Abstract
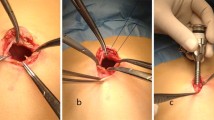
From 1981 to 1987, a total of 40 cirrhotic patients with umbilical hernia were treated either by conventional herniorrhaphy (26) or by herniorrhaphy and concomitant insertion of a peritoneovenous (PV) shunt (14). The aim of concomitant PV shunt insertion was to reduce postoperative complications of herniorrhaphy in those patients with intractable ascites, or in whom difficulty to control postoperative ascites was contemplated. In the group of patients with PV shunt, 8 were class B and 6 were class C according to Child's classification; 7 patients had complicated hernia including 2 patients with skin ulceration, 4 with rupture, and 1 with incarceration. In the group with standard herniorrhaphy, 5 patients were class A and 21 were class B; 13 patients were operated on electively for uncomplicated hernia without ascites, 6 had incarceration, and 7 had skin ulceration. The technical procedure of concomitant PV shunting and hernia repair included: insertion of the valve, surgical repair of the hernia, and insertion of the venous tube. In that order, in-hospital mortality was nil. Postoperative complications included sepsis in 2 patients who had concomitant insertion of a PV shunt, and massive ascitic fluid production in 5 patients treated by conventional herniorrhaphy, resulting in ascitic leak from the surgical wound in 1 case. Recurrence of the hernia was observed in 6 patients treated by conventional herniorrhaphy, and in none who had a patent PV shunt. We conclude that concomitant insertion of a PV shunt should be considered in cirrhotic patients whose ascites does not respond to medical treatment or in patients with complicated hernia requiring an emergency procedure in whom poor liver function anticipates difficult management of postoperative ascites.
Résumé
Entre 1981 et 1987, 40 patients cirrhotiques porteurs d'une hernie ombilicale (HO) ont été traités soit par une réparation pariétale classique seule (RG) (26 cas), soit par une RC associée à une insertion concommitante de valve de Le Veen (VL) (14 cas). Le but du traitement associé (RC+VL) était de tenter de réduire le taux de complications post-opératoires observées chez les patients ayant une ascite réfractaire ou chez qui une aggravation post-opératoire était à craindre. La gravité de la cirrhose a été évaluée selon la classification de Child. Dans le group RC, 5 patients étaient de classe A et 21 patients de classe B. Dans 13 cas, l'intervention a été pratiquée en urgence pour une complication locale de la hernie: engouement ou étranglement herniaire (6 cas), lésions cutanées (7 cas). Les 13 autres patients ont été opérés à froid de leur HO non compliquée sans ascite. Dans le groupe RC+VL, 8 patients étaient de classe B et 6 patients de classe C. Sept patients avaient une HO compliquée: engouement (1 cas), rupture de HO (4 cas), lésions cutanées (2 cas). Dans ce groupe, l'ordre des étapes chirurgicales était toujours le même: insertion de la valve, réparation pariétale et insertion du tube veineux. La mortalité hospitalière s'est avérée nulle. Les complications postopératoires observées étaient un sepsis chez 2 patients dans le groupe VL et une production massive d'ascite chez 5 patients dans le groupe RC (1 de ces patients avait une fuite de la plaie chirurgicale). On a observé une récidive chez 6 patients traités par RC et aucune chez les patients traités par RC+VL lorsque la VL était toujours perméable. Nous concluons que, chez le patient cirrhotique porteur d'une hernie ombilicale, à fonction hépatique détériorée et chez lequel on peut craindre une aggravation postopératoire, il faut envisager l'insertion d'une VL associée à la cure pariétale si l'ascite est réfractaire ou si une complication herniaire nécessite une réparation en urgence.
Resumen
Cuarenta pacientes cirróticos que presentaban hernia umbilical fueron tratados mediante herniorrafia convencional (26) o mediante herniorrafia con la inserción simultánea de un “shunt” peritoneovenoso (14). El propósito de insertar simultáneamente el “shunt” fue el de reducir las complicaciones postoperatorias de la herniorrafia en los pacientes con ascitis intratable, o en aquellos en que se preveía un dificil control postoperatorio de la ascitis. En el grupo de pacientes con el “shunt” PV, 8 fueron clase B y 6 clase C, según la clasificación de Child; 7 exhibían una hernia complicada, incluyendo 2 con ulceración de la piel, 4 con ruptura, y uno con incarceración. En el grupo sometido a herniorrafia estándar, 5 eran clase A y 21 clase B; 13 pacientes fueron operados en forma electiva por la presencia de una hernia no complicada sin ascitis, 6 presentaban incarceración y 7 ulceración de la piel. El procedimiento para la inserción del “shunt” PV y la reparación simultánea de la hernia incluyó los siguientes pasos: inserción extraperitoneal de la válvula, reparación quirúrgica de la hernia e inserción del tubo venoso. La mortalidad hospitalaria fue nula. Complicaciones postoperatorias incluyeron sepsis en 2 pacientes sometidos al procedimiento simultáneo y producción masiva de ascitis en 5 casos sometidos a herniorrafia convencional, lo cual resultó en escape del líquido ascítico a través de la incisión quirúrgica en uno. Se observó recurrencia de la hernia en 6 pacientes tratados mediante herniorrafia convencional, pero en ninguno de aquellos con un “shunt” permeable. Nuestra conclusion es que la inserción simultánea de un “shunt” PV debe ser considerada en los pacientes cirróticos con ascitis que no responda al tratamiento médico o en pacientes con una hernia complicada que requiera una operación de emergencia y en quienes una mala función hepática haga preveer un dificil manejo postoperatorio de la ascitis.
