Abstract
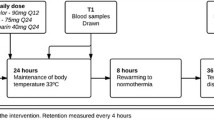
We wanted to test the hypothesis that NO generation by L-arginine (LA) infusion will be beneficial in increasing blood flow to all organs to counteract the process of global ischemia during cardiopulmonary bypass (CPB) and to reduce platelet emboli by platelet inhibition. The effect of LA infusion on NO formation, vasodilation, and reduction of thromboembolic burden in organs and tissues after CPB was quantified with In-111-labeled autologous platelets in two major groups: 180 minutes CPB (CPB) and 90 minutes CPB plus 90 minutes reperfusion (RP). Platelets labeled with In-111 tropolone (650–780 μCi) were administered 24 hours before CPB and LA infusion (bolus, 10 mg/kg and infusion at 2 mg/kg/min, 21 pigs for 180 minutes CPB) in 8 groups of 30 Yorkshire pigs (30–35 kg, 6 pigs; LA 2 mg/kg/min, 3 pigs; sham-thoracotomy control, 6 pigs; unoperated control, 6 pigs). Two groups of 9 pigs (control CPB, 6 pigs; LA 2 mg/ kg/min, 3 pigs) underwent 90 minutes of CPB and 90 minutes of reperfusion. All pigs were heparinized (ACT >400 seconds); CPB was instituted with a roller pump, an oxygenator (OX: Bentley Univox, 1.8 m2), and an arterial filter (AF: 0.25 m2, Bentley) at a blood flow of 2.5–3.5 1/min. Radioactive thrombi in OX and AF and emboli in viscera, brain, and connective tissues were imaged with a gamma camera and were finally measured with an ion chamber and a gamma counter. The percent of injected platelets (mean ± SD) in the organs and tissues of all pigs was calculated. Cerebral emboli were mapped in 25 regions of both hemispheres of pig brain. Flow cytometry with antibodies to CD61 (GPIIIa) and CD62P (GMP-140: control) of porcine platelets was carried out with blood samples taken before, during, and after CPB. Coronary bypass with LA infusion decreased the amount of adherent thrombi in OX and AF (p < 0.07). The embolic burden in brain and lung also decreased. Regional cerebral mapping of In-111 platelets showed reduced emboli in almost all regions, including the medulla, hippocampus, and posterior cerebral cortex in both LA-treated groups. Flow cytometry of blood samples demonstrated the shift of equilibria from single platelet to platelet-aggregate-microparticle during CPB and steady-state level after the first 5–10 minutes of initiation of CPB. The L-arginine infusion reduced thrombi and emboli during CPB in the pig model.
Similar content being viewed by others
References
Woodman RC, Harker LA. Bleeding complications associated with cardiopulmonary bypass. Blood 1990;76:1680–1697.
Turner NA, Moake JL, Kamat SJ, et al. Comparative real-time effects on platelet adhesion and aggregation under flowing conditions of in vivo aspirin, heparin, and monoclonal antibody fragment against glycoprotein IIb-IIIa. Circulation 1995;91:1354–1362.
Kestin AS, Valeri CR, Khuri SF, et al. The platelet function defect of cardiopulmonary bypass. Blood 1993;82:107–117.
O'Toole TE, Lomis JC, Plow EF, et al. Efficient surface expression of platelet IIb-IIIa requires both subunits. Blood 1989;74:14–18.
Pugsley W, Klinger L, Paschalis C, Aspey B, Newman S, Harrison M, Treasure T. Microemboli and cerebral impairment during cardiac surgery. Vasc Surg 1990;24:34–43.
Dewanjee MK, Tago M, Josa M, et al. Quantification of platelet retention in aortocoronary femoral vein bypass graft in dogs treated with dipyridamole and aspirin. Circulation 1984;69:350–356.
Peterson KA, Dewanjee MK, Kaye MP. Fate of indium-111 labeled platelets during cardiopulmonary bypass performed with membrane and bubble oxygenators. J Thor Cardiovasc Surg 1982;84:39–43.
Palatianos GM, Dewanjee MK, Smith W, et al. Platelet preservation during cardiopulmonary bypass with iloprost and heparin-coated surface. Trans ASAIO 1991;37:620–622.
Dewanjee MK, Belinskiy V, Holland JFW, et al. Dominant effect of thoracotomy on platelet and neutrophil dynamics during cardiopulmonary bypass in a pig model. J Thromb Thromboly, 1995;3:195–208.
Dewanjee MK, Rao SA, Didisheim P. Indium-111 tropolone, a new high affinity platelet label: Preparation and evaluation of labeling parameters. J Nucl Med 1981;22:981–987.
