Abstract
Background and aim
Sauna-type bathing has increased worldwide, and it has been related to both harmful and beneficial effects. There are few studies of bathing in sauna in very old age.
Methods
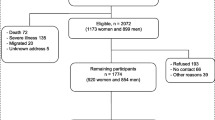
The series consists of 524 mostly home-living survivors of the Helsinki Businessmen Study (HBS, mean age 86 years, range 80–95), who in 2015 responded to a questionnaire survey about lifestyle (including sauna bathing), prevalent diseases, and health-related quality of life (HRQoL, RAND-36).
Results
Of the men 57.6% (n = 302) reported all-year round and 17.6% (n = 92) part-year sauna bathing. Sauna was currently used mostly once a week, but 10% bathed more than twice a week. Median time in the hot room was 15 min at 80 °C. Among 45.7% of the men, the habit had decreased with ageing, and 130 (24.8%) did not attend sauna. However, 92.2% of the latter had discontinued an earlier habit, respective proportions 20.7% and 75.0% among all-year and part-year users. Overall, reasons for decreased sauna bathing were nonspecific or related to mobility problems or diverse health reasons (n = 63). The most frequent motivations for sauna were relaxation and hygienic reasons. Of the RAND-36 domains physical function, vitality, social functioning, and general health were significantly better among sauna users than non-users. These differences partly remained after adjusting for prevalent diseases and mobility-disability.
Conclusions
Regular sauna bathing was common among octogenarian men and was associated with better HRQoL. However, reverse causality must be taken into account in this cross-sectional study. The bathing habit seemed to be prudent and had decreased in almost half of the cohort.
Similar content being viewed by others
References
Hooper PL (1999) Hot-tub therapy for type 2 diabetes mellitus. N Engl Med 341:924–925
Crandall CG, González-Alonso J (2010) Cardiovascular function in the heat stressed human. Acta Physiol [Oxf] 199:407–423. https://doi.org/10.1111/j.1748-1716.2010.02119.x
Brunt VE, Howard MJ, Francisco MA et al (2016) Passive heat therapy improves endothelial function, arterial stiffness and blood pressure in sedentary humans. J Physiol 18:5329–5342
Hooper PL, Balogh G, Rivas E et al (2014) The importance of the cellular stress response in the pathogenesis and treatment of type 2 diabetes. Cell Stress Chaperones 19:447–464
Gagnon D, Romero SA, Ngo H et al (2016) Healthy aging does not compromise the augmentation of cardiac function during heat stress. J Appl Physiol 121:885–892. https://doi.org/10.1152/japplphysiol.00643.2016
Brunt VE, Eymann TM, Francisco MA et al (2016) Passive heat therapy improves cutaneous microvascular function in sedentary humans via improved nitric oxide-dependent dilation. J Appl Physiol 121:716–723. https://doi.org/10.1152/japplphysiol.00424.2016
Romero SA, Gagnon D, Adams A et al (2016) Acute limb heating improves macro- and microvascular dilator function in the leg of aged humans. Am J Physiol Heart Circ Physiol 312:H89–H97. https://doi.org/10.1152/ajpheart.00519 2017.
