Abstract
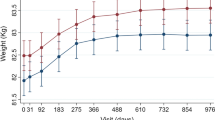
Background: In epidemiologic studies, excessive body weight, independent of other risk factors, portends a poor prognosis among patients with coronary artery disease experiencing acute myocardial infarction (MI). At least one recent study has suggested that patients of excessive body weight when receiving thrombolytic therapy are often underdosed, potentially reducing early coronary arterial patency and adversely affecting in-hospital clinical outcome. Concern has also been raised that body weight may influence treatment utilization, delays, and complication rates. Despite these concerns, the association between body weight and patient outcome following coronary thrombolysis has received limited attention.Methods/Results: Demographic, procedural, and outcome data from patients with MI were collected at 1073 United States hospitals participating in The National Registry of Myocardial Infarction from 1990 through 1994. Among 350,755 patients with MI enrolled, 87,688 (25.1%) were treated with tissue plasminogen activator (t-PA). Divided into body weight tertiles, 23.5% of patients were less than 70 kg (low weight), 36.8% were 70–85 kg (modrate weight), and 37.5% were greater than 85 kg (high weight). Patients of low weight were older (p < 0.001), received treatment later (p < 0.001), and were less likely to undergo cardiac catheterization, coronary angioplasty, or bypass surgery (p < 0.001) than moderate- or high-weight patients. Low-weight patients also experienced minor bleeding, major bleeding, recurrent MI, and death more often (p < 0.001). Adjusted for age, low body weight was independently associated with in-hospital mortality. Despite receiving a lower dose of t-PA per kg body weight, high-weight patients had a low incidence of cardiogenic shock, recurrent MI, death, and hemorrhagic complications.
When high-weight women and men were compared, several interesting observations emerged. Mortality was increased twofold in women (6.8% vs. 3.0; p < 0.001), even adjusting for their older age. Despite being at increased risk, women were less likely than their male counterparts to undergo cardiac catheterization (p=0.001) or bypass surgery (p=0.008).Conclusions: The National Registry of Myocardial Infarction provides a unique resource for assessing health care trends in the United States. Our findings suggest that low body weight is associated with increased in-hospital morbidity and mortality. They also suggest that current dosing strategies for t-PA administration are probably adequate for high-weight patients. The excessive mortality and limited use of in-hospital interventions among high-weight women deserve further study to address gender-related differences in disease processes, as well as potential bias or discrimination.
Similar content being viewed by others
References
Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study.Circulation 1983;5:968–977.
Noppa H, Bengtsson C, Wedel H, Wilhelmsen L. Obesity in relation to morbidity and mortality from cardiovascular disease.Am J Epidemiol 1980;111:682–692.
Rogers WJ, Bowlby LJ, Chandra NC, et al. For the participants in The National Registry of Myocardial Infarction. Treatment of myocardial infarction in the United States (1990 to 1993): Observations from The National Registry of Myocardial Infarction.Circulation 1994;90:2103–2114.
Jarrett RJ, Shipley MJ, Rose G. Weight and mortality in the Whitehall Study.Br Med J 1982;285:535–537.
Keen H, Thomas BJ, Jarrett RJ. Obesity and cardiovascular risk,Int J Obes 1982;6:83–89.
Dyer AR, Stamler J, Berkson DM, Lindberg HA. Relationship of relative weight and body mass index to 14 year old mortality in the Chicago Peoples Gas Company Study.J Chron Dis 1975;28:109–123.
Canning H, Mayer J. Obesity: An influence on high school performance.Am J Clin Nutr 1967;20:352–354.
Canning H, Hayer J. Obesity-its possible effect on college acceptance.N Engl J Med 1966;275:1172–1174.
Goldblatt PB, Moore ME, Stunkard AJ. Social factors in obesity.JAMA 1965;192:1039–1044.
Roe DA, Eickwort KR. Relationships between obesity and associated health factors with unemployment among low income women.JAMA 1976;31:193–204.
Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: Collaborative overview of early mortality and major morbidity results from all randomized trials of more than 1,000 patients.Lancet 1994;343:311–322.
The GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. V.Engl J Med 1993;329:673–682.
Bovill EG, Terrin ML, Stump DC, et al. and Chesebro JH, for the TIMI Investigators. Hemorrhagic events during therapy with recombinant tissue-type plasminogen activator, heparin, and aspirin for acute myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI), Phase II Trial.Ann Intern Med 1991;115:256–265.
Simoons MLK, Arnold AER. Tailored thrombolytic therapy: A perspective.Circulation 1993;88:2556–2564.
Karagounis LA, Anderson JL, Sorensen SG, Moreno FL for the TEAM-3 Investigators. Relation of reperfusion success with anistreplase or alteplase in acute myocardial infarction to body weight.Am J Cardiol 1994;73:16–22.
Smalling RW, Schumacher R, Morris D, et al. Improved infarct-related arterial patency after high dose, weightadjusted, rapid infusion of tissue plasminogen activator in myocardial infarction: Results of a multicenter randomized trial of two dosage regimens.J Am Coll Cardiol 1990;15:915–921.
Neuhaus KI, von Essen R, Tebbe U, et al. Improved thrombolysis in acute myocardial infarction with front loaded administration of alteplase: Results of the rt-PA-APSAC Patency Study (TAPS).J Am Coll Cardiol 1992;19:885–891.
Tanswell P, Tebbe U, Neuhaus K-L, Gläsle-Schwarz L, Wojcik J, Scifried E. Pharmacokinetics and fibrin specificity of alteplase during accelerated infusions in acute myocardial infarction.J Am Coll Cardiol 1992;19:1071–1075.
Becker RC, Terrin M, Ross R, Knatterud GL, Desvigne-Nickens P, Gore JM, Braunwald E, and the Thrombolysis in Myocardial Infarction Investigators. Comparison of clinical outcomes for women and men after acute myocardial infarction.Ann Intern Med 1994;120:638–645.
Tobin JN, Wassertheil-Smoller S, Wexler JP, et al. Sex bias in considering coronary bypass surgery.Ann Intern Med 1987;107:19–25.
Mark DB, Shaw LK, DeLong ER, Califf RM, Pryor DB. Absence of sex bias in referral of patients for cardiac catheterization.N Engl J Med 1994;330:1101–1106.
Kleiman NS, White HD, Ohman EM, et al. For the GUSTO Investigators. Mortality within 24 hours of thrombolysis for myocardial infarction.Circulation 1994;90:2658–2665.
Lee KL, Woodlief LH, Topol EJ, et al. for the GUSTO-1 Investigators. Predictors of 30-day mortality in the Era of Reperfusion for Acute Myocardial Infarction: Results from an international trial of 41,021 patients.Circulation 1995;91:1659–1668.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Becker, R.C., Gore, J.M., Rubison, M. et al. Association between body weight and in-hospital clinical outcome following thrombolytic therapy: A report from the national registry of myocardial infarction. J Thromb Thrombol 2, 231–237 (1995). https://doi.org/10.1007/BF01062715
Issue Date:
DOI: https://doi.org/10.1007/BF01062715