Abstract
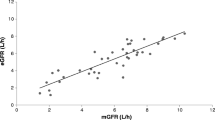
This study forms a part of an investigation into the extent to which the type of renal damage influences the renal clearance of drugs. We have already demonstrated an effect of different types of experimental renal failure (ERF) on the renal clearance of two cations: cimetidine, a drug that is filtered and secreted by the nephron, and lithium, which is filtered and reabsorbed by more than one segment of the nephron. In this report the renal clearance of cephalexin (CL CEX )is investigated, a drug that has a different mode of renal elimination, since it is filtered, secreted, and reabsorbed by the proximal tubules. The aim was to extend our earlier studies to an organic onion, and to provide an opportunity to evaluate the feasibility of using the renal clearance of N-1-methylnicotinamide (NMN) to predict the renal clearance of anionic drugs in renal failure. Different models of sitespecific ERF have been developed in the rat; proximal tubular necrosis (induced by cisplatin), papillary necrosis (induced by 2-bromoethylamine), andglomerulonephritis (induced by sodium aurothiomalate or by antiglomerular basement membrane antibodies). Glomerular function (GFR)was assessed by the clearance of inulin (CL NULIN ),and tubular function was assessed by the clearance of endogenous NMN (CL NLM .Our results show that even if the models of ERF used were not absolutely site-specific, glomerular function and tubular function did not decrease to the same extent in the different ERF. Therefore, glomerulo-tubular imbalance existed, which is incompatible with the “intact nephron hypothesis, ” i.e., the site of the damage along the nephron and not only the degree of renal dysfunction, is a potential source of variability in the clearance of certain drugs. The renal clearance ofcephalexin was estimated more accurately by CLNMN than GFR (r= 0.90). We conclude that the clearance of the endogenous cation NMN can be used to predict the renal clearance of drugs that are not only filtered by the glomeruli but also secreted and/or reabsorbed by the proximal tubules, and in the limited examples investigated appears to apply to both anionic and cationic compounds. In this respect the GFRalone was not an adequate parameter for the prediction of the renal clearance of such drugs.
Similar content being viewed by others
References
A. Maïza and P. T. Daley-Yates. Prediction of drug renal regimens in different diseases of the kidney using endogenous cation N-1-methylnicotinamide (NMN). In J. M. Aiache (ed.),Fourth European Congress of Biopharmaceutics and Pharmacokinetics, Special issue, Geneva, 1990, p. 409.
A. Maïza and P. T. Daley-Yates. Estimation of the renal clearance of drugs using endogenous N-1-methylnicotinamide.Toxicol. Letters 53:231–235 (1990).
K. Okumura, H. Katayama, M. Yasuhara, and H. Hori. Effect of protein binding on the disposition of cephalexin and cefazoloin in a simultaneous perfusion system of rat liver and kidney.Chem. Pharm. Bull. 37:3150–3152 (1989).
C. H. Nightingale, D. S. Greene, and R. Quintiliani. Pharmacokinetics and clinical use of cephalosporin antibiotics.J. Pharm. Sci. 64:1899–1927 (1975).
R. Hori, K. Okumura, H. Nihira, H. Nakano, K. Akagi, and A. Kamiya. A new dosing regimen in renal insufficiency: application to cephalexin.Clin. Pharmacol. Ther. 38:290–295 (1985).
A. Kamiya, K. Okumura, and R. Hori. Quantitative investigation on renal handling of drugs in rabbits, dogs, and humans.J. Pharm. Sci. 72:440–443 (1983).
A. Kamiya, K. Okumura, and R. Hori. Quantitative investigation of renal handling of drugs in dogs with renal insufficiency.J. Pharm. Sci. 73:892–896 (1984).
J. S. Welles, R. O. Froman, W. R. Gibson, N. V. Owen, and R. C. Anderson. Toxicology and pharmacology of cephalexin in laboratory animals.Antimicrob. Agents Chemother. 1968:489–496 (1969).
J. Fabre and L. Balant. Renal failure, drug pharmacokinetics and drug action.Clin. Pharmacokin. 1:99–120 (1976).
J. Fabre, L. Balant and A. Chavaz. Acquisitions recentes sur le maniement des medica-ments dans l'insuffisance renale. In J. Fabre, L. Balant, and A. Chavaz (eds.),Actualités Nephrologiques de l'Hopital Necker, Flammarion, Paris, 1974, pp. 7–14.
B. Petipierre and J. Fabre. Effet de l'insuffisance renale sur l'action hypoglycemiante des sulfonylurees. Cinetique de la chlorpropamide en cas de nephropathie.Schweiz. Med. Wochenschr. 102:570–578 (1972).
N. S. Bricker, P. A. F. Morrin, and S. W. Kime. The pathologic physiology of chronic Bright's disease.Am. J. Med. 28:77–88 (1960).
N. S. Bricker, R. Klahr, and R. E. Rieselbach. The functional adaptation of the diseased kidney. I. Glomerular filtration rate.J. Clin. Invest. 43:1915–1921 (1964).
N. S. Bricker, R. Klahr, H. Lubowitz, and R. E. Rieselbach. Renal physiology in chronic renal disease.Medicine 44:263–268 (1965).
P. Cottier and G. Haldeman. De l'emploi d'un sulfamide (RO-4-4393) a duree d'action prolongee dans le traitement de la pyelonephrite chronique.J. Urol. Nephrol. 70:797–809 (1964).
