Abstract
Topic
The purpose of the review was to identify structural, functional, blood-based, and other types of biomarkers for early, intermediate, and late nonexudative stages of age-related macular degeneration (AMD) and summarize the relevant data for proof-of-concept clinical trials.
Clinical relevance
AMD is a leading cause of blindness in the aging population, yet no treatments exist for its most common nonexudative form. There are limited data on the diagnosis and progression of nonexudative AMD compared to neovascular AMD. Our objective was to provide a comprehensive, systematic review of recently published biomarkers (molecular, structural, and functional) for early AMD, intermediate AMD, and geographic atrophy and to evaluate the relevance of these biomarkers for use in future clinical trials.
Methods
A literature search of PubMed, ScienceDirect, EMBASE, and Web of Science from January 1, 1996 to November 30, 2020 and a patent search were conducted. Search terms included “early AMD,” “dry AMD,” “intermediate AMD,” “biomarkers for nonexudative AMD,” “fundus autofluorescence patterns,” “color fundus photography,” “dark adaptation,” and “microperimetry.” Articles were assessed for bias and quality with the Mixed-Methods Appraisal Tool. A total of 94 articles were included (61,842 individuals).
Results
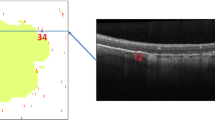
Spectral-domain optical coherence tomography was superior at highlighting detailed structural changes in earlier stages of AMD. Fundus autofluorescence patterns were found to be most important in estimating progression of geographic atrophy. Delayed rod intercept time on dark adaptation was the most widely recommended surrogate functional endpoint for early AMD, while retinal sensitivity on microperimetry was most relevant for intermediate AMD. Combinational studies accounting for various patient characteristics and machine/deep-learning approaches were best suited for assessing individualized risk of AMD onset and progression.
Conclusion
This systematic review supports the use of structural and functional biomarkers in early AMD and intermediate AMD, which are more reproducible and less invasive than the other classes of biomarkers described. The use of deep learning and combinational algorithms will gain increasing importance in future clinical trials of nonexudative AMD.

Similar content being viewed by others
References
Wong WL, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob Heal. 2014;2(2):e106–16. https://doi.org/10.1016/S2214-109X(13)70145-1.
Pennington KL, DeAngelis MM. Epidemiology of age-related macular degeneration (AMD): associations with cardiovascular disease phenotypes and lipid factors. Eye Vis. 2016. https://doi.org/10.1186/s40662-016-0063-5.
Hageman GS, Gehrs K, Johnson LV, Anderson D. Age-related macular degeneration (AMD). University of Utah Health Sciences Center; 1995.
Ferris FL, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013;120(4):844–51. https://doi.org/10.1016/j.ophtha.2012.10.036.
Carnevali A, et al. Retinal microcirculation abnormalities in patients with systemic sclerosis: an explorative optical coherence tomography angiography study. Rheumatology. 2021. https://doi.org/10.1093/rheumatology/keab258.
Vujosevic S, Smolek MK, Lebow KA, Notaroberto N, Pallikaris A, Casciano M. Detection of macular function changes in early (AREDS 2) and intermediate (AREDS 3) age-related macular degeneration. Ophthalmologica. 2011;225(3):155–60. https://doi.org/10.1159/000320340.
Chew EY, et al. Long-term effects of vitamins C and E, β-carotene, and zinc on age-related macular degeneration: AREDS Report No. 35. Ophthalmology. 2013;120(8):1604. https://doi.org/10.1016/j.ophtha.2013.01.021.
Plyukhova AA, et al. Comparative safety of bevacizumab, ranibizumab, and aflibercept for treatment of neovascular age-related macular degeneration (AMD): A systematic review and network meta-analysis of direct comparative studies. J Clin Med. 2020;9(5):1522. https://doi.org/10.3390/jcm9051522.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Ann Intern Med. 2009;151(4):264. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
Nha Hong Q, et al. Mixed Methods Appraisal Tool (MMAT) version 2018 User guide. 2019. [Online]. http://mixedmethodsappraisaltoolpublic.pbworks.com/. Accessed: 20 Dec 2019.
Howells K, Sarkar M, Fletcher D. Can athletes benefit from difficulty? A systematic review of growth following adversity in competitive sport. Progress Brain Res. 2017;234:117–59.
Feeny AK, Tadarati M, Freund DE, Bressler NM, Burlina P. Automated segmentation of geographic atrophy of the retinal epithelium via random forests in AREDS color fundus images. Comput Biol Med. 2015;65:124–36. https://doi.org/10.1016/J.COMPBIOMED.2015.06.018.
Yu JJ, et al. Natural history of drusenoid pigment epithelial detachment associated with age-related macular degeneration: age-related eye disease study 2 report no. 17. Ophthalmology. 2019;126(2):261–73. https://doi.org/10.1016/J.OPHTHA.2018.08.017.
