Summary
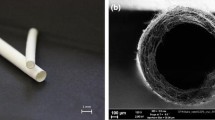
The ultrastructure of a new type of vascular graft, prepared from a mixture of polyurethane (95 weight %) and poly-L-lactic acid (5 weight %), was examined six weeks after implantation into the abdominal aorta of rats. These microporous, compliant, biodegradable, vascular grafts function as temporary scaffolds for the regeneration of the arterial wall.
Smooth muscle cells, covering the grafts, regenerated a neo-media underneath an almost completely regenerated endothelial layer (neo-intima). These smooth muscle cells varied in morphology from normal smooth muscle cells to myofibroblasts. They were surrounded by elastic laminae and collagen fibers.
Macrophages, epithelioid cells, multinucleated giant cells, fibroblasts and capillaries were present in the disintegrating graft lattices. The epithelioid cells and multinucleated giant cells engulfed polymer particles of the disintegrating grafts.
The regeneration of the endothelial and smooth muscle cells is similar to the natural response of arterial tissue upon injury. The presence of macrophages, epithelioid cells, multinucleated giant cells, fibroblasts and capillaries in the graft lattices resembles the natural response of tissue against foreign body implants. Both of these responses result in the formation of a neo-artery that possesses sufficient strength, compliance and thromboresistance to function as a small caliber arterial substitute.
Similar content being viewed by others
References
Adams DO (1976) The granulomatous inflammatory response. A review. Am J Pathol 84:164–191
Albert EN (1972) Developing elastic tissue. An electron microscopic study. Am J Pathol 69:89–102
Anderson JM, Miller KM (1984) Biomaterial biocompatibility and the macrophage. Biomaterials 5:5–10
Berger KE, Sauvage LR, Rao AM, Wood SJ (1972) Healing of arterial prosthesis in man: its incompleteness. Ann Surg 175:118–127
Bossart MI, Turner SA, Milam JD, Connor DJ, Urrutia CO, Frazier OH (1982) Multipotential cells in the circulating blood: ultrastructural evidence in the calf. Trans Am Soc Artif Intern Organs 28:185–189
Castellot JJ Jr, Addonizio ML, Rosenberg R, Karnovsky MJ (1981) Cultured endothelial cells produce a heparin-like inhibitor of smooth muscle cell growth. J Cell Biol 90:372–379
Chemnitz J, Christensen BC (1984) Repair in arterial tissue. Demonstration of fibrinogen/fibrin in the normal and healing rabbit thoracic aorta by the indirect immunoperoxidase technique. Virchows Arch Pathol Anat 403:163–171
Clark RA, Stone RD, Leung DYK, Silver I, Hohn DC, Hunt TK (1976) Role of macrophages in wound healing. Surg Forum 27:16–18
Coleman DL, King RN, Andrade JD (1974) The foreign body reaction: a chronic inflammatory response. J Biomed Mater Res 8:199–211
DiCorleto PE, Bowen-Pope DF (1983) Cultured endothelial cells produce a platelet-derived growth factor-like protein. Proc Natl Acad Sci 80:1919–1923
Evans G, Mustard JF (1968) Platelet-surface reaction and thrombosis. Surgery 64:273–280
Fisher-Dzoga K, Chen R, Wissler RW (1974) Effects of serum lipoproteins on the morphology, growth and metabolism of arterial smooth muscle cells. Adv Exp Med Biol 43:299–311
Fishman JA, Ryan GB, Karnovsky MJ (1975) Endothelial regeneration in the rat carotid artery and the significance of endothelial denudation in the pathogenesis of myointimal thickening. Lab Invest 32:339–351
Gajdusek C, DiCorletto P, Ross R, Schwartz SM (1980) An endothelial cell-derived growth factor. J Cell Biol 85:467–472
Gebrane J, Orcel L (1982) The evolution of experimental endarteritis in the rabbit abdominal aorta. Light and transmission electron microscopy. Virchows Arch Pathol Anat 398:205–220
Gebrane J, Roland J, Orcel L (1982) Experimental diffuse intimal thickening of the femoral arteries in the rabbit. Virchows Arch Pathol Anat 396:41–59
Gerrity RG, Cliff WJ (1975) The aortic tunica media of the developing rat. I Quantitative stereologic and biochemical analysis. Lab Invest 32:585–600
Gerrity RG, Adams EP, Cliff WJ (1975) The aortic tunica media of the developing rat. II Incorporation by medial cells of 3H-Proline into collagen and elastin: Autoradiographic and chemical studies. Lab Invest 32:601–609