McGinn R, Poirier MP, Kenny GP (2017) Using heat as a therapeutic tool for the aging vascular tree. Am J Physiol Heart Circ Physiol 312:H806–H807. https://doi.org/10.1152/ajpheart.00519.2016
Kenny GP, Poirier MP, Metsios GS et al (2017) Hyperthermia and cardiovascular strain during an extreme heat exposure in young versus older adults. Temperature 4:79–88. https://doi.org/10.1080/23328940.2016.1230171
Romo M (1976) Heart attacks and the sauna. Lancet 313:809
Cooperman EM (1978) The sauna: a health hazard? CMAJ 118:1024
Hawkins C (1987) The sauna: killer or healer? Br Med J 295:1015–1016
Luurila OJ (1978) Cardiac arrhythmias, sudden death and the Finnish sauna bath. Adv Cardiol 25:73–81
Eisalo A, Luurila OJ (1988) The Finnish sauna and cardiovascular diseases. Ann Clin Res 20:267–270
Kukkonen-Harjula K, Kauppinen K (2006) Health effects and risks of sauna bathing. Int J Circumpolar Health 65:195–205
Hannuksela M, Ellahham S (2001) Benefits and risks of sauna bathing. Am J Med 110:118–126
Laukkanen T, Khan H, Zaccardi F et al (2015) Association between sauna bathing and fatal cardiovascular and all-cause mortality events. JAMA Intern Med 175:542–548
Zaccardi F, Laukkanen T, Willeit P et al (2017) Sauna bathing and incident hypertension: a prospective cohort study. Am J Hypertens. https://doi.org/10.1093/ajh/hpx102 (Epub ahead of print)
Laukkanen T, Kunutsor S, Kauhanen J et al (2017) Sauna bathing is inversely associated with dementia and Alzheimer’s disease in middle-aged Finnish men. Age Ageing 46:245–249
Krause M, Ludwig MS, Heck TG et al (2015) Heat shock proteins and heat therapy for type 2 diabetes: pros and cons. Curr Opin Clin Nutr Metab Care 18:374–380
Strandberg TE, Salomaa V, Strandberg AY et al (2016) Cohort profile: the Helsinki businessmen study [HBS]. Int J Epidemiol 45:1074–1074h
Aalto AM, Aro AR, Teperi J (1999) RAND-36 as a measure of health-related quality of life. Reliability, construct validity and reference values in the Finnish general population. Stakes, Research Reports, Helsinki No. 101
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33:350–357
Koljonen V (2009) Hot air sauna burns—review of their etiology and treatment. J Burn Care Res 30:705–710
Redberg R (2015) Health benefits of sauna bathing. JAMA Intern Med 175:548
Kivimäki M, Virtanen M, Ferrie JE (2015) The link between sauna bathing and mortality may be noncausal. JAMA Intern Med 175:1718
Epstein Y, Schoenfeld Y (2015) The link between sauna bathing and mortality may be noncausal. JAMA Intern Med 175:1718–1719
Gryka D, Pilch W, Szarek M et al (2014) The effect of sauna bathing on lipid profile in young, physically active, male subjects. Int J Occupat Med Environ Health 14:27:608–618
Cornelius C, Perrotta R, Graziano A et al (2013) Stress responses, vitagenes and hormesis as critical determinants in aging and longevity: mitochondria as a “chi”. Immunity Ageing 10:15
Tei C, Horikiri Y, Park JC et al (1995) Acute hemodynamic improvement by thermal vasodilation in congestive heart failure. Circulation 91:2582–2590
Kihara T, Biro S, Imamura M et al (2002) Repeated sauna treatment improves vascular endothelial and cardiac function in patients with chronic heart failure. J Am Coll Cardiol 39:754–759. https://doi.org/10.1016/S0735-1097[01]01824-1
Kihara T, Miyata M, Fukudome T et al (2009) Waon therapy improves the prognosis of patients with chronic heart failure. J Cardiol 53:214–218. https://doi.org/10.1016/j.jjcc.2008.11.005
Kuwahata S, Miyata M, Fujita S et al (2011) Improvement of autonomic nervous activity by Waon therapy in patients with chronic heart failure. J Cardiol 57:100–106. https://doi.org/10.1016/j.jjcc.2010.08.005
Sobajima M, Nozawa T, Fukui Y et al (2015) Waon therapy improves quality of life as well as cardiac function and exercise capacity in patients with chronic heart failure. Int Heart J 56:203–208. https://doi.org/10.1536/ihj.14-266
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Helsinki University Hospital [Valtion tutkimusrahoitus TYH2014 and TYH2015 to T.E.S], and Academy of Finland (Grant 311492).
Conflict of interest
The authors report no conflicts of interest.
Ethical approval
The Helsinki Businessmen Study had ethical approval from the Ethics Committee of the Department of Medicine, Helsinki University Hospital.
Statement of human and animal rights
All procedures performed in this study involving human participants were in accordance with the ethical approval and standards of the institutional research committee.
Informed consent
All participants gave written informed consent.
Rights and permissions
About this article
Cite this article
Strandberg, T.E., Strandberg, A., Pitkälä, K. et al. Sauna bathing, health, and quality of life among octogenarian men: the Helsinki Businessmen Study. Aging Clin Exp Res 30, 1053–1057 (2018). https://doi.org/10.1007/s40520-017-0855-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0855-z