Abstract
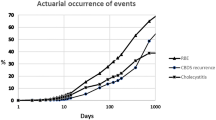
During 7057 conventional cholecystectomies (1972–1991), 16 bile duct injuries occurred, amounting to a risk of 0.22%. A total of 1022 laparoscopic cholecystectomies were performed without such a complication since April 1990. In a retrospective study, 64 patients (16 of our patients and 48 referrals) with an injury or stricture due to conventional cholecystectomy were investigated. In 14 of our 16 patients the injury was recognized and immediately repaired with a good long-term result of 93%, including one successful repair of a subsequent stricture. Two cases of unrecognized injury were managed by nonoperative means. The group of 48 referred patients comprised 10 early postoperative complications (21%) and 38 strictures after an “uneventful” cholecystectomy. Of the 64 total patients, 10 (16%) underwent nonoperative treatment, and 54 required surgery. The mean follow-up period after surgery was 7.4 ±4.9 years. Most cases (93%) were repaired by bilioenteric anastomosis (i.e., foremost hepaticojejunostomy) with an 18% restricture rate. Including second and third repairs for restricture, a total of 60 operations (14 primary and 46 secondary reconstructions) were performed without hospital mortality. A good long-term result after stricture repair was achieved in 75% of the patients, whereas 17% had a poor outcome owing to restricture or death (10% had related mortality within 10 years). The other 8% had a moderate result due to recurrent cholangitis. Thus immediate repair of a bile duct injury offers the better chance of a favorable prognosis compared to secondary stricture repair.
Résumé
Parmi 7057 cholécystectomies traditionnelles réalisées entre 1972 et 1991, on a enregistré 16 lésions de la voie biliaire principale, ce qui représente un risque de 0.22%. Depuis le mois d'avril 1990, on a réalisé 1022 cholécystectomies sous coelioscopie, sans observer un seul de ces accidents. Nous avons analysé rétrospectivement les dossiers de 64 patients ayant une lésion ou une sténose secondaire à une cholécystectomie traditionnelle. Chez 14 de ces 16 observations personnelles, la lésion a été reconnue pendant l'intervention et a été réparée immédiatement avec un résultat à long terme satisfaisant chez 93% de ces patients; un de ces patients a dû être opéré deux fois. Chez deux patients ayant une lésion non reconnue pendant l'intervention, le traitement a été conservateur. Parmi les 48 patients vus en seconde main, il y avait 10 patients ayant une lésion récente, apparue dans les suites immédiates d'une intervention (21%) et 38 sténoses apparues dans les suites d'une cholécystectomie “non compliquée”. Seulement 10 patients (16%) ont été traités de facon conservatrice alors que 54 patients ont nécessité une réparation chirurgicale. Le suivi moyen a été de 7.4 ±4.9 ans. La plupart des cas (93%) ont été réparés par une anastomose bilio-intestinale, le plus souvent des anastomoses hépatico-jéjunales, avec un taux de resténose de 18%. En incluant les réparations secondaires et tertiaires, un total de 60 interventions (14 reconstructions primitives et 46 reconstructions secondaires) ont été pratiquées, sans aucune mortalité. Les résultats à long terme après réparation biliaire étaient considérés comme des succès chez 75% des patients, alors que 17% des patients ont eu des suites compliquées de resténose ou mort (10% de mortalité en 10 ans). Ainsi, la réparation immédiate des lésions de la voie biliaire offre un bien meilleur pronostic que les réparations secondaires.
Resumen
Se presentaron 16 lesiones de la vía biliar en 7.057 colecistectomías (1972–1991), lo cual significa un riesgo de 0.22%. Desde Abril de 1990 se han practicado 1.022 colecistectomías laparoscópicas sin que se haya prsentado tal complicación.
En un estudio retrospectivo se estudiaron 64 pacientes con lesión o estenosis debido a colecistectomía convencional. En 14 de 16 la lesión fue reconocida y reparada inmediatamente con un buen resultado a largo plazo en 93%, incluyendo una exitosa reparación de una estrechez subsiguiente. Dos casos propios de lesión no reconocida fueron manejados por medios no operatorios. El grupo de 48 pacientes referidos estuvo conformado por 10 casos de complicaciones postoperatorias tempranas (21%) y 38 estrecheces luego de colecistectomía hecha “sin complicaciones”. Diez pacientes (16%) fueron tratados por medios no operatorios y 54 requirieron cirugía. El promedio de seguimiento después de la cirugía fue de 7.4 ±4.9 años. La mayoría de los casos (93%) fueron reparados mediante anastomosis bilioentérica, principalmente hepaticoyeyunostomía con una tasa de reestenosis de 18%. Incluyendo segundas y terceras reparaciones por estenosis, se realizaron 60 operaciones (14 reconstrucciones primarias y 46 secundarias) sin mortalidad hospitalaria. Se logró un buen resultado a largo plazo en 75% de los pacientes con reparaciones por estenosis y 17 pacientes exhibieron mal resultado, a juzgar por reestenosis o por muerte (10% mortalidad en 10 años). Por lo tanto, aparece obvio que la reparación inmediata de una lesión de la vía biliar ofrece la mejor oportunidad de un pronóstico favorable en comparación con la reparación secundaria de una estrechez.