Yan YN, Wang YX, Xu L, Xu J, Bin Wei W, Jonas JB. Fundus tessellation: prevalence and associated factors: the Beijing Eye Study 2011. Ophthalmology. 2015;122(9):1873–80. https://doi.org/10.1016/J.OPHTHA.2015.05.031.
Jain N, et al. Quantitative comparison of Drusen segmented on SD-OCT versus Drusen delineated on color fundus photographs. Invest Ophthalmol Vis Sci. 2010;51(10):4875–83. https://doi.org/10.1167/iovs.09-4962.
Klein R, Klein BEK, Knudtson MD, Meuer SM, Swift M, Gangnon RE. Fifteen-year cumulative incidence of age-related macular degeneration. The Beaver Dam Eye Study. Ophthalmology. 2007;114(2):253–62. https://doi.org/10.1016/j.ophtha.2006.10.040.
Chisari CG, et al. Retinal nerve fiber layer thickness and higher relapse frequency may predict poor recovery after optic neuritis in MS patients. J Clin Med. 2019;8(11):2022. https://doi.org/10.3390/jcm8112022.
Reibaldi M, et al. Intrasession reproducibility of RNFL Thickness measurements using SD-OCT in eyes with keratoconus. Ophthalmic Surg Lasers Imaging. 2012. https://doi.org/10.3928/15428877-20121001-04.
Leuschen JN, et al. Spectral-domain optical coherence tomography characteristics of intermediate age-related macular degeneration. Ophthalmology. 2013;120(1):140–50. https://doi.org/10.1016/J.OPHTHA.2012.07.004.
Christenbury JG, et al. Progression of intermediate age-related macular degeneration with proliferation and inner retinal migration of hyperreflective foci. Ophthalmology. 2013;120(5):1038–45. https://doi.org/10.1016/j.ophtha.2012.10.018.
Veerappan M, et al. Optical coherence tomography reflective Drusen substructures predict progression to geographic atrophy in age-related macular degeneration. Ophthalmology. 2016;123(12):2554–70. https://doi.org/10.1016/j.ophtha.2016.08.047.
de Sisternes L, Simon N, Tibshirani R, Leng T, Rubin DL. Quantitative SD-OCT Imaging Biomarkers as Indicators of Age-Related Macular Degeneration Progression. Investig Opthalmology Vis Sci. 2014;55(11):7093. https://doi.org/10.1167/iovs.14-14918.
Niu S, de Sisternes L, Chen Q, Rubin DL, Leng T. Fully automated prediction of geographic atrophy growth using quantitative spectral-domain optical coherence tomography biomarkers. Ophthalmology. 2016;123(8):1737–50. https://doi.org/10.1016/J.OPHTHA.2016.04.042.
Dolz-Marco R, Balaratnasingam C, Gattoussi S, Ahn S, Yannuzzi LA, Freund KB. Long-term choroidal thickness changes in eyes with Drusenoid pigment epithelium detachment. Am J Ophthalmol. 2018;191:23–33. https://doi.org/10.1016/J.AJO.2018.03.038.
Schuman SG, Koreishi AF, Farsiu S, Jung SH, Izatt JA, Toth CA. Photoreceptor layer thinning over drusen in eyes with age-related macular degeneration imaged in vivo with spectral-domain optical coherence tomography. Ophthalmology. 2009;116(3):488–496.e2. https://doi.org/10.1016/j.ophtha.2008.10.006
Folgar FA, et al. Drusen volume and retinal pigment epithelium abnormal thinning volume predict 2-year progression of age-related macular degeneration. Ophthalmology. 2016;123(1):39-50.e1. https://doi.org/10.1016/J.OPHTHA.2015.09.016.
Sleiman K, et al. Optical coherence tomography predictors of risk for progression to non-neovascular atrophic age-related macular degeneration. Ophthalmology. 2017;124(12):1764–77. https://doi.org/10.1016/J.OPHTHA.2017.06.032.
Wu Z, et al. Optical coherence tomography-defined changes preceding the development of Drusen-associated atrophy in age-related macular degeneration. Ophthalmology. 2014;121(12):2415–22. https://doi.org/10.1016/J.OPHTHA.2014.06.034.
Farsiu S, et al. Quantitative classification of eyes with and without intermediate age-related macular degeneration using optical coherence tomography. Ophthalmology. 2014;121(1):162–72. https://doi.org/10.1016/J.OPHTHA.2013.07.013.
Sevilla MB, et al. Relating retinal morphology and function in aging and early to intermediate age-related macular degeneration subjects. Am J Ophthalmol. 2016;165:65–77. https://doi.org/10.1016/J.AJO.2016.02.021.
