Abstract
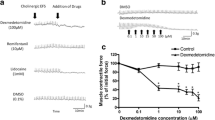
Pulmonary function is reportedly impaired by fiberoptic bronchoscopy. We investigated the effect of two anticholinergic agents, intramuscular atropine and inhaled ipratropium bromide, on bronchoconstriction in 29 patients who were undergoing diagnostic bronchoscopy. The patients were divided into three groups; the first received 0.5 mg of atropine intramuscularly; the second took four puffs of 0.02 mg ipratropium bromide aerosolized by a metered-dose inhaler, and the third inhaled four puffs of a placebo. Fifteen minutes later a standardized topical anesthetic, lidocaine, was administered, and a bronchoscopic examination was performed. Pulmonary function was measured before and 15 minutes after each step. Pulmonary function was not affected by the treatment with anticholinergics or the placebo. In the placebo and the atropine groups, the topical anesthesia produced significant reductions in forced expiratory volume in 1 second (FEV,) and peak expiratory flow rate (PEFR); further reductions in these values were observed after bronchoscopy. In the group treated with ipratropium bromide there were no significant changes in FEV, and PEFR after topical anesthesia. Bronchoscopy induced significant reductions in FEV1 and PEFR, but the changes were significantly smaller than those seen in the placebo and atropine groups. The results suggest that the deleterious effect of bronchoscopy on pulmonary function is due to topical lidocaine anesthesia and to the bronchoscopic examination itself. Inhaled ipratropium bromide protects against these deleterious effects, whereas intramuscular atropine does not.
Similar content being viewed by others
References
Aizawa H, Chung KF, Leikauf GD, Ueki I, Bethel RA, O'Byrne PM, Hirose T, Nadal JA (1985) Significance of thromboxane generation in ozone-induced airway hyperresponsiveness in dogs. J Appl Physiol 59:1918–1923
Anggard E, Samuelsson B (1965) Biosynthesis of prostaglandins from arachidonic acid in guinea pig lung. J Biol Chem 240:3518–3521
Beasley RCW, Featherstone RL, Church MK, Rafferty P, Varley JG, Harris A, Robinson C, Hollgate ST (1989) Effects of a thrombovane receptor antagonist on PGD2- and allergen-induced bronchoconstriction. J Appl Physiol 66:1685–1693
Chung KF, Aizawa H, Becker AB, Frick O, Gold WN, Nadal JA (1986) Inhibition of antigen-induced airway hyperresponsiveness by a thromboxane synthetase inhibitor (OKY-046) in allergic dogs. Am Rev Respir Dis 134:258–261
Chung KF, Aizawa H, Leikauf GD, Ueki I, Evans TW, Nadal JA (1986) Airway hyperresponsiveness induced by platelet-activating factor: role of thromboxane generation. J Pharmacol Exp Ther 236:580–584
Coleridge HM, Coleridge JCG (1986) Reflexes evoked from the tracheobranchial tree and lungs. In: Cherniack NS, Widdicombe JG (eds) Handbook of Physiology, Section 3. The respiratory system, vol. 11, part 2: Control of respiration. American Physiological Society, Washington, D.C., pp 395–429
Graybar GB, Harrington JK, Cowen KH, Spannhake EW, Hyman AL, McNamara DB, Kadowitz PJ (1986) Cyclooxygenase mediated airway response to leukotriene D4 in the cat. Prostaglandins 31:167–177
Greenberg R, Antonaccio MJ, Steinbacher T (1982) Thromboxane A2 mediated bronchoconstriction in anesthetized guinea pig. Eur J Pharmacol 80:19–27
Hamberg M, Samuelsson B (1973) Detection and isolation of an endoperooxidase intermediate in prostaglandin biosynthesis. Proc Natl Acad Sci USA 70:899–903
Hamberg M, Samuelsson B (1974) Prostaglandin endoperoxidases. VII. Novel transformation of arachidonic acid in guinea pig lung. Biochem Biophys Res Commun 61:942–949
