Abstract
Background
The history, ECG, age, risk factor (HEAR) score has been proposed to identify patients at sufficiently low risk of acute coronary syndrome that they may not require troponin testing. The objective of this study was to externally validate a low HEAR score to identify emergency department (ED) patients with chest pain at very low risk of 30-day major adverse cardiac events (MACE).
Methods
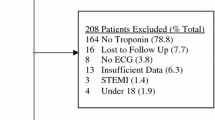
This was a secondary analysis of a prospective cohort of patients requiring troponin testing to rule out myocardial infarction (MI) in a large urban ED. HEAR scores were calculated in two cohorts: (1) patients with no known history of coronary artery disease (CAD); and (2) all eligible patients. The proportion of patients classified as very low risk, sensitivity, specificity, predictive values and likelihood ratios at each cut-off were quantified for index acute myocardial infarction (AMI) and 30-day MACE at HEAR = 0 and HEAR ≤ 1 thresholds.
Results
Of the 1150 patients included in this study, 820 (71.3%) had no history of CAD, 97 (8.4%) had index AMI and 123 (10.7%) had 30-day MACE. In patients with no prior history of CAD, HEAR ≤ 1 identified 202 (24.6%) of patients as very low risk for 30-day MACE with 98.4% (95% CI 91.6–99.9%) sensitivity. Among all patients, HEAR ≤ 1 identified 202 (17.6%) patients as very low risk for 30-day MACE with 99.2% (95% CI 95.6–99.9%) sensitivity.
Conclusions
A HEAR score ≤ 1 can identify more than 17% of all patients as very low risk for index AMI and 30-day MACE and unlikely to benefit from troponin testing. Broad implementation of this strategy could lead to significant resource savings.
Résumé
Contexte
Le score HEAR (History, ECG, Age, Risk Factor) a été proposé pour identifier les patients présentant un risque suffisamment faible de syndrome coronarien aigu pour ne pas nécessiter de test à la troponine. L’objectif de cette étude était de valider à l’externe un faible score HEAR afin d’identifier les patients du service d’urgence (DE) souffrant de douleurs thoraciques à très faible risque d’événements cardiaques indésirables majeurs (MACE) de 30 jours.
Méthodes
Il s'agissait d'une analyse secondaire d'une cohorte prospective de patients nécessitant un test à la troponine pour exclure un infarctus du myocarde (IM) dans un grand service d'urgence urbain. Les scores HEAR ont été calculés dans deux cohortes : (1) les patients sans antécédents connus de maladie coronarienne (MC) ; et (2) tous les patients éligibles. La proportion de patients classés à très faible risque, la sensibilité, la spécificité, les valeurs prédictives et les rapports de vraisemblance à chaque seuil ont été quantifiés pour l'infarctus aigu du myocarde (IAM) de l'index et la MACE à 30 jours aux seuils HEAR = 0 et HEAR ≤ 1.
Résultats
Sur les 1 150 patients inclus dans cette étude, 820 (71.3%) n'avaient pas d'antécédents de coronaropathie, 97 (8.4%) avaient un IAM index et 123 (10.7%) avaient une MACE à 30 jours. Chez les patients sans antécédents de coronaropathie, HEAR ≤ 1 a identifié 202 (24,6%) des patients comme présentant un très faible risque de MACE à 30 jours avec une sensibilité de 98.4% (IC 95% 91.6–99.9%). Parmi tous les patients, HEAR ≤ 1 a identifié 202 (17.6%) patients comme présentant un très faible risque de MACE à 30 jours avec une sensibilité de 99.2% (IC 95% 95.6–99.9%).
Conclusions
Un score HEAR ≤ 1 peut identifier plus de 17% de tous les patients comme étant à très faible risque d'IAM d'index et de MACE à 30 jours et peu susceptibles de bénéficier d'un test à la troponine. La mise en œuvre à grande envergure de cette stratégie pourrait permettre de réaliser d’importantes économies de ressources.
Similar content being viewed by others
Change history
25 March 2024
A Correction to this paper has been published: https://doi.org/10.1007/s43678-024-00671-x
References
Ko DT, Dattani ND, Austin PC, et al. Emergency department volume and outcomes for patients after chest pain assessment. Circ Cardiovasc Qual Outcomes. 2018;11:e004683. https://doi.org/10.1161/circoutcomes.118.004683.
Hess EP, Brison RJ, Perry JJ, et al. Development of a clinical prediction rule for 30-day cardiac events in emergency department patients with chest pain and possible acute coronary syndrome. Ann of Emerg Med. 2012;59:115-125.e111. https://doi.org/10.1016/j.annemergmed.2011.07.026.
Liu N, Ng JCJ, Ting CEA, et al. Clinical scores for risk stratification of chest pain patients in the emergency department: an updated systematic review. J Emerg Crit Care Med. 2018. https://doi.org/10.21037/jeccm.2018.01.10.
Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge. Circulation. 2018;138:2456–68. https://doi.org/10.1161/CIRCULATIONAHA.118.036528.
Six A, Backus B, Kelder J. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16:191–6. https://doi.org/10.1007/BF03086144.
Laureano-Phillips J, Robinson RD, Aryal S, et al. HEART score risk stratification of low-risk chest pain patients in the emergency department: a systematic review and meta-analysis. Ann Emerg Med. 2019. https://doi.org/10.1016/j.annemergmed.2018.12.010.
Backus BE, Six AJ, Cullen L, et al. The HEART score for chest pain patients at the emergency department validated in a multi centre Asia-Pacific population. Eur Heart J. 2012;1:6–7. https://doi.org/10.1093/eurheartj/ehs281.
Brady W, de Souza K. The HEART score: a guide to its application in the emergency department. Tur J Emerg Med. 2018;18:47–51. https://doi.org/10.1016/j.tjem.2018.04.004.
Stopyra JP, Riley RF, Hiestand BC, et al. The HEART pathway randomized controlled trial one-year outcomes. Acad Emerg Med. 2019;26:41–50. https://doi.org/10.1111/acem.13504.
Streitz MJ, Oliver JJ, Hyams JM, et al. A retrospective external validation study of the HEART score among patients presenting to the emergency department with chest pain. Int Emerg Med. 2018;13:727–48. https://doi.org/10.1007/s11739-017-1743-4.
Smith LM, Ashburn NP, Snavely AC, et al. Identification of very low-risk acute chest pain patients without troponin testing. Emerg Med J. 2020. https://doi.org/10.1136/emermed-2020-209698 (emermed-2020-209698).
Mahler SA, Burke GL, Duncan PW, et al. HEART pathway accelerated diagnostic protocol implementation: prospective pre-post interrupted time series design and methods. JMIR Res Prot . 2016;5: e10. https://doi.org/10.2196/resprot.4802.
Moumneh T, Sun BC, Baecker A, et al. Identifying patients with low-risk of acute coronary syndrome without troponin testing: VALIDATION of the HEAR score. Am J Med. 2020. https://doi.org/10.1016/j.amjmed.2020.09.021.
Otsuka Y, Takeda S. Validation study of the modified HEART and HEAR scores in patients with chest pain who visit the emergency department. Acute Med Surg. 2020;7:e591. https://doi.org/10.1002/ams2.591.
Andruchow JE, Boyne T, Innes G, et al. Low high-sensitivity troponin thresholds identify low-risk patients with chest pain unlikely to benefit from further risk stratification. CJC Open. 2019;1:289–96. https://doi.org/10.1016/j.cjco.2019.08.002.
Andruchow JE, Boyne T, Seiden-Long I, et al. Prospective comparative evaluation of the European Society of Cardiology (ESC) 1-h and a 2-h rapid diagnostic algorithm for myocardial infarction using high-sensitivity troponin-T. CJEM. 2020. https://doi.org/10.1017/cem.2020.349.
Ghali WA, Knudtson ML. Overview of the alberta provincial project for outcome assessment in coronary heart disease. On BEHALF of the APPROACH investigators. Can J Cardiol. 2000;16:1225–30.
Moons KGM, Altman DG, Reitsma JB, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Int Med. 2015;162:W1-73. https://doi.org/10.7326/M14-0698.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35. https://doi.org/10.1161/CIR.0b013e31826e1058.
Wickham H, François R, Henry L, Müller K. dplyr: A grammar of data manipulation. 2020. https://dplyr.tidyverse.org/. Accessed 15 July 2021.
Stepinska J, Lettino M, Ahrens I, et al. Diagnosis and risk stratification of chest pain patients in the emergency department: focus on acute coronary syndromes. A position paper of the acute cardiovascular care association. Eur Heart J Acute Cardiovasc Care. 2020;9:76–89. https://doi.org/10.1177/2048872619885346.
Andruchow JE, Kavsak PA, McRae AD. Contemporary emergency department management of patients with chest pain: a concise review and guide for the high-sensitivity troponin Era. Can J Cardiol. 2018;34:98–108. https://doi.org/10.1016/j.cjca.2017.11.012.
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. https://doi.org/10.1002/sim.2929.
Funding
The parent study was funded by an investigator initiated, non-restricted research grant from Roche Diagnostics Canada.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
The original online version of this article was revised: Authorship correction.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
O’Rielly, C.M., Andruchow, J.E., McRae, A.D. et al. External validation of a low HEAR score to identify emergency department chest pain patients at very low risk of major adverse cardiac events without troponin testing. Can J Emerg Med 24, 68–74 (2022). https://doi.org/10.1007/s43678-021-00159-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-021-00159-y