Similar content being viewed by others
References
Chapman, C.B., Snell, A.M., Rowntree, L.G.: Decompensated portal cirrhosis. Report of 112 cases. J. Am. Med. Assoc.97:237, 1931
Franco, D., Charra, M., Jeambrun, P., Belghiti, J., Cortesse, A., Sossier, C., Bismuth, H.: Nutrition and immunity after peritoneovenous drainage of intractable ascites in cirrhotic patients. Am. J. Surg.146:652, 1983
Leonetti, J.P., Aranha, G.V., Wilkinson, W.A., Stanley, M., Greenlee, H.B.: Umbilical herniorrhaphy in cirrhotic patients. Arch. Surg.119:442, 1984
O'Hara, E.T., Oliai, A., Patek, A.J., Nabseth, D.C.: Management of umbilical hernias associated with hepatic cirrhosis and ascites. Ann. Surg.181:85, 1975
Yonemoto, R.H., Davidson, C.S.: Herniorrhaphy in cirrhosis of the liver with ascites. N. Engl. J. Med.255:733, 1956
Biagini, J.R., Belghiti, J., Fékété, F.: Prevention of coagulopathy after placement of peritoneovenous shunt with replacement of ascitic fluid by normal saline solution. Surg. Gynecol. Obstet.163:315, 1986
Lemmer, J.H., Strodel, W.E., Knol, J.A., Eckhauser, F.E.: Management of spontaneous umbilical hernia disruption in the cirrhotic patient. Ann. Surg.198:30, 1983
Baron, H.C.: Umbilical hernia secondary to cirrhosis of the liver. Complications of surgical correction. N. Engl. J. Med.263:824, 1960
Pescovitz, M.D.: Umbilical hernia repair in patients with cirrhosis. No evidence for increased incidence of variceal bleeding. Ann. Surg.199:325, 1984
O'Connor, M., Allen, J.I., Schwartz, M.L.: Peritoneous shunt therapy for leaking ascites in the cirrhotic patient. Ann. Surg.200:66, 1984
Eisenstadt, S.: Symptomatic umbilical hernias after peritoneovenous shunts. Arch. Surg.114:1443, 1979
Lemmer, J.H., Strodel, W.E., Eckhauser, F.E.: Umbilical hernia incarceration: A complication of medical therapy of ascites. Am. J. Gastroenterol.78:295, 1983
Belghiti, J., Rueff, B., Fékété, F.: Umbilical hernia in cirrhotic patients with ascites. Prevalence, course and management. Gastroenterology84:1363 A, 1983
Aranha, G.V., Greenlee, H.B.: Intra-abdominal surgery in patients with advance cirrhosis. Arch. Surg.121:275, 1986
Garrison, R.N., Cryer, H.M., Howard, D.A., Polk, H.C.: Clarification of risk factors for abdominal operations in patients with hepatic cirrhosis. Ann. Surg.199:648, 1984
Doberneck, R.C., Sterling, W.A., Allison, D.C.: Morbidity and mortality after operation in nonbleeding cirrhotic patients. Am. J. Surg.146:306, 1983
Fékété, F., Belghiti, J., Cherqui, D., Langonnet, F., Gayet, B.: Results of esophagogastrectomy for carcinoma in cirrhotic patients. A series of 23 consecutive patients. Ann. Surg.206:74, 1987
Greenlee, H.B., Stanley, M.M., Reinhardt, G.F.: Intractable ascites treated with peritoneovenous shunts. Arch. Surg.116:518, 1981
Prokesch, R.C., Rimland, D.: Infectious complications of the peritoneovenous shunt. Am. J. Gastroenterol.78:235, 1983
Fulenwinder, J.T., Smith, R.B., Redd, S.C., Ansley, J.D., Henderson, J.M., Millikan, W.F., Galambos, J.T., Warren, W.D.: Peritoneovenous shunts. Lessons learned from an eight-year experience with 70 patients. Arch. Surg.119:1133, 1984
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Belghiti, J., Desgrandchamps, F., Farges, O. et al. Herniorrhaphy and concomitant peritoneovenous shunting in cirrhotic patients with umbilical hernia. World J. Surg. 14, 242–246 (1990). https://doi.org/10.1007/BF01664882
Issue Date:
DOI: https://doi.org/10.1007/BF01664882