Abstract
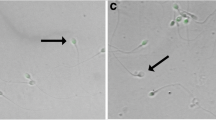
Failure of in vitro fertilization or very low cleavage rates may occur even though oocyte and semen parameters seem satisfactory. Quantified ultrastructural study of spermatozoa was performed in such cases of failure (n =6) or low cleavage rate (<20%; n =4). Through 1 to 11 retrievals, the number of inseminated oocytes ranged from 14 to 145. The results were compared to those of six fertile men. Quantification was achieved by cataloguing cell defects of the spermatozoon heads and mid-/principal pieces of the flagella. Using the data from each specimen, the percentages of total cellular abnormalities in the head/mid-/principal pieces were established. At the level of the head overall percentages for six groups of defects were determined. The overall percentage of combined head abnormalities, defined as the presence of at least three of these six defects on the same spermatozoon head, was established. Statistical differences among control and patient groups were analyzed by nonparametric Mann—Whitney Utest. The percentages of anomalies of the midpiece and of the principal piece were not significantly different between patients and controls. Motility assessed by spermogram was considered “functionally uncompromised.” In eight patients the percentage of cell alterations of the head (93–100 vs 77.3 ± 6.4%) and the percentage of combined anomalies of the head (78.1–100 vs 60.8 ± 8.5%) were significantly different between patients and controls. In two cases, the percentages established for all head parameters considered were not globally different from those observed in controls. Thus in 8 cases of 10, electron microscopy with quantified analysis supplied valuable evidence about the poor quality of these sperm samples judged as normal under light microscopy and may provide an explanation for their impaired fertilizability. In the two other cases the fact that the sperm appeared to be ultrastructurally normal does not rule out functional sperm pathology. Alternatively, defects in the oocyte may also account for unexplained failures of in vitro fertilization.
Similar content being viewed by others
References
Fawcett DW: The mammalian spermatozoon. Dev Biol 1975;44:394–436
Bisson JP, David G: Anomalies morphologiques du spermatozoïde humain. (2) Etude ultrastructurale. J Gynecol Obstet Biol Reprod 1975;4(S1):37–86
Bacceti B: The human spermatozoon.In Ultrastructure of Reproduction, J Van Blerkom, PM Motta (eds). Boston, Martinus Nijhoff, 1984, pp 110–126
Zamboni L: The ultrastructural pathology of the spermatozoon as a cause of infertility: The role of electron microscopy in the evaluation of semen quality. Fertil Steril 1987;48:711–734
Zamboni L: Physiology and pathophysiology of the human spermatozoon: The role of electron microscopy. J Electron Microsc Tech 1991;17:412–436
Von Bernhardi R, de Joannes AE, Blanco LP, Herrera E, Bustos-Obregon E, Vigil P: Round-headed spermatozoa: A model to study the role of acrosome in early events of gamete interaction. Andrologia 1990,22:12–20
Bartoov B, Eltes F, Langsam J, Snyder M, Fisher J: Ultrastructural studies in morphological assessment of human spermatozoa. Int J Androl 1982;Suppl 5:81–96
Escalier D: Human spermatozoa with large heads and multiple flagella: A quantitative ultrastructural study of 6 cases. Biol Cell 1983;48:65–74
Jouannet P, Escalier D, Serres C, David G: Motility of human sperm without outer dynein arms. J Submicrosc Cytol 1983;15:67–71
Serres C, Escalier D, David G: Ultrastructural morphometry of the human sperm flagellum with a stereological analysis of the lengths of the dense fibers. Biol Cell 1983;49:153–162
Escalier D, David G: Pathology of cytoskeleton of the human sperm flagellum: Axonemal and peri-axonemal anomalies. Biol Cell 1984;50:37–52
Escalier D, Serres C: Aberrant distribution of the periaxonemal structures in the human spermatozoon: Possible role of the axomeme in the spatial organization of the flagellar components. Biol Cell 1985;53:239–250
Serres C, Feneux D, Jouannet P: Abnormal distribution of the peri-axonemal structures in a human sperm flagellar dyskinesia. Cell Motil Cytoskel 1986;6:68–76
Carlon N, Navarro A, Pizant J: Etude ultrastructurale quantifiée du sperme dans 72 cas d'infécondité masculine. Contracept Fertil Sex 1991;19:985–993
David G, Bisson JP, Czyglik K, Jouannet P, Gernigon C: Anomalies morphologiques du spermatozoïde humain. (1) Propositions pour un système de classification. J Gynecol Obstet Biol Reprod 1975;4(S1):17–36
WHO: Laboratory Manual for the Examination Human Semen and Semen Cervical Mucus Interaction. Cambridge, University Press, 1987
De Almeida M, Soumah A, Jouannet P: Incidence of spermassociated immunoglobine in infertile men with suspected autoimmunity to sperm. Int J Androl 1986;9:321–330
Giorgetti C, Hans E, Spach JL, Barbeault JM, Franquebalme JP, Roulier R: Qualité de sperme et fécondation in vitro. Contracept Fertil Sex 1990;18:633–635
Fawcett DW, Philips DM: Recent observations on the ultrastructure and development of the mammalian spermatozoon.In Comparative Spermatology, B Bacetti (ed). Proceedings of the International Symposium in Rome, 1969, New York, Academic Press, 1970, pp 13–28
Pedersen H: Ultrastructure of the ejaculated human sperm.In Comparative Spermatology, B Baccetti (ed). Proceedings of the International Symposium in Rome, 1969, New York, Academic Press, 1970, pp 133–142
Escalier D, Bisson JP: Quantitative ultrastructural modifications in human spermatozoa after freezing.In Human Artificial Insemination and Semen Preservation, G David, WS Price (eds). 1980, pp 107–122
Holstein AF, Roosen-Runge EC: Atlas of Human Spermatogenesis. Grosse Verlag, 1981
David G, Escalier D: Apport de la microscopie électronique à l'examen du sperme.In Techniques d'examen du sperme: stage de formation permanente. Centre hospitalier de Bicêtre, 1986, pp 148–160
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Carlon, N., Navarro, A., Giorgetti, C. et al. Quantified ultrastructural study of spermatozoa in unexplained failure of in vitro fertilization. J Assist Reprod Genet 9, 475–481 (1992). https://doi.org/10.1007/BF01204054
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01204054