Abstract
Background
Higher socioeconomic status (SES) has less impact on cardio-metabolic disease and preterm birth risk among Black women compared to White women, an effect called “diminishing returns.” No studies have tested whether this also occurs for pregnancy cardio-metabolic disease, specifically preeclampsia, or whether preeclampsia risk could account for race-by-SES disparities in birth timing.
Methods
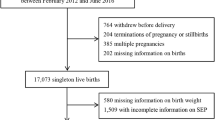
A sample of 718,604 Black and White women was drawn from a population-based California cohort of singleton births. Education, public health insurance status, gestational length, and preeclampsia diagnosis were extracted from a State-maintained birth cohort database. Age, prenatal care, diabetes diagnosis, smoking during pregnancy, and pre-pregnancy body mass index were covariates.
Results
In logistic regression models predicting preeclampsia risk, the race-by-SES interaction (for both education and insurance status) was significant. White women were at lower risk for preeclampsia, and higher SES further reduced risk. Black women were at higher risk for preeclampsia, and SES did not attenuate risk. In pathway analyses predicting gestational length, an indirect effect of the race-by-SES interaction was observed. Among White women, higher SES predicted lower preeclampsia risk, which in turn predicted longer gestation. The same was not observed for Black women.
Conclusions
Compared to White women, Black women had increased preeclampsia risk. Higher SES attenuated risk for preeclampsia among White women, but not for Black women. Similarly, higher SES indirectly predicted longer gestational length via reduced preeclampsia risk among White women, but not for Black women. These findings are consistent with diminishing returns of higher SES for Black women with respect to preeclampsia.



Similar content being viewed by others
Notes
Both White and Black categories include women born in and outside the USA.
References
Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33(3):130–7. https://doi.org/10.1053/j.semperi.2009.02.010.
Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365(9461):785–99. https://doi.org/10.1016/s0140-6736(05)71003-5.
Esakoff TF, Rad S, Burwick RM, Caughey AB. Predictors of eclampsia in California. J Matern Fetal Neonatal Med. 2016;29(10):1531–5. https://doi.org/10.3109/14767058.2015.1057489.
Savitz DA, Danilack VA, Engel SM, Elston B, Lipkind HS. Descriptive epidemiology of chronic hypertension, gestational hypertension, and preeclampsia in New York State, 1995-2004. Matern Child Health J. 2014;18(4):829–38. https://doi.org/10.1007/s10995-013-1307-9.
Eskenazi B, Fenster L, Sidney S. A multivariate analysis of risk factors for preeclampsia. JAMA. 1991;266(2):237–41.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–44. https://doi.org/10.1016/S0140-6736(10)60279-6.
Silva LM, Coolman M, Steegers EA, Jaddoe VW, Moll HA, Hofman A, et al. Low socioeconomic status is a risk factor for preeclampsia: the Generation R Study. J Hypertens. 2008;26:1200–8.
Reeves R, Rodrigue E, Kneebone E. Five evils: multidimensional poverty and race in America. Washington, DC: Brookings Institute; 2016.
Kelly UA. Integrating intersectionality and biomedicine in health disparities research. ANS Adv Nurs Sci. 2009;32(2):E42–56. https://doi.org/10.1097/ANS.0b013e3181a3b3fc.
Hogan VK, de Araujo EM, Caldwell KL, Gonzalez-Nahm SN, Black KZ. “We black women have to kill a lion everyday”: an intersectional analysis of racism and social determinants of health in Brazil. Soc Sci Med. 2018;199:96–105. https://doi.org/10.1016/j.socscimed.2017.07.008.
Fuller-Rowell TE, Curtis DS, Doan SN, Coe CL. Racial disparities in the health benefits of educational attainment: a study of inflammatory trajectories among African American and white adults. Psychosom Med. 2015;77(1):33–40. https://doi.org/10.1097/PSY.0000000000000128.
