Abstract
Background
Understanding the determinants of children’s health behaviours is important to develop successful behaviour-change interventions.
Objective
We aimed to synthesise the evidence around determinants (‘preceding predictors’) of change in physical activity (PA) in young children (0–6 years of age).
Methods
As part of a suite of reviews, prospective quantitative studies investigating change in physical activity in children aged 0–6 years were identified from eight databases (to October 2015): MEDLINE, Embase, CINAHL, PsycINFO, Web of Knowledge, British Nursing Index, Applied Social Sciences Index and Abstracts, and Sociological Abstracts. Determinants and direction of association were extracted, described and synthesised according to the socio-ecological model (individual, interpersonal, organisational, community, policy).
Results
Forty-four determinants, predominantly in the interpersonal and organisational domains, were reported across 44 papers (six prospective cohort, 38 interventional); 14 determinants were assessed in four or more papers. Parental monitoring showed a consistent positive association with change in PA; provider training was positively associated with change in children’s moderate-to-vigorous PA only. Five (sex, parental goal setting, social support, motor skill training and increased time for PA) showed no clear association. A further seven (child knowledge, parental knowledge, parental motivation, parenting skills, parental self-efficacy, curriculum materials and portable equipment) were consistently not associated with change in children’s PA. Maternal role-modelling was positively associated with change in PA in all three studies in which it was examined.
Conclusions
A range of studied determinants of change in young children’s PA were identified, but only parental monitoring was found to be consistently positively associated. More evidence dealing with community and policy domains from low-/middle-income countries and about lesser-explored modifiable family- and childcare-related determinants is required.
International Prospective Register for Systematic Reviews (PROSPERO) Registration Number
CRD42012002881.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Forty-four determinants of change in young children’s physical activity were assessed across 44 papers, predominately in the intrapersonal, interpersonal and organisational domain. |
Although 14 determinants were assessed in four or more studies, only parental monitoring was consistently positively associated with change in physical activity and provider training associated with change in moderate-to-vigorous physical activity. |
Evidence in community and policy domains, and from low-/middle-income countries, is required. |
1 Background
By the age of 5 years, over one in five children are overweight or obese the UK and USA [1, 2]. Obesity in childhood is associated with a range of unfavourable outcomes including type 2 diabetes, hyperlipidaemia and psychosocial problems [3], with obesity known to track and be associated with unfavourable outcomes in adulthood [4, 5]. Early childhood is a period of rapid growth and development, and the preschool years (defined here as up to the age of 6 years) are therefore ideal to both prevent and reverse unhealthy weight gain, by establishing healthy habits and behaviours.
As a result, interventions aiming to effect positive dietary, physical activity and sedentary behaviour change have been developed to prevent or halt obesity in the preschool years [6–9]. However, with a few notable exceptions [10–12], many of these interventional studies showed small effects which are not sustained over time, or have no effect at all [6–9]. One difficulty in establishing the reasons for a lack of intervention success is that multiple behaviours are often targeted simultaneously [8, 9]. However, as each health behaviour has an independent significant impact on children’s health [13, 14], it is important to establish the most important determinants of each individual behaviour, and therefore how they may differ across behaviours. The socio-ecological model (SEM) [15] is a commonly used framework for categorising levels of influence on behaviours [16, 17], classifying them into five broad categories: individual; interpersonal, organizational, community and public policy. By grouping potential influences on behaviour in this way, commonalities and differences can be identified and subsequently used to develop more targeted interventions to effectively change children’s health behaviours [18].
In addition to consuming a balanced nutritious diet, children up to the age of 5 years are recommended to engage in 180 min of physical activity daily [19, 20]. Higher levels of physical activity are associated not only with decreased adiposity in preschool-aged children but also positively associated with motor skill development, psychosocial health and decreased cardio-metabolic risk prospectively [13]. Cross-sectional studies in older preschool-aged children (2 years and over) also indicate that increased physical activity is linked to better gross motor control [21] and improved social skills [22]. Yet despite the importance of physical activity for young children’s health and development [13], studies suggest that young children do not engage in sufficient levels of physical activity [23].