Thiele S, et al. Prognostic value of retinal layers in comparison with other risk factors for conversion of intermediate age-related macular degeneration. Ophthalmol Retin. 2020;4(1):31–40. https://doi.org/10.1016/j.oret.2019.08.003.
Borrelli E, Abdelfattah NS, Uji A, Nittala MG, Boyer DS, Sadda SR. Postreceptor Neuronal Loss in Intermediate Age-related Macular Degeneration. Am J Ophthalmol. 2017;181:1–11. https://doi.org/10.1016/J.AJO.2017.06.005.
Gin TJ, Wu Z, Chew SKH, Guymer RH, Luu CD. Quantitative analysis of the ellipsoid zone intensity in phenotypic variations of intermediate age-related macular degeneration. Investig Ophthalmol Vis Sci. 2017;58(4):2079–86. https://doi.org/10.1167/iovs.16-20105.
Zarubina AV, et al. Prevalence of subretinal drusenoid deposits in older persons with and without age-related macular degeneration, by multimodal imaging. Ophthalmology. 2016;123(5):1090–100. https://doi.org/10.1016/j.ophtha.2015.12.034.
Huisingh C, et al. The association between subretinal drusenoid deposits in older adults in normal macular health and incident age-related macular degeneration. Investig Ophthalmol Vis Sci. 2016;57(2):739–45. https://doi.org/10.1167/iovs.15-18316.
Borrelli, E et al. Impact of bleaching on photoreceptors in different intermediate AMD phenotypes. Transl Vis Sci Technol. 2019; 8(6). https://doi.org/10.1167/tvst.8.6.5LK.
Laíns I, et al. Choroidal changes associated with subretinal drusenoid deposits in age-related macular degeneration using swept-source optical coherence tomography. Am J Ophthalmol. 2017;180:55–63. https://doi.org/10.1016/J.AJO.2017.05.021.
Schlanitz FG, et al. Identification of Drusen characteristics in age-related macular degeneration by polarization-sensitive optical coherence tomography. Am J Ophthalmol. 2015;160(2):335-344.e1. https://doi.org/10.1016/J.AJO.2015.05.008.
Nattagh K, et al. Oct angiography to predict geographic atrophy progression using choriocapillaris flow void as a biomarker. Transl Vis Sci Technol. 2020;9(7):10. https://doi.org/10.1167/tvst.9.7.6.
Lek JJ, et al. Interpretation of subretinal fluid using oct in intermediate age-related macular degeneration. Ophthalmol Retin. 2018;2(8):792–802. https://doi.org/10.1016/J.ORET.2018.01.005.
Nesper PL, Soetikno BT, Fawzi AA. Choriocapillaris nonperfusion is associated with poor visual acuity in eyes with reticular pseudodrusen. Am J Ophthalmol. 2017;174:42–55. https://doi.org/10.1016/j.ajo.2016.10.005.
Venkatesh P, Sagar P, Chawla R, Gogia V, Vohra R, Raj Sharma Y. Evaluation of fundus autofluorescence patterns in age-related macular degeneration. Int J Ophthalmol. 2016. https://doi.org/10.18240/ijo.2016.12.13.
Schmitz-Valckenberg S, et al. Natural history of geographic atrophy progression secondary to age-related macular degeneration (Geographic Atrophy Progression Study). Ophthalmology. 2016;123(2):361–8. https://doi.org/10.1016/j.ophtha.2015.09.036.
Holz FG, et al. Progression of geographic atrophy and impact of fundus autofluorescence patterns in age-related macular degeneration. Am J Ophthalmol. 2007;143(3):463-472.e2. https://doi.org/10.1016/j.ajo.2006.11.041.
Allingham MJ, et al. Semiautomatic segmentation of rim area focal hyperautofluorescence predicts progression of geographic atrophy due to dry age-related macular degeneration. Invest Ophthalmol Vis Sci. 2016;57(4):2283–9. https://doi.org/10.1167/iovs.15-19008.
Marsiglia M, et al. Association between geographic atrophy progression and reticular pseudodrusen in eyes with dry age-related macular degeneration. Investig Ophthalmol Vis Sci. 2013;54(12):7362–9. https://doi.org/10.1167/iovs.12-11073LK.
Bagheri S, et al. Percentage of foveal vs total macular geographic atrophy as a predictor of visual acuity in age-related macular degeneration. J Vitreoretin Dis. 2019;3(5):278–82. https://doi.org/10.1177/2474126419859454.
Wiest MRJ, et al. Globotrioasylsphingosine levels and optical coherence tomography angiography in Fabry disease patients. J Clin Med. 2021;10(5):1093. https://doi.org/10.3390/jcm10051093.
Koman-Wierdak E, et al. Kinetic and static perimetry after 16 years and additional OCT-A analysis in eyes with longlasting optic disc drusen. PLoS ONE. 2021. https://doi.org/10.1371/journal.pone.0247399.