Assari S, Nikahd A, Malekahmadi MR, Lankarani MM, Zamanian H. Race by gender group differences in the protective effects of socioeconomic factors against sustained health problems across five domains. J Racial Ethn Health Disparities. 2016;4:884–94. https://doi.org/10.1007/s40615-016-0291-3.
Ross KM, Guardino C, Dunkel Schetter C, Hobel CJ. Interactions between race/ethnicity, poverty status, and pregnancy cardio-metabolic diseases in prediction of postpartum cardio-metabolic health. Ethn Health 2018;1–16. https://doi.org/10.1080/13557858.2018.1493433.
Assari S. Health disparities due to diminished return among Black Americans: public policy solutions. Soc Iss Policy Rev. 2018;12:112–45.
Assari S. Unequal gain of equal resources across racial groups. Int J Health Policy Manag. 2017;7(1):1–9. https://doi.org/10.15171/ijhpm.2017.90.
Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–86.
Assari S, Lankarani MM. Race and urbanity alter the protective effect of education but not income on mortality. Front Public Health. 2016;4:100. https://doi.org/10.3389/fpubh.2016.00100.
Everett BG, Rehkopf DH, Rogers RG. The nonlinear relationship between education and mortality: an examination of cohort, race/ethnic, and gender differences. Popul Res Policy Rev. 2013;32(6). https://doi.org/10.1007/s11113-013-9299-0.
Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and U.S. adult mortality: implications for understanding education’s causal influence. Soc Sci Med. 2015;127:8–18. https://doi.org/10.1016/j.socscimed.2014.11.024.
Assari S. Life expectancy gain due to employment status depends on race, gender, education, and their intersections. J Racial Ethn Health Disparities. 2018;5(2):375–86. https://doi.org/10.1007/s40615-017-0381-x.
Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. https://doi.org/10.1016/j.socscimed.2004.04.026.
Holmes CJ, Zajacova A. Education as “the great equalizer”: health benefits for Black and White adults. Soc Sci Q. 2014;n/a–n/a. https://doi.org/10.1111/ssqu.12092.
Cene CW, Halladay JR, Gizlice Z, Roedersheimer K, Hinderliter A, Cummings DM, et al. Associations between subjective social status and physical and mental health functioning among patients with hypertension. J Health Psychol. 2015;21:2624–35. https://doi.org/10.1177/1359105315581514.
Assari S. Ethnic and gender differences in additive effects of socio-economics, psychiatric disorders, and subjective religiosity on suicidal ideation among blacks. Int J Prev Med. 2015;6:53. https://doi.org/10.4103/2008-7802.158913.
Hudson DL, Bullard KM, Neighbors HW, Geronimus AT, Yang J, Jackson JS. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? J Mens Health. 2012;9(2):127–36. https://doi.org/10.1016/j.jomh.2012.03.006.
Kubzansky LD, Berkman LF, Seeman TE. Social conditions and distress in elderly persons: findings from the MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2000;55(4):P238–46.
Assari S, Thomas A, Caldwell CH, Mincy RB. Blacks’ diminished health return of family structure and socioeconomic status; 15 years of follow-up of a national urban sample of youth. J Urban Health. 2018;95(1):21–35. https://doi.org/10.1007/s11524-017-0217-3.
Geronimus AT, Pearson JA, Linnenbringer E, Schulz AJ, Reyes AG, Epel ES, et al. Race-ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. J Health Soc Behav. 2015;56(2):199–224. https://doi.org/10.1177/0022146515582100.
Paul K, Boutain D, Agnew K, Thomas J, Hitti J. The relationship between racial identity, income, stress and C-reactive protein among parous women: implications for preterm birth disparity research. J Natl Med Assoc. 2008;100(5):540–6. https://doi.org/10.1016/s0027-9684(15)31300-6.
Beach SR, Lei MK, Brody GH, Kim S, Barton AW, Dogan MV, et al. Parenting, socioeconomic status risk, and later young adult health: exploration of opposing indirect effects via DNA methylation. Child Dev. 2016;87(1):111–21. https://doi.org/10.1111/cdev.12486.