Hamberg M, Sevensson J, Samuelsson B (1975) Thromboxanes: a new group of biologically active compounds derived from prostaglandin endoperoxidases. Proc Natl Acad Sci USA 72:2994–2998
Hanasaki K, Arita H (1988) Characterization of a new compound, S-145, as a specific TXA2 receptor antagonist in platelets. Thromb Res 50:365–376
Hanasaki K, Nagasaki T, Arita H (1989) Characterization of platelet thromboxane A2/prostaglandin H2 receptor by a novel tromboane receptor antagonist, [3H]S-145. Biochem Pharmacol 38:2007–2017
Laurindo FRM, Goldstein RE, Davenport NJ, Ezra D, Feuerstein GZ (1989) Mechanisms of hypotension produced by platelet-activating factor. J Appl Physiol 66:2681–2690
Liu F, Carrithers JA, Shirer HW, Orr JA (1992) Thromboxane A2 mimetic, U46619, and slowly adapting stretch receptor activity in the rabbit. Respir Physiol 88:77–86
Mais DE, Saussy DL, Chaikhouni A, Kochel PJ, Knapp DR, Hamanaka N, Halushka PV (1985) Pharmacological characterization of human and canine thromboxane A2/prostaglandin H2 receptors in platelets and blood vessels: evidence for different receptors. J Pharmacol Exp Ther 233:418–424
Munoz NM, Shioya T, Murphy TM, Primack S, Dame C, Sands MF, Leff AR (1986) Potentiation of vagal contractile response by the thromboxane mimetic U-46619. J Appl Physiol 61:1173–1179
Narisada M, Ohtani M, Watanabe F, Uchida K, Arita H, Doteuchi M, Hanasaki K, Kakushi H, Otani K, Hara S (1988) Synthesis and in vitro activity of various derivations of a novel thromboxane receptor antagonist, (+)-5(Z)-7-(3-endo-phenyl-sulfonylamine-[2,2,1]bicyclohept-2-exo-yl) heptenomic acid. J Med Chem 31: 1847–1854
Nugteren DH, Hazelhop E (1973) Isolation and properties of intermediates in prostaglandin biosynthesis. Biochem Biophys Acta 326:448–461
O'Byrne PM, Leikauf GD, Aizawa H, Bethel RA, Ueki I, Holtzman MJ, Nadel JA (1985) Leukotriene B4 induces airway hyperresponsiveness in dogs. J Appl Physiol 59:1941–1946
Spannhake EW, Lemen RJ, Wegmann MJ, Hyman AL, Kadowitz PJ (1978) Analysis of airway effects of PGH2 analogue in the anesthetized dog. J Appl Physiol 44:406–415
Svensson J, Standberg K, Tuvemo T, Hamberg M (1977) Thromboxane A2: effects on airway and vascular smooth muscle. Prostaglandins 14:425–436
Takano S, Ishimoto H, Nakahata N, Nakanishi H (1992) Thromboxane A2 receptor characterization in human astrocytoma cells and rabbit platelets by a new thromboxane antagonist, [3H]ONO NT-126. Res Commun Chem Path Pharmacol 76:155–170
Toda N, Nakajima M, Okamura T, Miyazaki M (1986) Interactions of thromboxane A2 analogs and prostaglandins in isolated dog arteries. J Cardiovasc Pharmacol 8:818–825
Tymkewycz PM, Jones RL, Wilson NH, Marr CG (1991) Heterogeneity of thromboxane A2 (TP-) receptors: evidence from antagonist but not agonist potency measurements. Br J Pharmacol 102:607–614
Underwood DC, Kriseman T, MacNamara DB, Hyman AL, Kadowitz PJ (1987) Blockade of thromboxane responses in the airway of the cat by SQ29548. J Appl Physiol 62:2193–2200
Vargaftig BB, Lefort J, Chingnard M, Benveniste J (1980) Platelet-activating factor induces a platelet-dependent bronchoconstriction unrelated to the formation of prostaglandin derivatives. Eur J Pharmacol 65:185–192
Author information
Authors and Affiliations
Additional information
Offprint request to: H. Aizawa
Rights and permissions
About this article
Cite this article
Inoue, H., Aizawa, H., Takata, S. et al. Ipratropium bromide protects against bronchoconstriction during bronchoscopy. Lung 172, 293–298 (1994). https://doi.org/10.1007/BF00164311
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00164311