Bonfiglio V, et al. Vascular changes after vitrectomy for rhegmatogenous retinal detachment: optical coherence tomography angiography study. Acta Ophthalmol. 2020;98(5):e563–9. https://doi.org/10.1111/aos.14315.
Sunness JS, Rubin GS, Broman A, Applegate CA, Bressler NM, Hawkins BS. Low luminance visual dysfunction as a predictor of subsequent visual acuity loss from geographic atrophy in age-related macular degeneration. Ophthalmology. 2008. https://doi.org/10.1016/j.ophtha.2008.03.009.
Puell MC, Barrio AR, Palomo-Alvarez C, Gómez-Sanz FJ, Clement-Corral A, Pérez-Carrasco MJ. Impaired mesopic visual acuity in eyes with early age-related macular degeneration. Investig Ophthalmol Vis Sci. 2012;53(11):7310–4. https://doi.org/10.1167/iovs.11-8649.
Cocce KJ, et al. Visual function metrics in early and intermediate dry age-related macular degeneration for use as clinical trial endpoints. Am J Ophthalmol. 2018;189:127–38. https://doi.org/10.1016/J.AJO.2018.02.012.
Wu Z, Guymer RH, Finger RP, Research M. Low luminance deficit and night vision symptoms in intermediate age-related macular degeneration. Br J Ophthalmol. 2016;100(3):395–8. https://doi.org/10.1136/bjophthalmol-2015-306621.
Owsley C, McGwin G, Scilley K, Kallies K. Development of a questionnaire to assess vision problems under low luminance in age-related maculopathy. Investig Ophthalmol Vis Sci. 2006;47(2):528–35. https://doi.org/10.1167/iovs.05-1222.
Thompson AC, et al. Association of low luminance questionnaire with objective functional measures in early and intermediate age-related macular degeneration. Invest Ophthalmol Vis Sci. 2018;59(1):289–97. https://doi.org/10.1167/iovs.17-22528.
Owsley C, Clark ME, Huisingh CE, Curcio CA, McGwin G. Visual function in older eyes in normal macular health: association with incident early age-related macular degeneration 3 years later. Investig Ophthalmol Vis Sci. 2016;57(4):1782–9. https://doi.org/10.1167/iovs.15-18962LK.
Wrzesińska D, et al. Secondary vitrectomy with internal limiting membrane plug due to persistent full-thickness macular hole OCT-Angiography and microperimetry features: case series. J Ophthalmol. 2020. https://doi.org/10.1155/2020/2650873.
Wrzesinska D, et al. Vertical and horizontal M-charts and microperimetry for assessment of the visual function in patients after vitrectomy with ILM peeling due to stage 4 macular hole. J Ophthalmol. 2019. https://doi.org/10.1155/2019/4975973.
Rabin J, Gooch J, Ivan D. Rapid quantification of color vision: the cone contrast test. Investig Ophthalmol Vis Sci. 2011;52(2):816–20. https://doi.org/10.1167/iovs.10-6283.
Hsu ST, et al. Longitudinal study of visual function in dry age-related macular degeneration at 12 months. Ophthalmol Retin. 2019;3(8):637–48. https://doi.org/10.1016/J.ORET.2019.03.010.
Hariri AH, Tepelus TC, Akil H, Nittala MG, Sadda SR. Retinal sensitivity at the junctional zone of eyes with geographic atrophy due to age-related macular degeneration. Am J Ophthalmol. 2016;168:122–8. https://doi.org/10.1016/j.ajo.2016.05.007.
Wu Z, Ayton LN, Luu CD, Guymer RH. Microperimetry of nascent geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2014;56(1):115–21. https://doi.org/10.1167/iovs.14-15614.
Wu Z, et al. Longitudinal associations between microstructural changes and microperimetry in the early stages of age-related macular degeneration. Investig Ophthalmol Vis Sci. 2016;57(8):3714–22. https://doi.org/10.1167/iovs.15-18294.
Vujosevic S, et al. Long-term longitudinal modifications in mesopic microperimetry in early and intermediate age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol. 2017;255(2):301–9. https://doi.org/10.1007/s00417-016-3466-z.
Steinberg JS, Fitzke FW, Fimmers R, Fleckenstein M, Holz FG, Schmitz-Valckenberg S. Scotopic and photopic microperimetry in patients with reticular drusen and age-related macular degeneration. JAMA Ophthalmol. 2015;133(6):690–7. https://doi.org/10.1001/jamaophthalmol.2015.0477.
Nittala MG, et al. AMISH EYE STUDY: baseline spectral domain optical coherence tomography characteristics of age-related macular degeneration. Retina. 2019;39(8):1540–50. https://doi.org/10.1097/IAE.0000000000002210LK.