Menys VC, Belcher PR, Noble MIM, et al. Macroaggregation of platelets in plasma, as distinct from microaggregation in whole blood (and plasma), as determined using optical aggregometry and platelet counting respectively, is specifically impaired following cardiopulmonary bypass in man. Thromb Haemostas 1994;72:511–518.
Dietrich WD, Dewanjee S, Prado R, Watson BD, Dewanjee MK. Transient platelet accumulation in the rat brain after common carotid artery thrombosis: An 111In-labeled platelet study. Stroke 1993;24:1534–1540.
Dewanjee MK, Palatianos GN, Kapadvanjwala M, et al. Neutrophil dynamics and retention in lung, oxygenator and arterial filter during cardiopulmonary bypass (CPB) in pig model. ASAIO J 1994;40:M547-M553.
Dewanjee MK, Kapadvanjwala M, Mao WW, et al. Higher blood flow window of reduced thrombogenicity and acceptable fragmentation in a hollow-fiber hemodialyzer. ASAIO J 1993;39:M363-M367.
Dewanjee MK, Kapadvanjwala M, Cavagnaro CF, et al. In vitro and in vivo evaluation of the comparative thrombogenicity of cellulose acetate hemodialyzers with radiolabeled platelets. ASAIO J 1994;40:49–55.
Ault KA, Rinder HM, Mitchell JG, Rinder CS, Lambrew CT, Hillman RS. Correlated measurements of platelet release and aggregation in whole blood. Cytometry 1989;10:448–455.
Findik D, Reuter C, Presek P. Platelet membrane glycoproteins IIb and IIIa are substrates or purified pp60c-src protein kinase. FEBS Lett 1989;262:1–4.
Clark EA, Brugge JA. Integrins and signal transduction pathways: The road taken. Science 1995;268:233–239.
Macdonald RL, Kowalalczuk A, Johns L. Emboli enter penetrating arteries of monkey brain in relation to their size. Stroke 1995;26:1247–1251.
Harris DNF, Bailey SM, Smith PLC, Taylor KM, Oatridge A, Bydder GM. Brain swelling in first hour after coronary artery bypass surgery. Lancet 1993;342:586–587.
Dewanjee MK. Quantitation of platelet consumption in health and disease. In Martin-Comin J, ed. Radiolabeled Blood Elements. New York: Plenum Press, 1994:67–90.
Furchgott RF, Zawadzki JV. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 1980;288:373–386.
Hecker M, Sessa WC, Harris HJ, Anggard EE, Vane JR. The metabolism of L-arginine and its significance for the biosynthesis of endothelial-derived relaxation factor: Cultured endothelial cells recycle L-citrulline to L-arginine. Proc Natl Acad Sci USA 1990;87:8612–8616.
Knowles RG, Palacios M, Palmer RMJ, Moncada S. Formation of nitric oxide from L-arginine in the central nervous system: A transduction mechanism for stimulation of the soluble guanylate cyclase. Proc Natl Acad Sci USA 1989;86:5159–5162.
McCall TB, Boughton-Smith NK, Palmer RMJ, Whittle BJR, Moncada S. Synthesis of nitric oxide by L-arginine by neutrophils. Biochem J 1989;261:293–296.
Marletta MA, Yoon PS, Iyengar R, Leaf CD, Wishnok JS. Macrophage oxidation of L-arginine to nitrite and nitrate: Nitric oxide as an intermediate. Biochemistry 1988;27:8706–8711.
Billar TR, Curran RD, Stuehr DJ, West MA, Bentz BG, Simmons RL. An arginine-dependent mechanism mediates Kupffer cell inhibition of hepatocyte protein synthesis. J Exp Med 1989;169:1467–1472.
Radomski MW, Palmer RMJ, Moncada S. An L-arginine: nitric oxide pathway present in human platelets regulates aggregation. Proc Natl Acad Sci USA 1990;87:5193–5197.
Fineman JR, Chang R, Soifer SJ. L-arginine, precursor of EDRF in vitro, produces pulmonary vasodilation in lambs. Am J Physiol 1991;261:H1563-H1569.
Stuehr DJ, Nathan CF. Nitric oxide a macrophage product responsible for cytostasis and respiratory inhibition in tumor target cells. J Exp Med 1989;169:1543.
Rossaint R, Falke KJ, Lopez F, Slama K, Pison U, Zapol WM. Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med 1993;328:399–405.
Ketteler M, Border WA, Nobel NA. Cytokines and Larginine in renal injury and repair. Am J Physiol 1994;267:F197-F207.
Auphan N, DiDonato JA, Rosette C, Helmberg A, Karin M. Immunosuppression by glucocorticosteroids: Inhibition of NF-kB activity through inhibition of IkB synthesis. Science 1995;270:286–290.
Morris SM, Billiar TR. New insights into the regulation of inducible nitric oxide synthesis. Am J Physiol 1994;266:E829-E839.