Gogolewski S, Pennings AJ (1982) Biodegradable material of polylactides, 4a. Porous biomedical materials based on mixtures of polylactides and polyurethanes. Markromol Chem, Rapid Commun 3:839–845
Gogolewski S, Pennings AJ (1983) Resorbable materials of poly(1-lactide). 3 Porous materials for medical application. Colloid Polym Sci 261:477–484
Hassler O (1970) The origin of cells constituting arterial intimal thickening. An experimental autoradiographic study with the use of 3H-thymidin. Lab Invest 22:286–293
Haudenschild CC, Schwartz SM (1979) Endothelial regeneration. II Restitution of endothelial continuity. Lab Invest 41:407–418
Hess F, Jerusalem C, Braun B (1983) The endothelialization process of a fibrous polyurethane microvascular prosthesis after implantation in the abdominal aorta of the rat. J Cardiovasc Surg 24:516–524
Hinek A, Thyberg J (1977) Electron microscopic observations on the formation of elastic fibers in primary cultures of aortic smooth muscle cells. J Ultrastruct Res 60:395–401
Hulstaert CE, Kalicharan D, Hardonk MJ (1983) Cytochemical demonstration of phosphatases in the rat liver by a ceriumbased method in combination with osmium tetroxide and potassium ferrocyanide postfixation. Histochemistry 78:71–79
Karnovsky MJ (1981) Endothelial-vascular smooth muscle cell interactions. J Cell Biol 105:200–206
Lei B vd, Darius H, Schrör K, Molenaar I, Nieuwenhuis P, Wildevuur ChRH (1984) Improved neo-endothelialization of small caliber vascular grafts. Proc ESAO XI: 332–334
Lei B vd, Wildevuur ChRH, Nieuwenhuis P (1985a) Mechanical stimulation of smooth muscle cells by arterial pulsations. An important stimulus for the formation of elastic laminae in arterial tissue. Cell Biol Int Rep vol. 9 no 1:2
Lei B vd, Darius H, Schrör K, Nieuwenhuis P, Molenaar I, Wildevuur ChRH (1985b) Arterial wall regeneration in small caliber vascular grafts. Neo-endothelial healing and prostacyclin production. J Thoracic Cardiovasc Surg (in press)
Lei B vd, Bartels HL, Nieuwenhuis P, Wildevuur ChRH (1985c) Microporous, compliant, biodegradable vascular grafts for the regeneration of the arterial wall in rat abdominal aorta. Surgery (in press)
Lei B vd, Wildevuur ChRH, Nieuwenhuis P (1985d) Compliance and biodegradation of vascular grafts stimulate the regeneration of elastic laminae in neo-arterial tissue: An experimental study in rats. Surgery (in press)
Leibovich SJ, Ross RA (1976) A macrophage dependent factor that stimulates the proliferation of fibroblasts in vitro. Am J Pathol 84:501–513
Leung DYM, Glagov S, Mathews MB (1976) Cyclic stretching stimulates synthesis of matrix components by arterial smooth muscle cells in vitro. Science 191:475–477
Leung DYM, Glagov S, Mathews MB (1977) A new in vitro system for studying cell response to mechanical stimulation. Different effects of cyclic stretching and agitation on smooth muscle cell biosynthesis. Exp Cell Res 109:285–298
Lommen E, Gogolewski S, Pennings AJ, Wildevuur ChRH, Nieuwenhuis P (1983) Development of a neo-artery induced by a biodegradable polymeric vascular prosthesis. Trans Am Soc Artif Intern Organs 29:255–259
Madri JA, Stenn KS (1982) Aortic endothelial cell migration. I. Matrix Requirements and composition. Am J Pathol 106:180–186
Malckzak HT, Buck RC (1977) Regeneration of endothelium in rat aorta after local freezing. Am J Pathol 86:133–141
Mariano M, Spector WG (1974) The formation and properties of macrophage polykaryons (inflammatory giant cells). J Pathol 113:1–19
Martin BM, Gimbrone MA, Unanue ER, Cotran RS (1981) Stimulation of nonlymphoid mesenchymal cell proliferation by a macrophage-derived growth factor. J Immunol 126:1510–1515
Mehdorn HM, Townsend JJ, Weinstein PR, Chater NL, Meyermann R, Buncke HJ (1979) Endothelialization of a new arterial microvascular graft material. Scan Electron Microsc III:851–856
Minick CR, Stemerman MB, Insull W Jr (1979) Role of endothelium and hypercholesterolemia in intimal thickening and lipid accumulation. Am J Pathol 95:131–158