Jackson GR, Scott IU, Kim IK, Quillen DA, Iannaccone A, Edwards JG. Diagnostic sensitivity and specificity of dark adaptometry for detection of age-related macular degeneration. Investig Ophthalmol Vis Sci. 2014;55(3):1427–31. https://doi.org/10.1167/iovs.13-13745.
Owsley C, et al. Delayed rod-mediated dark adaptation is a functional biomarker for incident early age-related macular degeneration. Ophthalmology. 2016;123(2):344–51. https://doi.org/10.1016/J.OPHTHA.2015.09.041.
Nguyen CT, et al. Longitudinal changes in retinotopic rod function in intermediate age-related macular degeneration. Investig Ophthalmol Vis Sci. 2018;59(4):AMD9–24. https://doi.org/10.1167/iovs.17-23084 (LK).
Jackson GR, Clark ME, Scott IU, Walter LE, Quillen DA, Brigell MG. Twelve-month natural history of dark adaptation in patients with AMD. Optom Vis Sci. 2014;91(8):925–31. https://doi.org/10.1097/OPX.0000000000000247.
Owsley C, Clark ME, McGwin GOCMEMG. Natural history of rod-mediated dark adaptation over 2 years in intermediate age-related macular degeneration. Transl Vis Sci Techno. 2017. https://doi.org/10.1167/tvst.6.3.15 (LK).
Laíns I, et al. Structural changes associated with delayed dark adaptation in age-related macular degeneration. Ophthalmology. 2017;124(9):1340–52. https://doi.org/10.1016/J.OPHTHA.2017.03.061.
Neely D, et al. Association between subretinal drusenoid deposits (SDD) seen by multimodal imaging and dark adaptation (DA) in normal, early, and intermediate agerelated macular degeneration (AMD) eyes. Investig Ophthalmol Vis Sci. 2015;56(7):2777.
Laíns I, et al. Peripheral changes associated with delayed dark adaptation in age-related macular degeneration. Am J Ophthalmol. 2018;190:113–24. https://doi.org/10.1016/J.AJO.2018.03.035.
Tan R, Guymer RH, Luu CD. Subretinal drusenoid deposits and the loss of rod function in intermediate age-related macular degeneration. Investig Ophthalmol Vis Sci. 2018;59(10):4154–61. https://doi.org/10.1167/iovs.18-23970LK.
Sassmannshausen M, et al. Longitudinal analysis of structural and functional changes in presence of reticular pseudodrusen associated with age-related macular degeneration. Investig Ophthalmol Vis Sci. 2020. https://doi.org/10.1167/IOVS.61.10.19.
McGuinness MB, Fraser RG, Tan R, Luu CD, Guymer RH. Relationship between rod-mediated sensitivity, low-luminance visual acuity, and night vision questionnaire in age-related macular degeneration. Transl Vis Sci Technol. 2020;9(6):1–10. https://doi.org/10.1167/TVST.9.6.30.
Gaffney AJ, Binns AM, Margrain TH. The effect of pre-adapting light intensity on dark adaptation in early age-related macular degeneration. Doc Ophthalmol. 2013;127(3):191–9. https://doi.org/10.1007/s10633-013-9400-3.
Grant Robinson D, Margrain TH, Bailey C, Binns AM. An evaluation of a battery of functional and structural tests as predictors of likely risk of progression of age- related macular degeneration. Investig Ophthalmol Vis Sci. 2019;60(2):580–9. https://doi.org/10.1167/iovs.18-25092LK.
Cahill MT, Banks AD, Stinnett SS, Toth CA. Vision-related quality of life in patients with bilateral severe age-related macular degeneration. Ophthalmology. 2005;112(1):152–8. https://doi.org/10.1016/j.ophtha.2004.06.036.
Stein JD, Brown MM, Brown GC, Sharma S, Hollands H. Quality of life with macular degeneration: perceptions of patients, clinicians, and community members. Br J Ophthalmol. 2003;87(1):8–12. https://doi.org/10.1136/bjo.87.1.8.
Brody BL, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108(10):1893–900. https://doi.org/10.1016/S0161-6420(01)00754-0.
Colijn JM, et al. Increased high-density lipoprotein levels associated with age-related macular degeneration. Ophthalmology. 2018;126(3):393–406. https://doi.org/10.1016/j.ophtha.2018.09.045.
Reynolds R, et al. Serum lipid biomarkers and hepatic lipase gene associations with age-related macular degeneration. Ophthalmology. 2010;117(10):1989–95. https://doi.org/10.1016/J.OPHTHA.2010.07.009.
Laíns I, et al. Human plasma metabolomics study across all stages of age-related macular degeneration identifies potential lipid biomarkers. Ophthalmology. 2018;125(2):245–54. https://doi.org/10.1016/J.OPHTHA.2017.08.008.
