Summary
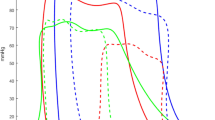
We evaluated the effect of trimetazidine (TMZ) on recovery of regional cardiac function in anesthetized open-chest pigs, subjected to fifteen 2-minute occlusions of the left anterior descending coronary artery, separated by 2 minutes of reperfusion and a 120-minute recovery period. Regional myocardial function was evaluated by sonomicrometry-derived segment lengthening and the area enclosed by the left ventricular pressure-segment length loop (external work, EW) in animals, which received either an intracoronary infusion of TMZ (33 µg/kg/min, n=6) or saline (1 ml/min, n=7), starting 15 minutes before the first occlusion and ending 2 minutes after the 15th occlusion. In addition, myocardial malondialdehyde production to evaluate oxygen free radical production, oxygen consumption, and the ATP, ADP, and AMP content, as well as the energy charge, were determined at regular time intervals.
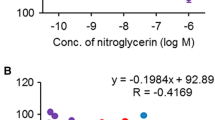
In control pigs the sequences of occlusion-reperfusion did not affect systemic hemodynamics, except for the LVdP/dtmax, which decreased by 11% during the interventions and did not recover during the following reperfusion period of 2 hours (78% of baseline, p<0.05). Systolic segment length shortening and EW were increased at the end of the first occlusion-reperfusion cycle, decreased gradually during the remainder of the occlusion-reperfusion periods, and did not improve during the recovery period. Energy charge and myocardial blood flow were not impaired, but oxygen consumption was decreased during the recovery period. The malondialdeyde data did not provide evidence for production of oxygen free radicals. TMZ decreased LVdP/dtmax by 6% (p<0.05) and caused a twofold increase in postsystolic segment shortening (p<0.05) before the first occlusion, but did not influence the hemodynamic responses, the changes in regional cardiac function, and the metabolic events produced by repetitive regional ischemia.
Similar content being viewed by others
References
Sellier P, Harpey C, Corona PP, Andouin P, Ourbak P. Ergometric parameters in effort angina.Cardiovasc Drugs Ther 1990;4:820–821.
Dalla-Volta S, Maraglino G, Della-Valentina P, Viena P, Desideri A. Comparison of trimetazidine with nifedipine in effort angina: A double-blind, crossover study.Cardiovasc Drugs Ther 1990;4:853–860.
Timour Q, Harpey C, Durr F, Faucon G. Is the antianginal action of trimetazidine independent of hemodynamic changes?Cardiovasc Drugs Ther 1991;5:1043–1044.
Lavanchy N, Martin J, Rossi A. Anti-ischemic effects of trimetazidine:31P-NMR spectroscopy in the isolated rat heart.Arch Int Pharmacodyn Ther 1987;286(Suppl 1): 97–110.
Renaud JF. Internal pH, Na+, and Ca2+ regulation by trimetazidine during cardiac cell acidosis.Cardiovasc Drugs Ther 1988;1:677–686.
Hugtenburg JG, Jap TJW, Mathy MJ, et al. Cardioprotective effect of trimetazidine and nifedipine in guinea-pig hearts subjected to ischaemia.Arch Int Pharmacodyn 1989;300:186–208.
Maridonneau-Parini I, Harpey C. Effect of trimetazidine on membrane damage induced by oxygen free radicals in human red cells.Br J Pharmacol 1985;20:148–151.
Guarnieri C, Muscari C. Beneficial effects of trimetazidine on mitochondrial function and superoxide production in the cardiac muscle of monocrotaline-treated rats.Biochem Pharmacol 1988;37:4685–4688.
Kober G, Buck T. Myocardial protection during PTCA: Effects of trimetazidine.Eur Heart J 1992;13:1109–1115.
Jaski BE, Serruys PW, Ten Katen H, Meij S. Epicardial wall motion and left ventricular function during coronary graft angioplasty in humans.J Am Coll Cardiol 1985;6:695–700.
Wijns W, Serruys PW, Slager CJ, et al. Effect of coronary occlusion during percutaneous transluminal angioplasty in humans on left ventricular chamber stiffness and regional diastolic pressure-radius relations.J Am Coll Cardiol 1986;7:455–463.
Bolli R. Oxygen-derived free radicals and postischemic myocardial dysfunction (“stunned myocardium”).J Am Coll Cardiol 1988;12:239–249.
Krams R, Duncker DJ, McFalls EO, Hoogendoorn A, Verdouw PD. Dobutamine restores the reduced efficiency of energy transfer from total mechanical work to external mechanical work is stunned porcine myocardium.Cardiovasc Res, 1993;27:740–747.
Vinten-Johansen J, Gayheart PA, Johnston WE, Julian JS, Cordell AR. Regional function, blood flow and oxygen utilization relation in repetitively occluded-reperfused canine myocardium.Am J Physiol 1991; 261:H538-H546.
Sassen LMA, Bezstarosti K, Verdouw PD, Lamers JMJ. Effects of nisoldipine on recovery of coronary blood flow, sarcoplasmic reticulum function and other biochemical parameters in post-ischaemic porcine myocardium.Biochem Pharmacol 1991;41:43–51.
Lamers JMJ, Hartog JM, Guarnieri C, Vaona I, Verdouw PD, Koster JF. Lipid peroxidation in normoxic and ischaemic-reperfused hearts of fish oil and lard fat fed pigs.J Mol Cell Cardiol 1988;20:605–615.
Atkinson DE. Energy charge of the adenylate pool as a regulatory parameter: Interaction with feedback modifiers.Biochemistry 1968;7:4030–4034.
Gaasch WH, Bernhardt SA. The effect of acute changes in coronary blood flow on left ventricular end-diastolic wall thickness—An echocardiographic study.Circulation 1977;56:593–598.
Verdouw PD, Ten Cate FJ, Hugenholtz PG. Effect of nifedipine on segmental myocardial function in the anesthetized pig.Eur J Pharmacol 1980;63:209–212.
Deutsch E, Berger M, Kussmaul WG, Hirshfeld JW, Herrmann HC, Laskey WK. Adaptation to ischemia during percutaneous transluminal coronary angioplasty.Circulation 1990;82:2044–2051.
Temporelli PL, Gianuzzi P, Gattone M, et al. Clinical relevance of ST segment changes during exercise in patients with anterior myocardial infarction.Eur Heart J 1992;13:403.
Maupoil V, Rochette L, Tabard A, Clauser P, Harpey C. Direct measurement of free radical generation in isolated rat heart by electron paramagnetic resonance spectroscopy: Effect of trimetazidine. In: Emerit I, Packer L, Auclair C, eds.Antioxidants in Therapy and Preventive Medicine. New York: Plenum Press, 1990:373–376.
Charlon V, Boucher F, Clauser P, et al. Effect of a 5 day trimetazidine pretreatment in a model of ischemic and reperfused isolated rat heart: Spin trapping experiments. In: Emerit I, Packer L, Auclair C, eds.Antioxidants in Therapy and Preventive Medicine. New York: Plenum Press, 1990:377–382.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Koning, M.M.G., Krams, R., Xiao, C.S. et al. Intracoronary trimetazidine does not improve recovery of regional function in a porcine model of repeated ischemia. Cardiovasc Drug Ther 7, 801–807 (1993). https://doi.org/10.1007/BF00878934
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00878934