Nemetschek-Gansler H, Weiss H, Wenisch HJC, Noetzel B, Pretzsch U (1979) Intimal thickening of human femoral arteries with special regard to elastin. Part 1, Diffuse intimai thickening due to growth and age. Atherosclerosis 34:167–191
O'Neal RM, Jordan GL, Rabin ER, DeBakey ME, Halpert B (1964) Cells grown on isolated Dacron hubs, an electron microscopic study. Exp Mol Pathol 3:403–412
Papadimitriou JM, Spector WG (1971) The origin, properties and fate of epithelioid cells. J Pathol 105:187–203
Papadimitriou JM, Walters MN-I (1979) Macrophage polykarya. CRC Crit Rev Toxicol 6:211–255
Paule WJ (1963) Electron microscopy of the newborn rat aorta. J Ultrastruct Res 8:219–235
Poole JCF, Cromwell SB, Benditt EP (1971) Behaviour of smooth muscle cells and formation of extracellular structures in the reaction of arterial walls to injury. Am J Pathol 62:391–414
Polverini PJ, Cotran RS, Gimbrone MA, Unanue ER (1977) Activated macrophages induce vascular proliferation. Nature 269:804–806
Reidy MA, Schwartz SM (1981) Endothelial regeneration. Time course of intimal changes after small defined injury to rat aortic endothelium. Lab Invest 44:301–308
Ross R (1971) The smooth muscle cell I. In vivo synthesis of connective tissue proteins. J Cell Biol 50:159–171
Ross R, Klebanoff SY (1971) The smooth muscle cell II. Growth of smooth muscle cell in culture and formation of elastic fibers. J Cell Biol 50:172–186
Ross R, Glomset J, Kariya B, Harker L (1974) A platelet dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Nat Acad Sci 71:1207–1210
Salthouse TN (1984) Some aspects of macrophage behaviour at the implant interface. J Biomed Mater Res 18:395–401
Schaper J, König R, Franz D, Schaper W (1976) The endothelial surface of growing coronary collateral arteries. Intimal margination and diapedesis of monocytes. A combined SEM and TEM study. Virchows Arch Path Anat 370:193–205
Schor AM, Schor SL, Allen TD (1983) Effects of culture conditions on the proliferation, morphology and migration of bovine aortic endothelial cells. J Cell Sci 62:267–285
Schwartz SM, Stemerman MB, Benditt EP (1975) The aortic intima. II Repair of the aortic lining after mechanical denudation. Am J Pathol 81:15–42
Schwartz SM, Haudenschild CC, Eddy EM (1978) Endothelial regeneration. I Quantitative analysis of initial stages of endothelial regeneration in rat aortic intima. Lab Invest 38:568–580
Spagnoli LG, Pietra GG, Villaschi S, Johns LW (1982) Morphometric analysis of gap junctions in regenerating arterial endothelium. Lab Invest 46:139–148
Stemerman MB, Spaet TH, Pitlick F, Cintron J, Lejnieks I, Tiell ML (1977) Intimal healing. The pattern of reendothelialization and intimai thickening. Am J Pathol 87:125–142
Stoute LC, Thorpe LW (1980) Histology of normal aortas in nonhuman primates with emphasis on diffuse intimal thickening (DIT). Atherosclerosis 35:165–180
Stump MM, Jordan GL, De Bakey ME, Halpert B (1963) Endothelium grown from circulating blood on isolated intravascular dacron hub. Am J Pathol 43:361–367
Sutton JS, Weiss L (1966) Transformation of monocytes in tissue culture into macrophages, epithelioid cells and multinucleated giant cells. J Cell Biol 28:303–332
Thakral KK, Goodsen WH, Hunt TK (1979) Stimulation of wound blood vessel growth by wound macrophages. J Surg Res 26:430–436
Thorgeirsson G, Lazzarini-Robertson A (1978) The vascular endothelium: pathobiologic significance: a review. Am J Pathol 93:803–848
Waiden R, L'Italien GJ, Megerman J, Abbott WM (1980) Matched elastic properties and successful arterial grafting. Arch Surg 115:1166–1169
Webster WS, Bishop SP, Geer JC (1974) Experimental aortic intimai thickening. I. Morphology and source of intimal cells. Am J Pathol 76:245–261
Author information
Authors and Affiliations
Additional information
Supported by Grant nr. 82.042 from the Dutch Heart Foundation
Rights and permissions
About this article
Cite this article
van der Lei, B., Wildevuur, C.R.H., Nieuwenhuis, P. et al. Regeneration of the arterial wall in microporous, compliant, biodegradable vascular grafts after implantation into the rat abdominal aorta. Cell Tissue Res. 242, 569–578 (1985). https://doi.org/10.1007/BF00225423
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00225423