Summary
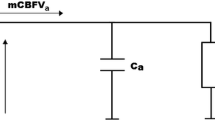
Testing vasoreactivity with CO2 or Diamox is a common diagnostic procedure for the study of haemodynamics in stroke patients. CO2 reactivity (CO2 R) was tested in 5 baboons six hours after permanent occlusion of the left middle cerebral artery (MCA) in order to attain new insights into interpretation of vasoreactivity tests. Using the microsphere method, cerebral blood flow (CBF) was determined in the various vascular territories as well as in the centre of the ischaemia, the penumbra and the remaining MCA-tissue. CBF decreased significantly in the affected MCA in all animals and in addition in the contralateral cerebellum in one animal (p < 0.05). In addition, the left anterior cerebral artery (ACA) demonstrated a similiar decrease. During hypercapnia CBF increased in all areas with the exception of the left, occluded MCA territory. Thus CO2 enhanced the difference between ischaemic and non-ischaemic tissue (i.e., tissue with diaschisis). Mean CO2 R was 3.37ml/100g/min/mmHg in the right MCA, 0.16 in the left. While the left ACA demonstrated a decreased perfusion during normocapnia in a similar range to the MCA territory, only CO2 R was able to identify precisely the territory of the occluded vessel. CO2 R was zero or negative in the ischaemic core, close to zero in the penumbra and profoundly decreased in the remaining MCA tissue. The overall CO2 R of the MCA was almost zero, suggesting vasoparalysis in response to hypercapnia in the core and penumbra and exhausted CO2 R even in non-infarcted, non-penumbral tissue. One animal displayed a negative CO2R equivalent to an intracerebral steal-phenomenon. Thus the CO2 challenge test helps to interpret CBF values by enhancing the differences between ischaemic and non-ischaemic tissue potentially distinguishing ischaemic tissue from low flow areas of different origin. The occluded vascular territory was identified correctly by CO2 R, not, however, by the normocapnic CBF measurement alone. Because of the risk of intracerebral steal phenomena it is recommended that the CO2 challenge test should not be performed during the acute stages of stroke.
Similar content being viewed by others
Abbreviations
- CBF:
-
cerebral blood flow
- MCA:
-
middle cerebral artery
- ACA:
-
anterior cerebral artery
- PCA:
-
posterior middle cerebral artery
- CO2 R CO2 :
-
reactivity
- SPECT:
-
single photon emission computed tomography
References
Baron JC, Bousser MG, Comar D, Castaigne P (1980) “Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc 105: 459–461
Bogsrud TV, Rootwelt K, Russell D, Nyberg-Hansen R (1990) Acetazolamide effect on cerebellar blood flow in crossed cerebral-cerebellar diaschisis. Stroke 21: 52–55
Brown MM, Wade JPH, Bishop CCR, Russell RWR (1986) Reactivity of the cerebral circulation in patients with carotid occlusion. J Neurol Neurosurg Psychiatry 49: 899–904
Buckberg GD, Luck JC, Payne BD, Hoffman JIE, Archie JP, Fixler DE (1971) Some sources of error in measuring regional blood flow with radioactive microspheres. J Appl Physiol 31: 598–604
Clifton GL, Halcott TH, Taylor JR, Sobel M (1988) Cerebrovascular CO2 reactivity after carotid artery occlusion. J Neurosurg 69: 24–28
Hartmann A, Menzel J, Buttinger C, Lange D, Alberti E (1981) Die regionale Gehirndurchblutung des Pavians beim ischämischen Hirninfarkt unter Dexamethasonbehandlung. Fortschr Neurol Psychiatr 49: 380–392
Heymann MA, Payne BD, Hoffman JIE, Rudolph AM (1977) Blood flow measurements with radionuclide-labeled particles. Cardiovasc Dis 20: 55–79