Krogh Nielsen M, Subhi Y, Rue Molbech C, Nilsson LL, Nissen MH, Sørensen TL. Imbalances in tissue inhibitors of metalloproteinases differentiate choroidal neovascularization from geographic atrophy. Acta Ophthalmol. 2019;97(1):84–90. https://doi.org/10.1111/aos.13894.
Lynch AM, et al. Proteomic profiles in advanced age-related macular degeneration using an aptamer-based proteomic technology. Transl Vis Sci Technol. 2019;8(1):14. https://doi.org/10.1167/tvst.8.1.14.
Lashkari K, et al. Plasma biomarkers of the amyloid pathway are associated with geographic atrophy secondary to age-related macular degeneration. PLoS ONE. 2020;15(8): e0236283. https://doi.org/10.1371/journal.pone.0236283.
Lynch AM, et al. Plasma biomarkers of reticular pseudodrusen and the risk of progression to advanced age-related macular degeneration. Transl Vis Sci Technol. 2020;9(10):1–13. https://doi.org/10.1167/tvst.9.10.12.
Adamus G, Chew EY, Ferris FL, Klein ML. Prevalence of anti-retinal autoantibodies in different stages of Age-related macular degeneration. BMC Ophthalmol. 2014;14(1):154. https://doi.org/10.1186/1471-2415-14-154.
Morohoshi K, et al. Serum autoantibody biomarkers for age-related macular degeneration and possible regulators of neovascularization. Exp Mol Pathol. 2012;92(1):64–73. https://doi.org/10.1016/J.YEXMP.2011.09.017.
Gu J, et al. Assessing susceptibility to age-related macular degeneration with proteomic and genomic biomarkers. Mol Cell Proteomics. 2009;8(6):1338–49. https://doi.org/10.1074/mcp.M800453-MCP200.
Ragusa R, et al. MicroRNAs in vitreus humor from patients with ocular diseases. Mol Vis. 2013;19:430–40.
Toro MD, et al. MicroRNAs in the vitreous humor of patients with retinal detachment and a different grading of proliferative vitreoretinopathy: A pilot study. Transl Vis Sci Technol. 2020;9(6):1–13. https://doi.org/10.1167/tvst.9.6.23.
Russo A, et al. miRNAs in the vitreous humor of patients affected by idiopathic epiretinal membrane and macular hole. PLoS ONE. 2017;12(3): e0174297. https://doi.org/10.1371/journal.pone.0174297.
Ragusa M, et al. miRNA profiling in vitreous humor, vitreal exosomes and serum from uveal melanoma patients: Pathological and diagnostic implications. Cancer Biol Ther. 2015;16(9):1387–96. https://doi.org/10.1080/15384047.2015.1046021.
Szemraj M, et al. Serum MicroRNAs as potential biomarkers of AMD. Med Sci Monit. 2015;21:2734–42. https://doi.org/10.12659/MSM.893697.
Ren C, et al. Circulating miRNAs as potential biomarkers of age-related macular degeneration. Cell Physiol Biochem. 2017;41(4):1413–23. https://doi.org/10.1159/000467941.
Mullins RF, et al. The ARMS2 A69S polymorphism is associated with delayed rod-mediated dark adaptation in eyes at risk for incident age-related macular degeneration. Ophthalmology. 2018. https://doi.org/10.1016/J.OPHTHA.2018.10.037.
Ferrara D, Seddon JM. Phenotypic characterization of complement factor H R1210C rare genetic variant in age-related macular degeneration. JAMA Ophthalmol. 2015;133(7):785–91. https://doi.org/10.1001/jamaophthalmol.2015.0814.
Cao S, et al. Relationship between systemic cytokines and complement factor h y402h polymorphism in patients with dry age-related macular degeneration. Am J Ophthalmol. 2013;156(6):1176–83. https://doi.org/10.1016/J.AJO.2013.08.003.
Seddon JM, Dossett JP, Widjajahakim R, Rosner B. Associations between perifoveal drusen burden and genetic risk in eyes with early or intermediate age-related macular degeneration. Investig Ophthalmol Vis Sci. 2019;60(9). https://doi.org/10.1167/iovs.19-27475.
Nielsen MK, Subhi Y, Molbech CR, Falk MK, Nissen MH, Sørensen TL. Systemic levels of interleukin-6 correlate with progression rate of geographic atrophy secondary to age-related macular degeneration. Investig Ophthalmol Vis Sci. 2019;60(1):202–8. https://doi.org/10.1167/iovs.18-25878.
Seddon JM. Biomarkers for age-related macular degeneration (AMD). US 2005/0250745 A1, 2005.
Lad EM, Cousins SW, Van Arnam JS, Proia AD. Abundance of infiltrating CD163+ cells in the retina of postmortem eyes with dry and neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2015;253(11):1941–5. https://doi.org/10.1007/s00417-015-3094-z.
