Summary
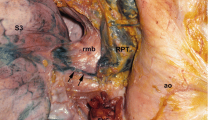
Correlation of the anatomic and surgical features in 360 cadavers and in 260 patients operated for bronchial carcinoma reveals that the lymphatics of the lung reach the ipsilateral mediastinum, sometimes directly and sometimes by sites which do not correspond to the anatomic site of the injection or of the pulmonary lesion. This implies the need for systematic eradication of all the lymph nodes of the ipsilateral mediastinum during surgery for bronchial carcinoma. In cases of tumoral lesions (N2), the prognosis is better when only one site is involved, whether the nodal disease is microscopic, uni- or multiglandular, with or without rupture of the capsule and whatever treatment is carried out, even when resection seems macroscopically complete to the surgeon. This is explicable in the light of the anatomic study, which shows that the lymph node chain is a functional entity which channels the lymph into the systemic circulation, either at the venous confluence of the neck or into the thoracic duct in the mediastinum. When only a single chain is affected, there is a greater than 70% chance that systemic metastases are already present, 90% when N2 affects 2 chains, while in N3 cases (lymph passage to contralateral chains) the incidence reaches virtually 100%. However, macroscopically satisfactory excision allows management of the local problem, and involvement of the mediastinal nodes, even with capsular rupture, cannot be considered as a contraindication in the absence of clinically detectable systemic metastases.
Résumé
La confrontation anatomochirurgicale de 360 cadavres et de 260 patients opérés de cancers bronchiques permet de constater que les lymphatiques du poumon rejoignent le médiastin homolatéral parfois directement et parfois par des sites qui ne correspondent pas au niveau anatomique de l'injection ou du cancer pulmonaire : ceci implique la nécessité de faire des curages systématiques de l'ensemble des lymphonoeuds du médiastin homolatéral lors de la chirurgie du cancer bronchique. En cas d'atteinte tumorale (N2), le pronostic est d'autant meilleur qu'un seul site est atteint, que l'atteinte nodale soit microscopique, uni ou plurinodale, avec ou sans rupture de la capsule et quel que soit le traitement réalisé, du moment que la résection semble macroscopiquement complète au chirurgien. Ceci s'éclaire à la lumière de l'étude anatomique qui montre que la chaine lymphonodale est une unité fonctionnelle qui déverse la lymphe dans la grande circulation soit au niveau des conflluents veineux du cou, soit dans le conduit thoracique au médiastin. En cas d'atteinte isolée d'une chaine, il y a plus de 70 % de chance pour que des métastases systémiques soient déjà présentes, 90 % quand N2 touche deux chaines et en cas de N3 (passage de la lymphe à des chaines controlatérales), cette fréquence atteint pratiquement 100 %. Mais, l'exérèse macroscopiquement satisfaisante permet de régler le problème local et l'atteinte des noeuds du médiastin, même avec rupture capsulaire ne peut pas être considére comme une contre-indication en l'absence de métastases systémiques cliniquement décelables.
Similar content being viewed by others
References
Cady B (1984) Lymph node metastases. Indicator, but not governors of survival. Arch Surg 119: 1007–1072.
Caplan I (1990) Anatomical review of the lymphnodes of the human mediastinum. Surg Radiol Anat 12: 9–18
Dyon MJF (1973) Contribution à l'étude du drainage des lymphatiques du poumon. Thèse Méd Grenoble
Maggi G (1988) Results of radical treatment of stage IIIa non small cell carcinoma of the Lung. Eur J Cardiothorac Surg 2: 329–335
Martini N, Flehinger BJ (1987) The role of surgery in N2 Lung Cancer. Surg Clin North Am 67: 1037–1049
Martini N, Flehinger BJ, Bains MS, Mc Cormack (1985) Management of stage III disease: alternate approaches to the management of mediastinal Adenopathy. In: Delarue NC, Eschapasse H (eds) International trends in general thoracic surgery (Lung cancer series, vol. 1) Saunders, Philadelphia, pp 108–120
Mountain CF (1986) A new international staging system for lung cancer. Chest 89: 225–233
Mountain CF (1985) The biological operability of Stage III non small cell lung cancer. Ann Thorac Surg 40: 60–64
Naruke T, Goya T, Tschuchiya R, Suemasu K (1988) The importance of surgery to non small cell carcinoma of lung with mediastinal lymph node metastasis. Ann Thorac Surg 46: 603–610
Naruke T, Suemasu K, Ishikawa S (1978) Lymph node mapping and curability at various level of metastasis in resected lung cancer. J Thorac Cardiovasc Surg 76: 832–839
Riquet M (1993) Anatomic basis of lymphatic spread from carcinoma of the lung to the mediastinum: surgical and pronostic implications. Surg Radiol Anat 15: 271–277
Riquet M, Debesse B, Hidden G (1986) Le drainage lymphatique des segments pulmonaires de l'adulte: faits cliniques et constations anatomiques. Bull Assoc Anat 70 : 43–47
Sakata K (1903) Uber die Lymphgefässe des Oesophagus und über seine regionalen Lymphdrüsen mit Berücksichtigung der Verbreitung des Karcinoms. Mitt Grenzgeb Med Chir 11: 634–656
Sarrazin R, Voog R, Dyon JF (1974) Contribution à l'étude des lymphatiques du poumon. Poumon Coeur 30: 289–299
Tisi GM, Triedman PJ, Peters RM, Pearson G, Can D, Lee Re Selavey O (1983) Clinical staging of primary lung cancer. Am Rev Respir Dis 123: 659–664
Watanabe Y, Ichihashi T, Iwat T (1988) Median sternotomy as an approach for pulmonary surgery. J Thorac Cardiovasc Surgeon 36: 227–231
Watanabe Y, Shimizu J, Oda M, Hayashi Y, Watanabe S, Tatouzawa Y, Iwa T, Suzuki M, Takashima T (1991) Aggressive surgical intervention in N2 non small cell cancer of the lung. Ann Thorac Surg 51: 253–260
Watanabe Y, Shimizu J, Tsubota M, Iwa T (1990) Mediastinal spread of metastatic lymph nodes in bronchogenic carcinoma. Mediastinal nodal metastases in lung cancer. Chest 97: 1059–1065
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Riquet, M., Manac'h, D., Dupont, P. et al. Anatomic basis of lymphatic spread of lung carcinoma to the mediastinum: anatomo-clinical correlations. Surg Radiol Anat 16, 229–238 (1994). https://doi.org/10.1007/BF01627676
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01627676