In order to specifically increase physical activity in targeted interventions, it is important to establish which factors influence activity behaviour [24]. A number of systematic reviews have been conducted to examine the associations between cross-sectional factors (‘correlates’) and young children’s physical activity [16, 25, 26]. A broad range of correlates have been investigated, including demographic, biological, environmental, social and psychological influences. Although conclusions about the influences on physical activity differ between reviews [25, 27], there is a suggestion that familial influences [16, 25, 26], time spent outside [25] and elements in the physical environment [25, 27] may be associated with increased activity in preschoolers. An additional review [28] that included cross-sectional studies and a small number prospective cohorts also suggests that home influences may be key for young children’s physical activity. However, it is difficult to draw firm conclusions about causality from cross-sectional studies. It is therefore necessary to use evidence from both prospective and interventional studies as these provide the best evidence to establish the longitudinal predictors (or ‘determinants’) of change in young children’s physical activity, and to aid understanding of how to effect positive behaviour change.
This systematic review is part of a suite of reviews exploring the determinants of obesogenic behaviours in children aged 0–6 years (focussed on fruit and vegetable intake, sugar-sweetened beverages and unhealthy diet intake, physical activity and sedentary behaviour) [29, 30]. It aims to synthesise the quantitative literature from prospective and interventional studies to ascertain the determinants (a ‘preceding predictor’) of change in physical activity in young children. It also aims to establish which (modifiable) determinants are associated with change; at which levels of influence these factors operate (i.e. individual, family, childcare setting, community or policy level); and where gaps in the literature exist for future research.
2 Methods
The protocol for this review project has been described previously [29]. The International Prospective Register for Systematic Reviews (PROSPERO) Registration number is CRD42012002881. Following established criteria for the rigorous conduct and reporting of systematic reviews [31, 32], this review was carried out in three stages [33, 34]. One search (led by HM) was conducted to identify studies across all reviews; at the data-extraction stage, smaller teams led each of the reviews focusing on specific behaviours of interest [i.e. physical activity (review lead: KH), fruit and vegetable consumption (COM), and sugar-sweetened beverages (VP)]. KH also conducted the search update specific to physical activity in October 2015.
2.1 Generic Review Methods
2.1.1 Identification of Studies for Review
A systematic search, common to all reviews, was undertaken in August 2012. Four sets of search terms were used related to: the population; study design (capturing observational, interventional and review articles); outcome; and exclusion of clinical populations. An extensive scoping phase was conducted prior to implementing the full search to maximize sensitivity and specificity of included papers. This involved contacting experts in the field and identifying key publications to be included for each behaviour, with searches run to ensure that these publications were captured. An electronic search was conducted in eight databases [MEDLINE, Embase (via OVID), CINAHL, PsycINFO (via EBSCO), Web of Knowledge (via Thomson Reuters), British Nursing Index (BNI), Applied Social Sciences Index and Abstracts (ASSIA) and Sociological Abstracts (via ProQuest)]. Citations were downloaded into Endnote citation management software (Thomson Reuters, Philadelphia, PA, USA). Included papers were searched for additional relevant publications, as were relevant reviews. No language restrictions were placed on the search, but articles were limited to published full texts. An updated search was conducted in October 2015 to capture studies with outcomes relating to physical activity only, published in the interim period (Electronic Supplementary Material Table S1).
2.1.2 Study Selection
In 2012, two batches of 500 titles and abstracts were screened for inclusion by the review leads (KH, VP, COM) and checked for fidelity by a fourth reviewer (CS). With less than a 5% discrepancy, each reviewer subsequently screened approximately 12,000 papers individually. For quality control, two random 5% samples (total n = 3600) were double screened by two additional reviewers (RL and EvS). All full texts were obtained and distributed for the behaviour-specific reviews to progress in parallel. Additional texts retrieved in 2015 were screened by KH and a subsample (15%) reviewed by EvS.