Brody GH, Yu T, Chen E, Miller GE, Kogan SM, Beach SR. Is resilience only skin deep?: rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychol Sci. 2013;24:1285–93.
Wang JT, Wiebe DJ, White PC. Developmental trajectories of metabolic control among White, Black, and Hispanic youth with type 1 diabetes. J Pediatr. 2011;159(4):571–6. https://doi.org/10.1016/j.jpeds.2011.03.053.
LaVeist TA, Thorpe RJ Jr, Galarraga JE, Bower KM, Gary-Webb TL. Environmental and socio-economic factors as contributors to racial disparities in diabetes prevalence. J Gen Intern Med. 2009;24(10):1144–8. https://doi.org/10.1007/s11606-009-1085-7.
Gaillard TR, Schuster DP, Bossetti BM, Green PA, Osei K. Do sociodemographics and economic status predict risks for type II diabetes in African Americans? Diab Educ. 1997;23:294–300.
Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol. 2011;174(5):537–45. https://doi.org/10.1093/aje/kwr116.
Thorpe RJ Jr, Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study. Soc Sci Med. 2008;67(10):1604–11. https://doi.org/10.1016/j.socscimed.2008.07.002.
Maynard JW, Fang H, Petri M. Low socioeconomic status is associated with cardiovascular risk factors and outcomes in systemic lupus erythematosus. J Rheumatol. 2012;39(4):777–83. https://doi.org/10.3899/jrheum.110724.
Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–72. https://doi.org/10.1016/j.amepre.2010.05.012.
Culhane JF, Goldenberg RL. Racial disparities in preterm birth. Semin Perinatol. 2011;35(4):234–9. https://doi.org/10.1053/j.semperi.2011.02.020.
Ahern J, Pickett KE, Abrams B. Preterm birth among African American and White women: a multilevel analysis of socioeconomic characteristics and cigarette smoking. J Epidemiol Community Health. 2003;57:606–11.
Braveman PA, Heck K, Egerter S, Marchi KS, Dominguez TP, Cubbin C, et al. The role of socioeconomic factors in Black-White disparities in preterm birth. Am J Public Health. 2015;105(4):694–702. https://doi.org/10.2105/AJPH.2014.302008.
Lieberman E, Ryan KJ, Monson RR, Schoenbaum SC. Risk factors accounting for racial differences in the rate of premature birth. N Engl J Med. 1987;317(12):743–8. https://doi.org/10.1056/NEJM198709173171206.
Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–62. https://doi.org/10.1007/s11524-006-9094-x.
Messer LC, Kaufman JS, Dole N, Savitz DA, Laraia BA. Neighborhood crime, deprivation, and preterm birth. Ann Epidemiol. 2006;16(6):455–62. https://doi.org/10.1016/j.annepidem.2005.08.006.
Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med. 2005;60(10):2217–28. https://doi.org/10.1016/j.socscimed.2004.10.010.
Schempf AH, Kaufman JS, Messer LC, Mendola P. The neighborhood contribution to black-white perinatal disparities: an example from two north Carolina counties, 1999-2001. Am J Epidemiol. 2011;174(6):744–52. https://doi.org/10.1093/aje/kwr128.
Collins JW Jr, Hammond NA. Relation of maternal race to the risk of preterm, non-low birth weight infants: a population study. Am J Epidemiol. 1996;143(4):333–7.
Pickett KE, Ahern JE, Selvin S, Abrams B. Neighborhood socioeconomic status, maternal race and preterm delivery: a case-control study. Ann Epidemiol. 2002;12(6):410–8.
Savitz DA, Kaufman JS, Dole N, Siega-Riz AM, Thorp JM Jr, Kaczor DT. Poverty, education, race, and pregnancy outcome. Eth Dis. 2004;14(3):322–9.
Collins JW Jr, David RJ, Simon DM, Prachand NG. Preterm birth among African American and White women with a lifelong residence in high-income Chicago neighborhoods: an exploratory study. Ethn Dis. 2007;17:113–7.
