Abstract
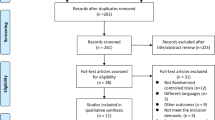
Polycystic ovary syndrome (PCOS) is a heterogeneous condition that affects women of reproductive age. It is associated with menstrual disturbances, hyperandrogenism, and polycystic ovaries. In addition to this, it results in altered anthropometric parameters, insulin resistance, and subsequently untoward cardio-metabolic sequelae. Therapeutic approaches that target weight loss and improve insulin sensitivity are used to address the metabolic complications in PCOS. Curcumin is a phytochemical which exhibits anti-inflammatory and anti-oxidant properties, and therefore, its use in PCOS has been a subject of substantial interest and research. The aim of this study was to synthesize the existing evidence on the effects of curcumin on glycaemic and lipid parameters in PCOS. We searched PubMed, Embase, Web of Science, Scopus, and ClinicalTrials databases from inception to June 07, 2021. Only randomized controlled trials (RCT) presenting sufficient data on glycemic and lipid parameters in patients with PCOS at baseline and the end of the follow-up period in each group were included. Meta-analysis of five RCTs showed a significant reduction on fasting glucose (WMD: − 3.68 mg/dL, 95% CI: − 5.11, − 2.25, p < 0.00001, I2 = 18%), insulin levels (WMD: − 1.72 µUI/mL, 95% CI: − 2.53, -0.92, p < 0001, I2 = 41%), and HOMA-IR index (WMD: − 0.94, 95% CI: − 1.73, − 0.16, p = 0.02, I2 = 90%) after curcumin therapy. None of the lipid indices were significantly altered by curcumin. Curcumin administration in PCOS resulted in significant improvement in glycaemic parameters; however, no significant changes were seen in lipid parameters with its use.




Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Strowitzki T. Advanced diagnosis of polycystic ovary syndrome-new prediction models with standard parameters. Fertil Steril. 2021;115(1):92–3. https://doi.org/10.1016/j.fertnstert.2020.09.031.
March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544–51.
Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8(1):41. https://doi.org/10.1186/1741-7015-8-41.
Legro RS, Strauss JF III. Molecular progress in infertility: polycystic ovary syndrome. Fertil Steril. 2002;78(3):569–76.
Doi SA, Al-Zaid M, Towers P, Scott C, Al-Shoumer KA. Ovarian steroids modulate neuroendocrine dysfunction in polycystic ovary syndrome. J Endocrinol Invest. 2005;28(1):882–92.
Ndefo UA, Eaton A, Green MR. Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. Pharm Ther. 2013;38(6):336.
Essah PA, Wickham EP, Nestler JE. The metabolic syndrome in polycystic ovary syndrome. Clin Obstet Gynecol. 2007;50(1):205–25.
Garruti G, Depalo R, Vita MG, Lorusso F, Giampetruzzi F, Damato AB, Giorgino F. Adipose tissue, metabolic syndrome and polycystic ovary syndrome: from pathophysiology to treatment. Reprod Biomed Online. 2009;19(4):552–63.
Salley KE, Wickham EP, Cheang KI, Essah PA, Karjane NW, Nestler JE. Position statement: glucose intolerance in polycystic ovary syndrome—a position statement of the Androgen Excess Society. J Clin Endocrinol Metab. 2007;92(12):4546–56.
Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004. 19 (1):41-47. https://doi.org/10.1093/humrep/deh098
Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004. 81 (1):19-25. https://doi.org/10.1016/j.fertnstert.2003.10.004
Domecq JP, Prutsky G, Mullan RJ, Hazem A, Sundaresh V, Elamin MB, Phung OJ, Wang A, Hoeger K, Pasquali R. Lifestyle modification programs in polycystic ovary syndrome: systematic review and meta-analysis. J Clin Endocrinol Metab. 2013;98(12):4655–63.
Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007;370(9588):685–97. https://doi.org/10.1016/s0140-6736(07)61345-2.
Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, Hesson LA, Osei SY, Kaplan R, Stunkard AJ. Randomized trial of lifestyle modification and pharmacotherapy for obesity. N Engl J Med. 2005;353(20):2111–20.