Similar content being viewed by others
References
Meyers, W.C.: The Southern Surgeons Club. A prospective analysis of 1518 laparoscopic cholécystectomies. N. Engl. J. Med.324:073, 1991
Bismuth, H.: Postoperative strictures of the bile duct. In: The Biliary Tract. Clinical Surgery International, Vol. 5, L.H. Blumgart, editor. Edinburgh, Churchill Livingstone, 1982, pp. 209–218
Hepp, J.: Hepaticojejunostomy using the left biliary trunk for iatrogenic biliary lesions: the French connection. World J. Surg.9:507, 1985
Browder, W., Dowling, J.B., Koontz, K.K., Litwin, M.S.: Early management of operative injuries of the extrahepatic biliary tract. Ann. Surg.205:649, 1987
Andren-Sandberg, A., Johansson, S., Bengmark, S.: Accidental lesions of the common bile duct at cholecystectomy. II. Results and treatment. Ann. Surg.201:452, 1985
Blumgart, L.H.: Benign biliary strictures. In: Surgery of the Liver and Biliary Tract, L.H. Blumgart, editor. Edinburgh, Churchill Livingstone, 1988, pp. 721–752
Csendes, A., Diaz, J.C., Burdiles, P., Maluenda, F.: Late results of immediate primary end to end repair in accidental section of the common bile duct. Surg. Gynecol. Obstet.168:125, 1989
Czerniak, A., Thompson, J.N., Soreide, O., Benjamin, I.S., Blumgart, L.H.: The management of fistulas of the biliary tract after injury to the bile duct during cholecystectomy. Surg. Gynecol. Obstet.167:33, 1988
Kaufman, S.L., Kadir, S., Mitchell, S.E., et al.: Percutaneous transhepatic biliary drainage for bile leaks and fistulas. A.J.R.144:1055, 1985
Van Sonnenberg, E., Casola, G., Wittich, G.R., et al.: The role of interventional radiology for complications of cholecystectomy. Surgery107:632, 1990
Sauerbruch, T., Weinzierl, M., Holl, J., Pratschke, E.: Treatment of postoperative bile fistulas by internal endoscopic biliary drainage. Gastroenterology90:1998, 1986
Longmire, W.P., Tompkins, R.K.: Lesions of the segmental and lobar hepatic ducts. Ann. Surg.182:478, 1975
Hadjis, N.S., Blumgart, L.H.: Injury to segmental bile ducts. Arch. Surg.123:351, 1988
ReMine, S.G., Braasch, J.W., Rossi, R.L.: Unilateral hepatic duct obstruction. Am. J. Surg.153:86, 1987
Pellegrini, C.A., Thomas, M.J., Way, L.W.: Recurrent biliary stricture—patterns of recurrence and outcome of surgical therapy. Am. J. Surg.147:175, 1984
Pitt, H.A., Miyamoto, T., Parapatis, S.K., Thompkins, R.K., Longmire, W.P.: Factors influencing outcome in patients with postoperative biliary strictures. Am. J. Surg.144:14, 1982
Huibregtse, K., Katon, R.M., Tytgat, G.N.J.: Endoscopic treatment of postoperative biliary strictures. Endoscopy18:133, 1986
Berkelhammer, C., Kortan, P., Haber, G.B.: Endoscopic biliary prostheses as treatment for benign postoperative bile duct strictures. Gastrointest. Endosc.35:95, 1989
Williams, H.J., Bender, C.E., May, G.R.: Benign postoperative biliary strictures: dilation with fluoroscopic guidance. Radiology163:629, 1987
Rossi, P., Salvatori, F.M., Bezzi, M., Maccioni, F., Porcaro, M.L., Ricci, P.: Percutaneous management of benign biliary strictures with balloon dilation and self-expending metallic stents. Cardiovasc. Intervent. Radiol.13:231, 1990
Pitt, H.A., Kaufman, S.L., Coleman, J., White, R.I., Cameron, J.L.: Benign postoperative biliary strictures—operate or dilate? Ann. Surg.210:417, 1989
Terblanche, J., Worthley, C.S., Spence, R.A.J., Krige, J.E.: High or low hepaticojejunostomy for bile duct strictures? Surgery108: 828, 1990
Barker, E.M., Winkler, M.: Permanent-access hepaticojejunostomy. Br. J. Surg.71:188, 1984
Russell, E., Yrizarry, J.M., Huber, J.S., et al.: Percutaneous transjejunal biliary dilatation: alternate management for benign strictures. Radiology159:209, 1986
Genest, J.F., Nanos, E., Grundfest-Broniatowski, S., Vogt, D., Hermann, R.E.: Benign biliary strictures: an analytic review (1970 to 1984). Surgery99:409, 1986
Moossa, A.R., Mayer, A.D., Stabile, B.: Iatrogenic injury to the bile duct. Arch. Surg.125:1028, 1990
Warren, K.W., Jefferson, M.F.: Prevention and repair of strictures of the extrahepatic bile ducts. Surg. Clin. North Am.53:1169, 1973
Davidoff, A.M., Pappas, T.N., Murray, E.A., et al.: Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann. Surg.215:196, 1992
Moossa, A.R., Easter, D.W., van Sonnenberg, E., Casola, G., D'Ágostino, H.: Laparoscopic injuries to the bile duct. Ann. Surg.215:203, 1992
Cheslyn-Curtis, S., Emberton, M., Ahmed, H., Williamson, R.C.N., Habib, N.A.: Bile duct injury following laparoscopic cholecystectomy. Br. J. Surg.79:231, 1992
Lepsien, G., Lüdtke, F.E., Neufang, T., Schafmayer, A., Peiper, H.J.: Treatment of iatrogenic common bile duct injury during laparoscopic cholecystectomy through the laparoscopic insertion of a T-tube stent. Surg. Endosc.5:119, 1991
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Raute, M., Podlech, P., Jaschke, W. et al. Management of bile duct injuries and strictures following cholecystectomy. World J. Surg. 17, 553–562 (1993). https://doi.org/10.1007/BF01655124
Issue Date:
DOI: https://doi.org/10.1007/BF01655124