MacLeod CL, Finley KD, Kakuda DK. Y+ type cationic amino acid transport: Expression and regulation of mCAT genes. J Exp Biol, 1994;196:109–121.
Knowles RG, Moncada S. Nitric oxide synthases in mammals. Biochem J 1994;298:249–258.
Wennmalm A. Endothelial nitric oxide and cardiovascular disease. J Int Med 1994;235:317–327.
Wink DA, Kasprzak KS, Maragos CM, et al. DNA deaminating ability and genotoxicity of nitric oxide and its progenitors. Science 1991;254:1001–1003.
Stamler JS, Jaraki O, Osborne J, et al. Nitric oxide circulates in mammalian plasma primarily as S-nitroso adduct of serum albumin. Proc Natl Acad Sci USA 1992;89:7674–7677.
de Belder A, Radomski M, Hancock V, Brown A, Moncada S, Martin J. Megakaryocytes from patients with coronary atherosclerosis express the inducible nitric oxide synthase. Arterioscler Thromb Vasc Biol 1995;15:637–641.
Greenberg RS, Helfaer MA, Kirsch JR, Moore LE, Traystman RJ. Nitric oxide synthase inhibition with NG-monomethyI-L-arginine reversibly decreases cerebral blood flow in piglets. Crit Care Med 1994;22:384–392.
Genaro AM, Hortelano S, Alvarez A, Martinez AC, Bosca L. Splenic B lymphocyte programmed cell death is prevented by nitric oxide release through mechanisms involving sustained bcl-2 levels. J Clin Inv 1995;95:1884–1890.
Bredt DS, Hwang PM, Glatt CE, Lowenstein C, Reed RR, Snyder SH. Cloned and expressed nitric oxide synthase structurally resembles cytochrome P-450 reductase. Nature 1991;351:714–718.
Boje KM, Aroa Pk. Microglia-produced nitric oxide and reactive nitrogen oxides mediate neuronal cell death. Brain Res 1992;587:250–256.
Matheis G, Sherman MP, Buckberg GD, Haybron DM, Young HH, Ignarro LJ. Role of L-arginine-nitric oxide pathway in myocardial reoxygenation injury. Am J Physiol 1992;262:H616-H620.
Gauthier TW, Davenpeck KL, Lefer AM. Nitric oxide attenuates leukocyte-endothelial interaction via P-selectin in splanchnic ischemia-reperfusion. Am J Physiol 1994;267:G562-G568.
Gauthier TW, Scalia R, Murohara T, Guo J, Lefer AM. Nitric oxide protects against leukocyte-endothelium interactions in the early stages of hypercholesterolemia. Thromb Vasc Biol 1995;15:1652–1659.
Clancy RN, Leszczyvka-Pirsok J, Abramson RB. Nitric oxide an endothelial cell relaxing factor, inhibits neutrophil superoxide anion production via a direct action on the NADPH oxidase. J Clin Inv 1992;90:1116–1121.
Zhang F, White JG, Iadecola C. Nitric oxide donors increase blood flow and reduce brain damage in focal ischemia: Evidence that nitric oxide is beneficial in the early stages of cerebral ischemia. J Cereb Blood Flow Metab 1994;14:217–226.
Pulsinelli WA. The therapeutic window in ischemic brain injury. Curr Opin Neural 1995;8:3–5.
Offner PJ, Robertson FM, Pruitt BA. Effects of nitric oxide synthase inhibition on regional blood flow in a porcine model of endotoxic shock. J Trauma Inj Infect Crit Care 1995;39:338–343.
Gross SS. Nitric oxide: Pathophysiological mechanisms. Ann Rev Physiol 1995;57:737–769.
Whitman ED, Doherty GM, Peplinsky GR, Norton JA. Role of cytokines in oxidative damage. In: Aggarwal BB, Puri RK, eds. Human Cytokines: Cambridge, MA: Blackwell Science, 1995:333–352.
Kapas L, Shibata M, Krueger JM. Role of cytokines in sleep, fever and anorexia. In: Aggarwal BB, Puri RK, eds. Human Cytokines: Their Role in Disease and Therapy. Cambridge, MA: Blackwell Science, 1995:305–314.
Wahlgren NG. Cytoprotective therapy for acute ischemic stroke. In: Stroke Therapy. Boston: Butterworth, 1995:315–350.
The General Linear Model Procedure. In: SAS/STAT Software, SAS/STAT User's Guide, Version 6, 4th ed, Volume 2. Gary NC: SAS Institute, 1989:893–993.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dewanjee, M.K., Wu, S.M., Kapadvanjwala, M. et al. Reduction of platelet thrombi and emboli by L-arginine during cardiopulmonary bypass in a pig model. J Thromb Thrombol 3, 343–360 (1996). https://doi.org/10.1007/BF00133078
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00133078