Lua ACY, How CH, King TFJ. Managing polycystic ovary syndrome in primary care. Singapore Med J. 2018;59(11):567–71. https://doi.org/10.11622/smedj.2018135.
Aggarwal BB, Kumar A, Bharti AC. Anticancer potential of curcumin: preclinical and clinical studies. Anticancer Res. 2003;23(1/A):363–98.
Aggarwal BB, Harikumar KB. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol. 2009;41(1):40–59.
Panahi Y, Hosseini MS, Khalili N, Naimi E, Simental-Mendía LE, Majeed M, Sahebkar A. Effects of curcumin on serum cytokine concentrations in subjects with metabolic syndrome: A post-hoc analysis of a randomized controlled trial. Biomed Pharmacother. 2016;82:578–82.
Ghandadi M, Sahebkar A. Curcumin: An effective inhibitor of interleukin-6. Curr Pharm Des. 2017;23(6):921–31. https://doi.org/10.2174/1381612822666161006151605.
Ghasemi F, Shafiee M, Banikazemi Z, Pourhanifeh MH, Khanbabaei H, Shamshirian A, Amiri Moghadam S, ArefNezhad R, Sahebkar A, Avan A, Mirzaei H. Curcumin inhibits NF-kB and Wnt/β-catenin pathways in cervical cancer cells. Pathol Res Prac. 2019;215(10):152556. https://doi.org/10.1016/j.prp.2019.152556.
Panahi Y, Khalili N, Sahebi E, Namazi S, Simental-Mendía LE, Majeed M, Sahebkar A. Effects of Curcuminoids Plus Piperine on Glycemic, Hepatic and Inflammatory Biomarkers in Patients with Type 2 Diabetes Mellitus: A Randomized Double-Blind Placebo-Controlled Trial. Drug Research. 2018;68(7):403–9. https://doi.org/10.1055/s-0044-101752.
Mohajeri M, Bianconi V, Ávila-Rodriguez MF, Barreto GE, Jamialahmadi T, Pirro M, Sahebkar A. Curcumin: a phytochemical modulator of estrogens and androgens in tumors of the reproductive system. Pharmacol Res. 2020;156:104765. https://doi.org/10.1016/j.phrs.2020.104765.
Sadeghian M, Rahmani S, Jamialahmadi T, Johnston TP, Sahebkar A. The effect of oral curcumin supplementation on health-related quality of life: A systematic review and meta-analysis of randomized controlled trials. J Affect Disord. 2021;278:627–36. https://doi.org/10.1016/j.jad.2020.09.091.
Wojcik M, Krawczyk M, Wojcik P, Cypryk K, Wozniak LA. Molecular mechanisms underlying curcumin-mediated therapeutic effects in type 2 diabetes and cancer. Oxid Med Cell Longev. 2018;2018:9698258. https://doi.org/10.1155/2018/9698258.
Shin SK, Ha TY, McGregor RA, Choi MS. Long-term curcumin administration protects against atherosclerosis via hepatic regulation of lipoprotein cholesterol metabolism. Mol Nutr Food Res. 2011;55(12):1829–40.
Heshmati J, Golab F, Morvaridzadeh M, Potter E, Akbari-Fakhrabadi M, Farsi F, Tanbakooei S, Shidfar F. The effects of curcumin supplementation on oxidative stress, Sirtuin-1 and peroxisome proliferator activated receptor γ coactivator 1α gene expression in polycystic ovarian syndrome (PCOS) patients: a randomized placebo-controlled clinical trial. Diabetes Metab Syndr. 2020;14(2):77–82.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Higgins JPT GS, eds. Cochrane Handbook for Systematic Reviews of Interventions. , vol Version 5.0.2. London. 2009
Hozo SPDB, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. https://doi.org/10.1186/1471-2288-5-13.
Sahebkar ACA, Simental-Mendía LE, Aggarwal BB, Gupta SC. Curcumin downregulates human tumor necrosis factor-α levels: A systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2016;107:234–42. https://doi.org/10.1016/j.phrs.2016.03.026.
Serban CSA, Ursoniu S, Mikhailidis DP, Rizzo M, Lip GY, Kees Hovingh G, Kastelein JJ, Kalinowski L, Rysz J, Banach M. A systematic review and meta-analysis of the effect of statins on plasma asymmetric dimethylarginine concentrations. Sci Rep. 2015;5:9902. https://doi.org/10.1038/srep09902.