O. M. Williams, J. Wimpenny, and A. W. Asscher. Renal clearance of sodium sulfa-dimidine in normal and uraemic subjects.Lancet 2:1058–1060 (1968).
A. Maïza and P. T. Daley-Yates. Prediction of the renal clearance of cimetidine using endogenous N-1-methylnicotinamide.J. Pharmacokin. Biopharm. 19:175–188 (1991).
A. Maïza and P. T. Daley-Yates. The clearance of drugs in different types of renal disease (abstract).Renal Failure 11:67 (1988).
A. Maïza and P. T. Daley-Yates. Estimation of renal tubular secretion in man using endogenous N-1-methylnicotinaniide (NMN).Nephron 60:12–16 (1992).
K. H. Beyer, H. F. Russo, S. R. Gass, K. S. Wilhoyte, and A. A. Pitt. Renal tubular elimination of N-1-methylnicotinamide.Am. J. Physiol. 160:311–320 (1950).
A. Farah and M. Frazer. Studies on the uptake of N-1-methylnicotinamide by renal slices of the dog.J. Pharmacol. Exp. Ther. 126:202–211 (1959).
J. W. Huff and W. A. Perzweig. N-1-methylnicotinamide, a metabolite of nicotinic acid in the urine.J. Biol. Chem. 150:395–400 (1943).
M. Stanulovic and S. Chaykin. Metabolic origins of the pyridones of N-1-methylnicotin-amide in man and rat.Arch. Biochem. Biophys. 145:35–41 (1971).
B. R. Rennick. Renal tubule transport of organic cations.Am. J. Physiol. 240:F83 (1981).
J. C. Cal, A. Maïza, and P. T. Daley-Yates. The clearance of endogenous N-1-methyl-nicotinamide: a new marker of nephrotoxicity. In P. H. Bach, N. J. Gregg, M. F. Wilks, and L. Delacruz (eds.),Nephrotoxicity: Mechanisms, Early Diagnosis, and Therapeutic Management, Marcel Dekker, New York, 1991, pp. 41–46.
K. Nasseri and P. T. Daley-Yates. A comparison of N-1-methylnicotinamide clearance with five other markers of renal function in models of acute and chronic renal failure.Toxicol. Letters 53:231–245 (1990).
R. Barbhaiya and P. Turner. Fluorimetric assay of cephradin, cephalexin and cephalo-glycin.Br. J. Clin. Pharmacol. 4:427–431 (1977).
R. Greger, F. Lang, F. G. Knox, and C. Lechene. Analysis of tubule fluid. In M. Martinez-Maldonado (ed),Methods in Pharmacology, Vol. 4B, Plenum Press, New York, 1978, pp.105–120.
C. K. Shim, Y. Sawada, T. Iga, and M. Hanano. Estimation of renal blood flow by use of endogenous N-1-methylnicotinamide in rats.J. Pharmacobiodyn. 8:20–24 (1985).
A. H. Nagi, F. Alexander, and A. Z. Barabas. Gold nephropathy in rats-light and electron-microscopic studies.Exp. Mol. Pathol. 15:354–362 (1971).
B. V. Skrifvars. Hypothesis for the pathogenesis of sodium aurothiomalate (Myocrisin) induced immune complex nephritis.Scand. J. Rheum. 8:113–118 (1979).
T. S. Edgington, R. J. Glassock, J. A. Watson, and F. J. Dixon. Characterization and isolation of specific renal tubular epithelial antigens.J. Immunol. 99:1199–1210 (1967).
D. C. Cattran and W. B. Chodirker. Experimental membranous glomerulonephritis.Nephron 31:260–265 (1982).
D. C. Dobyan, J. Levi, C. Jacobs, J. Kosek, and M. W. Weiner. Mechanism of cis-platinum nephrotoxicity: II. Morphologic observations.J. Pharmacol. Exp. Ther. 213:551–556 (1980).
P. T. Daley-Yates and D. C. H. McBrien. Cisplatin (cis dichlorodiammine platinum II) nephrotoxicty. In P. H. Bach, F. W. Bonner, J. W. Bridges, and E. A. Lock (eds.),Nephro-toxicity, Assessment and Pathogenesis, Wiley, Chichester, 1982, pp. 356–370.
G. S. Hill, R. G. Willye, M. Miller, and R. M. Heptinstall. Experimental papillary necrosis of the kidney.Am. J. Pathol. 68:213–234 (1972).
R. Vanholder, N. Lameire, W. Eeckhaut, and S. Ringoir. Renal function studies in an experimental model of papillary necrosis in rat.Arch. Int. Physiol. Biochem. 89:63–73 (1981).
C. K. Shim, Y. Sawada, T. Iga, and M. Hanano. Effect of experimental renal failure on intrinsic renal tubular secretory clearance of organic cations in rats.J. Pharmacobiodyn. 6:787–789 (1983).
J. L. McNay, S. Rosello, and P. G. Dayton. Effects of azotemia on renal extraction and clearance of PAH and TEA.Am. J. Physiol. 230:901–906 (1976).
R. Hori, K. Okumura, A. Kamiya, H. Nihira, and H. Nakano. Ampicillin and cephalexin in renal insufficiency.Clin. Pharmacol. Ther. 34:792–798 (1983).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Maïza, A., Daley-Yates, P.T. Variability in the renal clearance of cephalexin in experimental renal failure. Journal of Pharmacokinetics and Biopharmaceutics 21, 19–30 (1993). https://doi.org/10.1007/BF01061773
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF01061773