MIC90s of 2 and 16 mg/l. The data presented demonstrate differences in the susceptibility patterns of six major respiratory tract pathogens in Europe.
Similar content being viewed by others
References
Perlman PE, Ginn DR: Respiratory infections in ambulatory adults: choosing the best treatment — respiratory tract infections. Postgraduate Medicine (1990) 87:175–184
Spencer RC: Predominant pathogens found in the European prevalence of infection in intensive care study. European Journal of Clinical Microbiology & Infectious Diseases (1996) 15:281–285
Niederman MS, Campbell GD, Fein AM, Grossman RF, Mandell LA, Marrie TJ, Sarosi GA, Torres A, Yu V: Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. American Reviews of Respiratory Disease (1993) 148:1418–1426
Chow AW, Hall CB, Klein JO, Kammer RB, Meyer RD, Remington JS: General guidelines for the evaluation of new anti-infective drugs for the treatment of respiratory tract infections. Clinical Infectious Diseases (1992) 15, Supplement: 62–88
Fraimow HS, Abrutyn E: Pathogens resistant to antimicrobial agents — epidemiology, molecular mechanisms, and clinical management. Infectious Disease Clinics of North America (1995) 9:497–530
Friedland IR, McCracken GH Jr: Management of infections caused by antibiotic-resistantStreptococcus pneumoniae. New England Journal of Medicine (1994) 331:377–382
Felmingham D, Grüneberg RN, the Alexander Project Group: A multicentre collaborative study of the antimicrobial susceptibility of community-acquired, lower respiratory tract pathogens 1992–1993: the Alexander Project. Journal of Antimicrobial Chemotherapy (1996) 38. Supplement A: 1–57
Baquero F, the Task Force of the General Direction for Health Planning of the Spanish Ministry of Health: Antibiotic resistance in Spain: what can be done? Clinical Infectious Diseases (1996) 23:819–823
Centers for Disease Control: Defining the public health impact of drug-resistantStreptococcus pneumoniae: report of a working group. 45/RR1. Morbidity and Mortality Weekly Report (1996) 45:1–13
National Committee for Clinical Laboratory Standards: Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A4, NCCLS, Villanova, PA (1995)
Klugman KP: Pneumococcal resistance to antibiotics. Clinical Microbiology Review (1990) 3:171–196
Schito GC, Mannelli S, Pesce A, the Alexander Project Group: Trends in the activity of macrolides and β-lactam antibiotics and resistance development. Journal of Chemotherapy (1997) 9, Supplement 3:18–28
Breiman RF, Butler JC, Tenover FC, Elliott JA, Facklan RR: Emergence of drug-resistant pneumococcal infections in the United States. Journal of American Medical Association (1994) 271:1831–1835
Mulligan ME, Murrary-Leisure KA, Ribner BS, Standifor HC, John JF, Korvick JA, Kauffman CA, Yu VL: Methicillin-resistantStaphylococcus aureus: a consensus review of the microbiology, pathogenesis and epidemiology with implication for prevention and management. American Journal of Medicine (1993) 94:313–328
Lyon RR, Skurray R: Antimicrobial resistance ofStaphylococcus aureus: genetic basis. Microbiological Reviews (1987) 117:390–398
Daum TE, Schaberg DR, Tenpenning MS, Sottile WS, Kauffman CA: Increasing resistance ofStaphylococcus aureus to ciprofloxacin. Antimicrobial Agents and Chemotherapy (1990) 34:1862–1863
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pontani, D., Washton, H., Bouchillon, S. et al. Susceptibility of European respiratory tract isolates to trovafloxacin, ciprofloxacin, clarithromycin, azithromycin and ampicillin. Eur. J. Clin. Microbiol. Infect. Dis. 17, 413–419 (1998). https://doi.org/10.1007/BF01691574
Issue Date:
DOI: https://doi.org/10.1007/BF01691574