2.2 Methods for Physical Activity Review
2.2.1 Inclusion/Exclusion Criteria
Articles were included if (a) they reported results from a longitudinal observational study, randomized controlled trial (RCT) or controlled trial (CT), (b) quantified a within-child change in physical activity behaviour (as primary/second outcome in interventions) and (c) assessed at least one potential determinant of change. Children had to be aged between 0 and 6 years at baseline, and studies assessing physical activity using objective or subjective measures were included. Exclusion criteria included: (a) clinical populations (e.g. children who were malnourished, had asthma, cerebral palsy, cystic fibrosis, autism, etc.), (b) non-human studies, (c) quantitative cross-sectional studies, (d) qualitative studies, and (e) laboratory-based studies (e.g. validation studies).
2.2.2 Quality Assessment
For descriptive purposes, a quality appraisal of each of the included studies was conducted focusing on internal and external validity using assessment criteria adapted from those used previously [34, 35] (Electronic Supplementary Material Table S2). Criteria included: sample representativeness, size and retention, use of objective exposure and outcomes measures, appropriateness of analysis strategy, and randomisation method for RCTs. Scores out of 6 (or 7 for RCTs) were allocated and categorised accordingly (high quality: ≥5; medium: 3–4; low: 1–2).
2.2.3 Data Extraction
All full texts identified for inclusion were read by KH, and double screened for inclusion by EvS. For relevant papers, data were extracted using a standardized form. Data extracted included fırst author; publication year; country; study design, setting and population; and baseline descriptive characteristics. Data were also extracted about physical activity measurement and outcome; potential determinants; method of analysis; duration of follow-up; loss to follow-up; and results. All outcome measures used in prospective and interventional studies [e.g. percentage time or minutes spent at differing activity intensities (i.e. light (LPA), moderate (MPA), vigorous (VPA), moderate to vigorous (MVPA) or total activity (LMVPA)] were extracted. However, in some studies, activity was only assessed during specific periods (i.e. at weekends, during recess). In an attempt to standardise findings across studies, where more than one physical activity outcome was reported, we report total physical activity/counts per epoch (given current guidelines for young children’s activity [19, 20]), followed by MVPA, LPA and MPA/VPA. For interventional studies, each of the described elements targeted in the intervention (e.g. parental knowledge, parental modelling) were extracted as potential determinants of change in physical activity. For each determinant, the smallest included sub-sample was considered for extraction (e.g. if stratified by sex). Where results were stratified by specific times of the day, results for the largest time periods were reviewed and extracted. For longitudinal studies, the latest data available before the children were 6 years old were included; where two or more papers reported on the same study sample, both were included if they reported determinants associated with different outcome measures. For interventional studies, we assessed the difference in physical activity between control and intervention groups over time to classify determinants, as this provided evidence of factors targeted in interventions (i.e. determinants) which were associated with change. Where possible, results of multivariable rather than univariable models were included.
2.3 Data Synthesis
Narrative data synthesis was undertaken for all studies. Due to the heterogeneous nature of included quantitative studies and the physical activity outcomes used, meta-analysis was not appropriate. Each extracted determinant was scored based on direction and strength of evidence: ‘−’ significant decrease in physical activity; ‘0’ no significant association/effect or ‘+’ significant increase in physical activity. Evidence from cohort and interventional studies was weighted equally, as both provide prospective determinants of change in physical activity behaviour. As per previous reviews [16, 17, 36], consistency across studies for any given determinant was then summarized according to the following metric: ‘0’ (no association) if supported by 0–33% of individual studies; ‘?’ (indeterminate/possible) if supported by 34–59%; and ‘+’ or ‘−’ if supported by 60–100%. Where four or more studies reported on a potential determinant, double indicators were used (e.g. ‘00’, ‘??’, ‘++’ and ‘−−’) to indicate greater levels of evidence and therefore confidence in findings. Determinants, study score and consistency across studies were then presented according to the SEM (individual, interpersonal, organisational, community and policy) [17, 36].