Herold S, Brown M, Frackowiack RSJ, Mansfield AO, Thomas DJ, Marshall J (1988) Assessment of cerebral haemodynamics reserve: correlation between PET parameters and CO2 reactivity measured by the intravenous133Xenon injection technique. J Neurol Neurosurg Psychiatry 51: 1045–1050
Hudgins WR, Garcia JR (1970) Transorbital approach to the middle cerebral artery of the squirrel monkey. A technique for experimental cerebral infarction applicable to ultrastructural studies. Stroke 1: 107–111
Jones SC, Bose B, Furlan AJ, Friel HT, Easley KA, Meredith MP, Little JR (1989) CO2 reactivity and heterogeneity of cerebral blood flow in ischaemic, border zone, and normal cortex. Am J Physiol 257: H 473-H 482
Kleiser B, Widder B (1992) Course of carotid artery occlusions with impaired cerebrovascular reactivity. Stroke 23: 171–174
Lassen NA, Astrup J (1987) Ischaemic penumbra. In: Wood JH (ed) Cerebral blood flow. McGraw-Hill, New York, pp 458–466
Levine RL, Dobkin JA, Rozental JM, Satter MR, Nickles RJ (1991) Blood flow reactivity to hypercapnia in strictly unilateral carotid disease: preliminary disease. J Neurol Neurosurg Psychiatry 54: 204–209
Levine RL, Lagrèze HL, Dobkin JA, Hanson JM, Satter MR, Rowe BR, Nickles RJ (1989) Cerebral vasocapacitance and TIAs. Neurology 39: 25–29
Norrving B, Nilsson B, Risberg J (1982) rCBF in patients with carotid occlusion. Resting and hypercapnic flow related to collateral pattern. Stroke 13: 155–162
O'Brien M, Waltz AG (1973) Transorbital approach for occluding the middle cerebral artery in baboons. Stroke 4: 201–206
Olsen TS, Larsen B, Herning M, Skriver EB, Lassen NA (1983) Blood flow and reactivity in collaterally perfused brain tissue. Evidence of an ischaemic penumbra in patients with acute stroke. Stroke 14: 332–341
Pappata S, Fiorelli M, Rommel T, Hartmann A, Dettmers C, Yamaguchi T, Chabriat H, Poline JB, Crouzel C, Giamberardino LDI, Baron JC (1993) PET study of changes in local brain haemodynamics and oxygen metabolism after unilateral middle cerebral artery occlusion in baboons. J Cereb Blood Flow Metab 13: 416–424
Symon L, Pasztor E, Branston NM (1974) The distribution and density of reduced cerebral blood flow following acute cerebral artery occlusion: an experimental study by the technique of hydrogen clearance in baboons. Stroke 5: 355–364
Symon L, Crockard HA, Dorsch NWC, Branston NM, Juhasz J (1975) Local cerebral blood flow and vascular reactivity in a chronic stable stroke in baboons. Stroke 6: 482–492
Takano T, Nagatsuka K, Ohnishi Y, Takamitsu Y, Matsuo H, Matsumoto M, Kimura K, Kamada T (1988) Vascular response to carbon dioxide in areas with and without diaschisis in patients with small, deep hemispheric infarction. Stroke 19: 840–845
Vorstrup S, Brun B, Lassen NA (1986) Evaluation of the cerebrovascular vasodilatatory capacity by the acetazolamide test before ECIC bypass surgery in patients with occlusion of the internal carotid artery. Stroke 17: 1291–1298
Yonas H, Durham SR, Smith HA, Johnson DW (1992) Acetazolamide vascular reserve testing identifies elevated stroke risk in patients with occlusive vascular disease. Washington, Second World Congress of Stroke, Proceedings, S 40
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dettmers, C., Young, A., Rommel, T. et al. CO2 reactivity in the ischaemic core, penumbra, and normal tissue 6 hours after acute MCA-occlusion in primates. Acta neurochir 125, 150–155 (1993). https://doi.org/10.1007/BF01401843
Issue Date:
DOI: https://doi.org/10.1007/BF01401843