Abstract
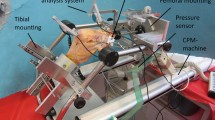
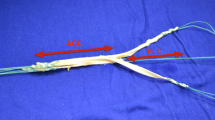
Compared to injuries of the other knee ligaments, a rupture of the posterior cruciate ligament (PCL) is relatively rare. Treatment may be conservative or operative. A rupture that has been operated on temporarily can be stabilised using a Grammont patello-tibial transfixation (olecranisation). Flexion and extension between 30° and 60° are allowed. The advantage of this method is that it avoids complete immobilisation of the joint and also the reduction of pull on the PCL. However, patients treated with this method show long-term osteoarthritis of the retropatellar joint area. Our study aimed to show the distribution of forces at the dorsal patellar surface in the following: (1) knee with intact ligament; (2) knee with PCL rupture; (3) knee with PCL rupture plus olecranisation. Fourteen fresh knee specimens were investigated in a Plitz/Wirth knee kinemator. The femur was fixed while the tibia was flexed between 5° and 120°. Pull was placed on the patella and on the dorsal side of the tibia with weights over the tendons of the quadriceps and the roots of the ischio-crural muscles. With the aid of a special measurement device in the patella, the medially laterally, proximally and distally acting forces in a movement cycle could be measured as well as the total retropatellar force in the above experimental setups. We found that, dependent on load and flexion angle in each preparation, (1) the total retropatellar force and some of the force components were greater when the PCL was ruptured than in the intact specimen. (2) with olecranisation the total force and the medial and lateral components were less than in the unrestricted patella with ruptured PCL, (3) the proximal area of the patella with olecranisation was less loaded than in the knee with either intact or defective PCL, and (4) the distal area of the patella with olecranisation was more loaded than in the knee joint with either intact or defective PCL.
Conclusions
To avoid destruction caused by overloading, especially in the distal area of the patella, the duration of patello-tibial transfixation should be carefully considered. Patients should be kept moving, at the same time being warned about excessive loading.
Similar content being viewed by others
References
Arnould H (1987) L'enclouage patello-tibial. Memoire du Concours de Medaille d'Or des Hôpiteaux, Interne des Hôpiteaux de Dijon, Prof. P. Grammont
Bandi W (1977) Die retropatellaren Kniegelenksschaden. Huber. Bern
Barton MT, Torg JS, Das M (1984) Posterior cruciate ligament insufficiency—a review of the literature. Sports Med 1:419–430
Baumgartner R, Müller W (1985) Die temporäre patello-tibiale transfixation in der Nachbehandlung von Rekonstruktionen hinterer Instabilitäten. Z Unfallchir Versicherungsmed Berufskr 78:28–35
Bücken U (1989) Entwicklung eines Kraftmesselementes für die Patella mit Fehlerkompensation bei nicht orthogonaler Krafteinleitung. Dissertation Fachhochschule Aachen
Dejour H, Walch G (1987) Die chronischen hinteren Instabilitäten. Orthopäde 16:149–156
Esser M, Dalziel R (1991) Posterior cruciate injuries in skiers. Ninth International Symposium on Ski Trauma and Skiing Safety, Threadbo, Australia
Grood ES, Suntay WJ, Noyes FR, Butler DL (1984) Biomechanics of the knee-extension exercise. J Bone Joint Surg [Am] 66:725–734
Hermens KA, Hackenbruch W (1986) Olecranisation of the patella in posterior instability of the knee. Orthop Rev 15:65–68
Hughston JC, Bowden JA, Andrews JR, Norwood LA (1980) Acute tears of the posterior cruciate ligament. J Bone Joint Surg [Am] 62:438–450
Lang J, Wachsmuth W (1972) Bein und Statik Springer, Berlin Heidelberg New York
Liorzou G (1991) Knee ligaments, clinical examinations. springer, Berlin Heidelberg New York
Reimeier E, Plitz W (1990) A theoretical and numerical approach to optimal positioning of the patellar surface replacement in a total knee endoprostheses. J Biomech 23:883–892
Stanish WD, Rubinovich M, Armason T, Lapenskie G (1986) Posterior cruciate ligament tears in wrestlers. Can J Appl Sports Sci 11:173–177
Trickey EL (1968) Rupture of the posterior cruciate ligament of the knee. J Bone Joint Surg [Br] 50:334–341
Trickey EL (1980) Posterior cruciate ligament injuries. Clin Orthop Rel Res 147:76–81
Vanquero J, Arriaza R (1992) The patella thinning osteotomy. An experimental study of a new technique for reducing patellofemoral pressure. Int Orthop 16:372–376
Wirth CJ, Kohn D (1989) Kreuzbandschaden—primäre und sekundäre Versorgungsstrategien. Chirurg 69:748–755
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hagena, F.W., Plitz, W., Mühlberger, G. et al. Retropatellar forces after rupture of the PCL and patello-tibial transfixation: An in vitro study. Knee Surg, Sports traumatol, Arthroscopy 2, 31–37 (1994). https://doi.org/10.1007/BF01552651
Issue Date:
DOI: https://doi.org/10.1007/BF01552651