3 Results
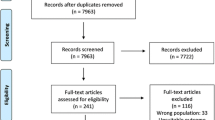
A total of 37,686 (full review) and 3652 (physical activity-specific update) references were retrieved in 2012 and 2015 respectively, of which 220 were read in full and 44 papers included for review (representing 42 study samples: four prospective cohort and 38 interventional studies, see Fig. 1). A descriptive summary of the included study samples is presented in Table 1; study-specific information is provided in Tables 2 and 3.
Flowchart outlining identification of papers for inclusion. ASSIA Applied Social Science Index and Abstracts, BNI British Nursing Index. 1Full search conducted including terms for all health behaviours (i.e. diet, physical activity), physical activity search update included terms for physical activity behaviours only
3.1 Summary of Study Characteristics
Study samples originated in the USA (n = 24), Australasia (n = 6) and Europe (n = 12); no papers were identified from developing nations, and all bar one was published after 2003. Of included studies, 15 (34%; 13 interventional, two prospective) had a final sample size greater than 250 children, and most included similar numbers of boys and girls. Objective measures of physical activity were used in 34 (77%) papers (accelerometer: 27; pedometer: four; heart-rate/Actiheart: three), although those papers using proxy-report measures were also included (n = 10; one prospective, nine interventional). Interventions often targeted a number of behaviours, including diet and sedentary behaviour, but 18 (38%) specifically aimed to increase physical activity [37–54]. The measurement period (from baseline to last contact) was a median of 2.5 years (range 1–5 years) for prospective papers and 34.5 weeks (range: 1 day to 5 years post-intervention) for interventional papers. One prospective paper and 26 interventional papers (61%) were deemed to be of high quality (score ≥5), nine were of medium quality (score 3–4) and six were low quality (score of 2). Of the interventional studies, 28 (64%) randomised participants. Most study samples drew participants from White populations; some targeted lower socioeconomic or racial minority groups [11, 55–58]. A retention rate of ≥70% was reported in 20 papers (46%), and 27 interventional studies reported final analysis samples by study group, indicating similar levels of attrition.
3.2 Overview of Prospective and Intervention Studies
A total of 44 potential determinants of change were reported (Table 4) across papers. The same cohort study [Children Living in Active Neighborhoods (CLAN) [59]] was described in three [60–62] of the six prospective papers. One paper describing this study contributed all 16 determinants identified across prospective studies in intrapersonal, interpersonal and temporal domains. This paper predominantly reported on determinants relating to parental influence on change in physical activity.
The 38 interventional studies targeted 28 potential (modifiable) determinants at intrapersonal (n = 6), interpersonal (n = 10), organisational (n = 10) and community levels (n = 1). No determinants at the policy level were identified across included studies. Of the 38 interventional studies, 27 (68%) were classified as multi-level [11, 42, 44, 46–48, 50–52, 54–56, 58, 63–76]; these most commonly targeted individual/interpersonal (i.e. children, parents, teachers) and organisational (i.e. preschool/ home environment) factors. Of these, 11 multi-level interventions (42%) effected a positive change in children’s physical activity [42, 44, 46, 47, 54, 58, 63, 65, 66, 69, 72], though no clear effective combinations of components emerged. Across all prospective studies, positive effect sizes were generally small, with increases of less than 10% in total activity or MVPA from relatively low baseline levels.
3.3 Determinants Identified in Four or More Studies
Fourteen determinants were assessed in four or more studies. One, sex, was reported in five prospective papers [60, 61, 77–79] (from four study samples: the associations between sex and two different outcome measures were assessed within the same CLAN study sample). The remaining 13 determinants, reported four or more times, were all interventional components, including at the intrapersonal level: motor/skills training [46, 47, 50–52, 54, 65, 66, 75, 80] and child knowledge [11, 42, 50, 55, 56, 64, 71, 73, 75, 76, 81], and at the interpersonal level: parental monitoring [42, 44, 66, 69, 70, 72]; parental motivation [49, 57, 72, 82]; goal setting [69, 72, 76, 83]; parental knowledge [11, 42, 44, 48–50, 55, 56, 58, 64, 66, 69–73, 75, 76, 80–83]; general parental skills [49, 51, 76, 81–84]; parent self-efficacy [57, 66, 70, 82]; parental social support [69, 72, 75, 83, 84]; and provider training [38, 44–47, 49–54, 64, 66, 72, 75, 80]. Those determinants at the organisational level included: more physical activity opportunities [11, 38, 40, 45, 53, 55, 56, 65, 66, 73, 75]; use of portable equipment [37, 41, 48, 50, 75]; and supplying curriculum materials [11, 49, 50, 53, 55, 56, 64, 71, 73, 75, 80].