Cherepanoff S, McMenamin P, Gillies MC, Kettle E, Sarks SH. Bruch’s membrane and choroidal macrophages in early and advanced age-related macular degeneration. Br J Ophthalmol. 2010;94(7):918–25. https://doi.org/10.1136/bjo.2009.165563.
De S, Rabin DM, Salero E, Lederman PL, Temple S, Stern JH. Human retinal pigment epithelium cell changes and expression of αB-Crystallin. Arch Ophthalmol. 2007;125(5):641. https://doi.org/10.1001/archopht.125.5.641.
Mo FM, Proia AD, Johnson WH, Cyr D, Lashkari K. Interferon γ-inducible protein-10 (IP-10) and eotaxin as biomarkers in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2010;51(8):4226–36. https://doi.org/10.1167/iovs.09-3910.
Lashkari K. Methods to identify and treat age-related macular degeneration. WO2010/129351A1, 2018.
Baek J-H, et al. Quantitative proteomic analysis of aqueous humor from patients with Drusen and reticular Pseudodrusen in age-related macular degeneration. BMC Ophthalmol. 2018;18(1):289. https://doi.org/10.1186/s12886-018-0941-9.
Qu SC, Xu D, Li TT, Zhang JF, Liu F. ITRAQ-based proteomics analysis of aqueous humor in patients with dry age-related macular degeneration. Int J Ophthalmol. 2019;12(11):1758–66. https://doi.org/10.18240/ijo.2019.11.15.
Schori C, Trachsel C, Grossmann J, Zygoula I, Barthelmes D, Grimm C. The proteomic landscape in the vitreous of patients with age-related and diabetic retinal disease. Invest Ophthalmol Vis Sci. 2018;59(4):AMD31–40. https://doi.org/10.1167/iovs.18-24122.
Winiarczyk M, Kaarniranta K, Winiarczyk S, Adaszek Ł, Winiarczyk D, Mackiewicz J. Tear film proteome in age-related macular degeneration. Graefe’s Arch Clin Exp Ophthalmol. 2018;256(6):1127–39. https://doi.org/10.1007/s00417-018-3984-y.
Guymer RH, et al. Identification of urinary biomarkers for age-related macular degeneration. Investig Ophthalmol Vis Sci. 2011;52(7):4639–44. https://doi.org/10.1167/iovs.10-7120.
Bogunovic H, et al. Machine learning of the progression of intermediate age-related macular degeneration based on OCT imaging. Invest Ophthalmol Vis Sci. 2017;58(6):BIO141–50. https://doi.org/10.1167/iovs.17-21789.
Grassmann F, et al. Clinical and genetic factors associated with progression of geographic atrophy lesions in age-related macular degeneration. PLoS ONE. 2015;10(5):e0126636. https://doi.org/10.1371/journal.pone.0126636.
Schmidt-Erfurth U, et al. Prediction of individual disease conversion in early AMD using artificial intelligence. Investig Opthalmology Vis Sci. 2018;59(8):3199. https://doi.org/10.1167/iovs.18-24106.
Perlee LT, et al. Inclusion of genotype with fundus phenotype improves accuracy of predicting choroidal neovascularization and geographic atrophy. Ophthalmology. 2013;120(9):1880–92. https://doi.org/10.1016/j.ophtha.2013.02.007.
Pfau M, et al. Progression of photoreceptor degeneration in geographic atrophy secondary to age-related macular degeneration. JAMA Ophthalmol. 2020;138(10):1026–34. https://doi.org/10.1001/jamaophthalmol.2020.2914.
Schmidt-Erfurth U, et al. Role of deep learning-quantified hyperreflective foci for the prediction of geographic atrophy progression. Am J Ophthalmol. 2020;216:257–70. https://doi.org/10.1016/j.ajo.2020.03.042.
Saha S, et al. Automated detection and classification of early AMD biomarkers using deep learning. Sci Rep. 2019. https://doi.org/10.1038/s41598-019-47390-3.
Finger RP, et al. MACUSTAR: Development and clinical validation of functional, structural, and patient-reported endpoints in intermediate age-related macular degeneration. Ophthalmologica. 2019;241(2):61–72. https://doi.org/10.1159/000491402.
The Age-Related Eye Disease Study Research Group. The age-related eye disease study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: The age-related eye disease study report number 6. Am J Ophthalmol. 2001;132(5):668–81. https://doi.org/10.1016/S0002-9394(01)01218-1.
Wu Z, Ayton LN, Luu CD, Baird PN, Guymer RH. Reticular pseudodrusen in intermediate age-related macular degeneration: Prevalence, detection, clinical, environmental, and genetic associations. Investig Ophthalmol Vis Sci. 2016;57(3):1310–6. https://doi.org/10.1167/iovs.15-18682.
Wu Z, et al. Fundus autofluorescence characteristics of nascent geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2015;56(3):1546–52. https://doi.org/10.1167/iovs.14-16211.