Slaughter-Acey JC, Holzman C, Calloway D, Tian Y. Movin’ on up: socioeconomic mobility and the risk of delivering a small-for-gestational age infant. Matern Child Health J. 2016;20(3):613–22. https://doi.org/10.1007/s10995-015-1860-5.
Colen CG, Geronimus AT, Bound J, James SA. Maternal upward socioeconomic mobility and black-white disparities in infant birthweight. Am J Public Health. 2006;96(11):2032–9. https://doi.org/10.2105/AJPH.2005.076547.
Gorman BK. Racial and ethnic variation in low birthweight in the United States: individual and contextual determinants. Health Place. 1999;5(3):195–207.
Parker JD, Schoendorf K, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann Epidemiol. 1994;4:271–8.
Schoendorf K, Hogue CJ, Kleinman JC, Rowley D. Mortality among infants of Black as compared to White college-educated parents. N Engl J Med. 1992;326:1522–6.
Starfield B, Shapiro S, Weiss J, Liang KY, Ra K, Paige D, et al. Race, family income, and low birth weight. Am J Epidemiol. 1991;134(10):1167–74.
Singh GK, Yu SM. Infant mortality in the United States: trends, differentials, and projections, 1950 through 2010. Am J Public Health. 1995;85:957–64.
Castrillio SM, Rankin KM, David RJ, Collins JW Jr. Small-for-gestational age and preterm birth across generations: a population-based study of Illinois births. Matern Child Health J. 2014;18(10):2456–64. https://doi.org/10.1007/s10995-014-1484-1.
Collins JW, Simon DM, Jackson TA, Drolet A. Advancing maternal age and infant birth weight among urban African Americans: the effect of neighborhood poverty. Ethn Dis. 2006;16:180–6.
Collins JW Jr, Rankin KM, David RJ. African American women’s lifetime upward economic mobility and preterm birth: the effect of fetal programming. Am J Public Health. 2011;101(4):714–9. https://doi.org/10.2105/AJPH.2010.195024.
Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175(5):1317–24. https://doi.org/10.1016/S0002-9378(96)70048-0.
Jaffee KD, Perloff JD. An ecological analysis of racial differences in low birthweight: implications for maternal and child health social work. Health Soc Work. 2003;28(1):9–22.
Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med. 2007;65(12):2440–57. https://doi.org/10.1016/j.socscimed.2007.07.014.
Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. Am J Public Health. 2001;91(11):1808–14. https://doi.org/10.2105/Ajph.91.11.1808.
Rauh VA, Andrews HF, Garfinkel RS. The contribution of maternal age to racial disparities in birthweight: a multilevel perspective. Am J Public Health. 2001;91(11):1815–24.
Sparks PJ. Do biological, sociodemographic, and behavioral characteristics explain racial/ethnic disparities in preterm births? Soc Sci Med. 2009;68(9):1667–75. https://doi.org/10.1016/j.socscimed.2009.02.026.
Hedderson M. Gestational diabetes mellitus and lesser degrees of pregnancy hyperglycemia: association with increased risk of spontaneous preterm birth. Obstet Gynecol. 2003;102(4):850–6. https://doi.org/10.1016/s0029-7844(03)00661-6.
Xiong X, Saunders LD, Wang FL, Demianczuk NN. Gestational diabetes mellitus: prevalence, risk factors, maternal and infant outcomes. Int J Gynaecol Obstet. 2001;75(3):221–8.
Hendricks CH. Delivery patterns and reproductive efficiency among groups of differing socioeconomic status and ethnic origins. AJOG. 1967;97(5):608–24.
Baer RJ, Altman MR, Oltman SP, Ryckman KK, Chambers CD, Rand L, et al. Maternal factors influencing late entry into prenatal care: a stratified analysis by race or ethnicity and insurance status. J Matern Fetal Neonatal Med. 2018;32:1–7. https://doi.org/10.1080/14767058.2018.1463366.
Baer RJ, Chambers CD, Bandoli G, Jelliffe-Pawlowski LL. Risk of preterm birth by subtype among Medi-Cal participants with mental illness. Am J Obstet Gynecol. 2016;215(4):519 e1–9. https://doi.org/10.1016/j.ajog.2016.06.017.