Of these 14 more frequently studied determinants, parental monitoring was consistently shown to be positively associated with change in young children’s physical activity across intensities, with four of six study samples reporting a positive association. Provider training was also positively associated with change in children’s MVPA in six of nine studies [38, 44, 46, 47, 53, 54], but showed no clear association with physical activity overall (positive association in 8/16 studies), suggesting that determinants may be intensity specific.
Five determinants, across the intra- and interpersonal domains, namely sex (positive association in 2/5 studies); motor skill training (5/10); parental goal setting (2/4); parental social support (2/5); and increased time for physical activity (usually within the care setting; 4/11) showed no consistent association with change in physical activity. In the case of sex, evidence from the CLAN study served to highlight how determinants may differ within the same sample depending on the outcome used and time of follow-up [i.e. no association with counts per epoch at first follow-up [60] but a positive association between (male) sex and MVPA at second follow-up [61]]. For motor skills training [46, 47, 54, 65, 66] and increased time for physical activity [38, 53, 65, 66] the majority of interventional studies that found a positive association with change in physical activity used objective measures.
The remaining seven determinants assessed in four or more studies, i.e. child knowledge (positive association in 2/12 studies), parental knowledge (7/22), parenting skills (2/7), parental motivation (1/4), parental self-efficacy (1/4), curriculum materials (2/11), and portable equipment (1/5), consistently showed no association with change in young children’s physical activity (i.e. >67% of studies reported no association).
3.4 Determinants Identified in Fewer than Four Studies
Determinants assessed in three study samples in the intra-/interpersonal domains included child monitoring [42, 70, 82], parental role-modelling [70, 76, 82] and maternal role modelling [44, 58, 61], with only the latter shown to be positively associated with change in physical activity in all three studies (one using proxy-reported physical activity [58]). In the organisational domain, increasing the number of care providers within the childcare setting was found to be positively associated with change in two (out of three) interventional studies [49, 65]. Community awareness showed no association with change in children’s physical activity [71, 72, 81]. Positive associations with change in physical activity were also found for providing additional opportunities for play within the home (two studies) [44, 58] and sibling co-participation (one study) [61], and with structured physical activity [53] and lowering playground density [43] in one study each within the organisational domain.
4 Discussion
4.1 Main Findings
This review is the first to synthesise evidence from longitudinal studies relating to the determinants of change in physical activity in preschool-aged children. Forty-four determinants were identified; determinants at the interpersonal and organisational levels were most commonly evaluated. Fourteen determinants were identified in four or more quantitative studies: parental monitoring showed a consistently positive association with change in physical activity. Provider training was positively associated with change in MVPA, but showed no clear association with physical activity overall. Of the remaining 12 determinants, a further five showed no clear association, and seven were consistently not associated with change in children’s physical activity. Moreover, maternal role modelling was positively associated with physical activity in three studies [44, 58, 61]. A range of modifiable family- and childcare-related elements also showed positive associations with change in young children’s activity in fewer studies. Where positive effects on change in physical activity were seen, they were often small in magnitude, particularly in studies reporting accelerometer-measured outcomes. Despite identifying a range of determinants that have been assessed, there appears to be little evidence of what elements effect positive change in preschoolers’ physical activity. Where determinants have shown no positive effect (e.g. child/parental knowledge), researchers should divert emphasis instead to other potentially influential determinants. Both parental monitoring and maternal role modelling may provide feasible and effective determinants of change; given the lack of longitudinal evidence from the community and policy domains, and with no evidence to date from developing countries, further exploration of possible determinants of change in these areas is also required.