Mauschitz MM, et al. Topography of geographic atrophy in age-related macular degeneration. Investig Ophthalmol Vis Sci. 2012;53(8):4932–9. https://doi.org/10.1167/iovs.12-9711.
Fleckenstein M, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125(3):369–90. https://doi.org/10.1016/j.ophtha.2017.08.038.
Jackson GR, Owsley C. Method and apparatus for the detection of impaired dark adaptation. US 9572485 B2, 2017.
Owsley C, Huisingh C, Clark ME, Jackson GR, McGwin G. Comparison of visual function in older eyes in the earliest stages of age-related macular degeneration to those in normal macular health. Curr Eye Res. 2016;41(2):266–72. https://doi.org/10.3109/02713683.2015.1011282.
Wu Z, Ayton LN, Luu CD, Guymer RH. Relationship between retinal microstructures on optical coherence tomography and microperimetry in age-related macular degeneration. Ophthalmology. 2014;121(7):1445–52. https://doi.org/10.1016/J.OPHTHA.2014.01.025.
Kim JB, Lad EM. Therapeutic options under development for nonneovascular age-related macular degeneration and geographic atrophy. Drugs Aging. 2021;38(1):17–27. https://doi.org/10.1007/s40266-020-00822-6 (Adis).
Alkeus Pharmaceuticals I. A Phase 2/3 multicenter, randomized, double-masked, parallel-group, placebo-controlled study to investigate the safety, pharmacokinetics, tolerability, and efficacy of ALK-001 in geographic atrophy secondary to age. clinicaltrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03845582. Accessed 28 May 28 2021.
Rosenfeld PJ, et al. Emixustat hydrochloride for geographic atrophy secondary to age-related macular degeneration: a randomized clinical trial. Ophthalmology. 2018;125(10):1556–67. https://doi.org/10.1016/j.ophtha.2018.03.059.
Mettu P, Cousins S. The ReCLAIM phase 1 clinical trial of elamipretide for dry AMD. Retinal Phys. 2019. https://www.retinalphysician.com/issues/2019/november-2019/the-reclaim-phase-1-clinical-trial-of-elamipretide. Accessed 28 May 28 2021.
Ophthalmics LA. Bausch health to acquire option to purchase all ophthalmology assets of allegro ophthalmics. Allegro Ophthalmics, LLC. 2020. https://www.allegroeye.com/bausch-health-to-acquire-option-to-purchase-all-ophthalmology-assets-of-allegro-ophthalmics/. Accessed 28 May 28 2021.
BioSpace. Gemini therapeutics enrolls first patient in phase 2a study of GEM103 for Dry age-related macular degeneration. BioSpace. 2020. https://www.biospace.com/article/gemini-therapeutics-enrolls-first-patient-in-phase-2a-study-of-gem103-for-dry-age-related-macular-degeneration/. Accessed 28 May 28 2021.
“Zimura phase 2b trial results positive in geographic atrophy secondary to dry AMD,” Healio Ophthalmol. 2019. https://www.healio.com/news/ophthalmology/20191028/zimura-phase-2b-trial-results-positive-in-geographic-atrophy-secondary-to-dry-amd. Accessed 28 May 28 2021.
Liao DS, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology. 2020;127(2):186–95. https://doi.org/10.1016/j.ophtha.2019.07.011.
Markowitz SN, et al. A double-masked, randomized, sham-controlled, single-center study with photobiomodulation for the treatment of dry age-related macular degeneration. Retina. 2020;40(8):1471–82. https://doi.org/10.1097/IAE.0000000000002632.
Joachim N, Mitchell P, Burlutsky G, Kifley A, Wang JJ. The incidence and progression of age-related macular degeneration over 15 years: the Blue Mountains Eye Study. Ophthalmology. 2015;122(12):2482–9. https://doi.org/10.1016/j.ophtha.2015.08.002.
Stark A. FDA permits marketing of artificial intelligence-based device to detect certain diabetes-related eye problems. Case Med Res. 2018. https://doi.org/10.31525/fda2-ucm604357.htm.
Acknowledgments
Financial support—EML: Apellis, LumiThera, Novartis, Roche (through Duke University).
Author information
Authors and Affiliations
Ethics declarations
Funding
EML: Apellis, LumiThera, Novartis, and Roche (through Duke University).
Conflict of interest
VF: none; MGC: none; EML: Consultant—Apellis, Galimedix, Genentech/Roche, Novartis, Retrotope, Gemini Therapeutics, Allegro, and Alexion.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Rights and permissions
About this article
Cite this article
Fang, V., Gomez-Caraballo, M. & Lad, E.M. Biomarkers for Nonexudative Age-Related Macular Degeneration and Relevance for Clinical Trials: A Systematic Review. Mol Diagn Ther 25, 691–713 (2021). https://doi.org/10.1007/s40291-021-00551-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-021-00551-5