American Medical Association. International Classification of Diseases: ICD-9-CM. Chicago: American Medical Association; 2008.
IBM Corp. IBM SPSS Statistics for Windows, Version 24.0. IBM Corp: Armonk; 2016.
Rosseel Y. lavaan : an R package for structural equation modeling. J Stat Softw. 2012;48:ePub.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2014.
Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Ann Rev Public Health. 2008;29:235–52. https://doi.org/10.1146/annurev.publhealth.29.020907.090852.
Colen CG, Ramey DM, Cooksey EC, Williams DR. Racial disparities in health among nonpoor African Americans and Hispanics: the role of acute and chronic discrimination. Soc Sci Med. 2018;199:167–80. https://doi.org/10.1016/j.socscimed.2017.04.051.
Hudson DL, Neighbors HW, Geronimus AT, Jackson JS. Racial discrimination, John Henryism, and depression among African Americans. J Black Psychol. 2016;42(3):221–43. https://doi.org/10.1177/0095798414567757.
Tyson K, Darity W Jr, Castellino DR. It’s not “a Black thing”: understanding the burden of acting White and other dilemmas of high achievement. Am Sociol Rev. 2005;70:582–605.
Jones CP. Levels of racism: a theoretic framework and a Gardener’s tale. Am J Public Health. 2000;90:1212–5.
Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21(1):55–89. https://doi.org/10.1210/er.21.1.55.
Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nat Rev Immunol. 2011;11(9):625–32. https://doi.org/10.1038/nri3042.
Chae DH, Clouston S, Martz CD, Hatzenbuehler ML, Cooper HLF, Turpin R, et al. Area racism and birth outcomes among Blacks in the United States. Soc Sci Med. 2018;199:49–55. https://doi.org/10.1016/j.socscimed.2017.04.019.
Kothari CL, Paul R, Dormitorio B, Ospina F, James A, Lenz D, et al. The interplay of race, socioeconomic status and neighborhood residence upon birth outcomes in a high black infant mortality community. SSM Popul Health. 2016;2:859–67. https://doi.org/10.1016/j.ssmph.2016.09.011.
McCluney CL, Schmitz LL, Hicken MT, Sonnega A. Structural racism in the workplace: does perception matter for health inequalities? Soc Sci Med. 2018;199:106–14. https://doi.org/10.1016/j.socscimed.2017.05.039.
Hicken MT, Kravitz-Wirtz N, Durkee M, Jackson JS. Racial inequalities in health: framing future research. Soc Sci Med. 2018;199:11–8. https://doi.org/10.1016/j.socscimed.2017.12.027.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–29. https://doi.org/10.1016/j.socscimed.2017.05.009.
James SA. John Henryism and the health of African Americans. In: LaVeist T, editor. Race, ethnicity, and health. San Francisco: Jossey-Bass; 2002.
Miller GE, Cohen S, Janicki-Deverts D, Brody GH, Chen E. Viral challenge reveals further evidence of skin-deep resilience in African Americans from disadvantaged backgrounds. Health Psychol. 2016;35(11):1225–34. https://doi.org/10.1037/hea0000398.
Hicken MT, Lee H, Hing AK. The weight of racism: vigilance and racial inequalities in weight-related measures. Soc Sci Med. 2018;199:157–66. https://doi.org/10.1016/j.socscimed.2017.03.058.
Dunkel Schetter C. Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol. 2011;62:531–58. https://doi.org/10.1146/annurev.psych.031809.130727.
Acknowledgments
This project was supported by University of California San Francisco California Preterm Birth Initiative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Ross, K.M., Dunkel Schetter, C., McLemore, M.R. et al. Socioeconomic Status, Preeclampsia Risk and Gestational Length in Black and White Women. J. Racial and Ethnic Health Disparities 6, 1182–1191 (2019). https://doi.org/10.1007/s40615-019-00619-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-019-00619-3