Asan SABM, Eren B, Karaca E. The effects of curcumin supplementation added to diet on anthropometric and biochemical status in women with polycystic ovary syndrome: A randomized, placebo-controlled trial. Progr Nutr. 2020;22(4):e2020089. https://doi.org/10.23751/pn.v22i4.10460.
Heshmati JMA, Sepidarkish M, Morvaridzadeh M, Salehi M, Palmowski A, Mojtahedi MF, Shidfar F. Effects of curcumin supplementation on blood glucose, insulin resistance and androgens in patients with polycystic ovary syndrome: A randomized double-blind placebo-controlled clinical trial. Phytomedicine. 2021;80:153395. https://doi.org/10.1016/j.phymed.2020.
Jamilian MFF, Kavossian E, Aghadavod E, Shafabakhsh R, Hoseini A, Asemi Z. Effects of curcumin on body weight, glycemic control and serum lipids in women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled trial. Clin Nutr ESPEN. 2020;36:128–33. https://doi.org/10.1016/j.clnesp.2020.01.005.
Sohaei SAR, Tarrahi MJ, Ghasemi-Tehrani H. The effects of curcumin supplementation on glycemic status, lipid profile and hs-CRP levels in overweight/obese women with polycystic ovary syndrome: A randomized, double-blind, placebo-controlled clinical trial. Complement Ther Med. 2019;47:102201. https://doi.org/10.1016/j.ctim.2019.
Sohrevardi SMHB, Azarpazhooh MR, Teymourzadeh M, Simental-Mendía LE, Atkin SL, Sahebkar A, Karimi-Zarchi M. Therapeutic Effect of Curcumin in Women with Polycystic Ovary Syndrome Receiving Metformin: A Randomized Controlled Trial. Adv Exp Med Biol. 2021;1308:109–17. https://doi.org/10.1007/978-3-030-64872-5_9.
Qin S, Huang L, Gong J, Shen S, Huang J, Ren H, Hu H. Efficacy and safety of turmeric and curcumin in lowering blood lipid levels in patients with cardiovascular risk factors: a meta-analysis of randomized controlled trials. Nutr J. 2017;16(1):68. https://doi.org/10.1186/s12937-017-0293-y.
Yang YS, Su YF, Yang HW, Lee YH, Chou JI, Ueng KC. Lipid-lowering effects of curcumin in patients with metabolic syndrome: a randomized, double-blind, placebo-controlled trial. Phytother Res. 2014;28(12):1770–7. https://doi.org/10.1002/ptr.5197.
Hasan ST, Zingg JM, Kwan P, Noble T, Smith D, Meydani M. Curcumin modulation of high fat diet-induced atherosclerosis and steatohepatosis in LDL receptor deficient mice. Atherosclerosis. 2014;232(1):40–51. https://doi.org/10.1016/j.atherosclerosis.2013.10.016.
Legro RSKA, Dunaif A. Prevalence and predictors of dyslipidemia in women with polycystic ovary syndrome. Am J Med. 2001;111(8):607–13. https://doi.org/10.1016/s0002-9343(01)00948-2.
Wild RARM, Clifton S, Carmina E. Lipid levels in polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril. 2011;95(3):1073–9. https://doi.org/10.1016/j.fertnstert.2010.12.027.
LE Simental-Mendía PM, Gotto AM Jr, Banach M, Atkin SL, Majeed M, Sahebkar A. Lipid-modifying activity of curcuminoids: A systematic review and meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2019;59(7):1178–87. https://doi.org/10.1080/10408398.2017.1396201.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
Muhammed Majeed is the founder of Sabinsa Corporation and Sami Labs Ltd. Other authors have no conflicting interests to disclose.
Rights and permissions
About this article
Cite this article
Simental-Mendía, L.E., Shah, N., Sathyapalan, T. et al. Effect of Curcumin on Glycaemic and Lipid Parameters in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Reprod. Sci. 29, 3124–3133 (2022). https://doi.org/10.1007/s43032-021-00761-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00761-6