Summary
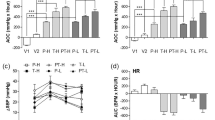
Cilazapril, and angiotensin-converting enzyme inhibitor, and mibefradil, a selective T-type voltage-operated calcium channel blocker, have been shown to prevent neointima formation after vascular injury. The goal of the present study was to evaluate the mechanism of action of both drugs. For this purpose, the influence of the renin angiotensin system on the effects of mibefradil (30 mg/kg po) and cilazapril (10 mg/kg po) on neointima formation after carotid injury were evaluated in normotensive rats (normal renin angiotensin system) and DOCA hypertensive rats (suppressed renin angiotensin system). In addition, in order to differentiate an effect on cell migration or cell proliferation, both drugs were given either before or after the smooth muscle migration phase. Finally, cilazapril and mibefradil were given in combination. In normotensive rats, mibefradil and cilazapril decreased neointima formation, resulting in neointima/media ratios of 38% (p<0.05) and 53% (p<0.01), respectively. However, in DOCA hypertensive rats, mibefradil was active, with a reduction of the neointima/media ratio by 63% (p<0.001), whereas cilazapril reduced it only slightly (19%) and not significantly. In addition, cilazapril was active only when treatment started before the migration phase (63%, reduction in neointima/media ratio, p<0.001) but not when started thereafter (13% reduction in neointima/media ratio, n.s.). In contrast, treatment with mibefradil was also active when started after the migration phase (51% reduction in neointima/media ratio, p<0.001 when treatment started 1 day before balloon injury and 41%, p<0.01 when treatment started 5 days after balloon injury). The combination of both drugs was additive (67% reduction in neointima/media ratio, p<0.001 vs. control). These experiments clearly show that mibefradil and cilazapril have a different mechanism of action after vascular injury. Mibefradil most likely prevents the proliferation of smooth muscle cells. In contrast, cilazapril most likely inhibits the migration of smooth muscle cells. These two different mechanisms of action explain why the effects of both drugs are additive.
Similar content being viewed by others
References
Powell JS, Clozel JP, Müller RKM, et al. Inhibitors of angiotensin-converting enzyme prevent myointimal proliferation after vascular injury.Science 1989;245:186–188.
Osterrieder W, Müller RKM, Powell JS, Clozel JP, Hefti F, Baumgartner HR. Role of angiotensin II in injury-induced neointima formation in rats.Hypertension 1991;18:II60-II64.
Mercator, Study Group. Does the new angiotensin converting enzyme inhibitor cilazapril prevent restenosis after percutaneous transluminal coronary angioplasty?Circulation 1992;86:100–110.
Clozel JP, Müller RKM, Roux S, Fischli W, Baumgartner HR. Influence of the status of the renin-angiotensin system on the effect of cilazapril on neointima formation after vascular injury in rats.Circulation 1993;88:1222–1227.
Fingerle J, Müller RKM, Kuhn H, Pech M, Baumgartner HR. Mechanism of inhibition of neointima formation by the angiotensin converting enzyme inhibitor cilazapril.Arterioscler Thromb Vasc Biol 1995;15:1945–1950.
Stary HC, Blankenhorn DH, Chandler AB, et al. A definition of the intima of human arteries and of its atherosclerosis-prone regions.Arterioscler Thromb 1992;12:120–134.
Clowes AW, Reidy MA, Clowes MM. Kinetic of cellular proliferation after arterial injury.Lab Invest 1983:49:327–334.
Epstein SE, Speir E, Unger EF, Guzman RJ, Finkle T. The basis of molecular strategies for treating coronary restenosis after angioplasty.J Am Coll Cardiol 1994;23:1278–1288.
Block PC. Restenosis after percutaneous transluminal coronary angioplasty—Anatomic and pathophysiological mechanisms.Circulation 1990;81:IV2-IV4.
Osterrieder W, Holck M. In vitro pharmacologic profile of Ro 40–5967, a novel Ca2+ channel blocker with potent vasodilator but weak inotropic action.J Cardiovasc Pharmacol 1989;13:754–759.
Clozel JP, Osterrieder W, Kleinboesem CH, et al. Ro 40–5967, A new nondihydropyridine calcium antagonist.Cardiovasc Drug Rev 1991;9:4–17.
Mishra SK, Hermsmeyer K. Selective inhibition of T-type Ca2+ channels by Ro 40–5967.Circ Res 1994;75:144–18.
Schmitt R, Clozel JP, Iberg N, Bühler F. Mibefradil prevents neointima formation after vascular injury in rats: Possible role of the blockade of the T-type voltage-operated calcium channel.Arterioscler Thromb, in press.
Carretero OA, Romero JC. Production and characteristics of experimental hypertension in animals. In: Genest J, Koiw E, Kuchel O, eds.Hypertension. New York: McGraw-Hill, 1977:485–506.
Oates HF, Stokes GS, Storey BG. Plasma renin concentration in hypertension produced by unilateral renal artery constriction in the rat.Clin Exp Pharmacol Physiol 1975; 2:289–296.
Natoff IL, Nixon JS, Francis RJ, et al. Biological properties of the angiotensin-converting enzyme inhibitor cilazapril.J Cardiovasc Pharmacol 1985;7:569–580.
Gerold M, Tschirky H. Measurement of blood pressure in unanesthetized rats and mice.Arzneim-Forsch/Drug Res 1969;18:1285–1287.
Haudenschild CC, Schwartz SM. Endothelial regeneration: II. Restitution of endothelial continuity.Lab Invest 1979; 41:407–418.
Daemen MJAP, Lombardi DM, Bosman FT, Schwartz SM. Angiotensin II induces smooth muscle cell proliferation in the normal and injured rat arterial wall.Circ Res 1991;68:450–456.
Clozel JP, Hess P, Schietinger K, Breu V, Fischli W, Baumgartner HR. Major role of the renin angiotensin system in the neointima formation after vascular injury in guinea pigs.Life Sci 1994;54:PL87–92.
Schmitt R, Kleinboesem CH, Belz GG. Hemodynamic and humoral effects of the novel calicum antagonist Ro 40–5967 in patients with hypertension.Clin Pharmacol Ther 1992; 52:314–323.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schmitt, R., Clozel, J.P., Iberg, N. et al. Prevention of neointima formation by mibefradil after vascular injury in rats: Comparison with ACE inhibition. Cardiovasc Drug Ther 10, 101–105 (1996). https://doi.org/10.1007/BF00823586
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00823586