4.2 Findings in the Context of Previous Research
As is also shown in cross-sectional studies [16, 25], the association between the child’s sex and change in physical activity [60, 61, 77–79] was not consistent here. In general, boys’ absolute levels of physical activity were reported to be higher than those of girls [61, 79], suggesting that, regardless of change, boys may remain more active than girls over time. The aim of this review was not to assess whether a determinant was associated with increased physical activity over time, but rather if different levels of a determinant predict differences in change in physical activity over time. Sex is a good example of this: boys’ physical activity may increase over time whilst girls’ activity remains stable, or boys’ activity may remain stable whilst girls’ activity decreases. Although the data available do not allow us to explore the actual direction of change, this is an important consideration for future research. Based on current evidence and quality of measurement, boys appear to be more active than girls, but firm conclusions about the influence of sex on changes in young children’s activity over time cannot be drawn.
Determinants in the interpersonal domain were most frequently assessed. Only one determinant, parental monitoring, was consistently positively associated with change in physical activity in both prospective and interventional studies in this age group. This was operationalized in a range of ways by increasing parental awareness of the child’s physical activity [66, 69], including using log books [44] and pedometers [42]. Although evidence of parental monitoring effecting a positive change in physical activity prospectively in older children is sparse [85, 86], cross-sectional evidence from a small sample of US children (n = 99) suggests that where parenting is permissive, parental monitoring may lead to increases in MVPA in children [87]. Evidence tends to suggest that parents tend to over-estimate their children’s physical activity in general [88]. Yet conscious parental monitoring of the target behaviour may increase its salience, resulting in a greater number of prompts to be active and therefore greater subsequent physical activity.
Three further studies reported a positive effect of maternal role modelling on children’s activity [44, 58, 61]; this ranged from assessing mothers’ own physical activity [61] to increasing maternal awareness and encouraging increased physical activity within families, with or without her child so as to model activity behaviour [44, 58]. These findings are supported by qualitative literature, with parents consistently suggesting that active parents and parents as role models were important facilitators of children’s activity [89–94]. Positive associations between parents’ and children’s activity have also been reported previously in cross-sectional studies [95–97]. Interventional studies targeting other interpersonal factors such as increasing parental knowledge [11, 42, 44, 48–50, 55, 56, 58, 64, 66, 69–73, 75, 76, 80–83] or social support [69, 72, 75, 83, 84], and improving parenting skills [49, 51, 76, 81] showed indeterminate associations; both high and lower quality studies reported both positive [42, 44, 49, 58, 66, 69, 83] and no associations [11, 48, 50, 51, 55, 56, 64, 70–73, 75, 76, 80–82, 84] for these interventional components. It may therefore be that it is parental awareness and their own activity behaviours that are important for their child’s activity. Further research is needed to explore how objectively measured physical activity in preschool-aged children and their parents are associated longitudinally.
Several reviews conducted previously suggest that elements in the preschool environment may be positively associated with children’s activity [27, 98]. Many interventional studies here specifically targeted the childcare environment, providing curriculum materials or modified elements within childcare settings, but no clear determinants were identified [11, 37, 39, 41, 43, 48–50, 53, 55, 56, 64, 71, 73, 75, 80]. Four of the interventional studies used variations of the same ‘Hip-Hop-to-Health’ intervention [11, 55, 56, 73], targeting a range of elements in the childcare setting: only one [56] showed a positive sustained effect on accelerometer-measured activity in a predominantly African American population. This highlights that even with a consistent core intervention, factors including cultural variability, differing reported outcomes and intervention fidelity likely influence intervention success.
Although environmental childcare determinants showed inconclusive results, of 16 interventional studies incorporating provider training, eight noted positive increases in children’s activity [38, 44, 46, 47, 49, 53, 54, 66] and MVPA in particular. Interestingly, those interventions showing positive effects often incorporated few additional environmental elements, including providing additional curriculum materials [49, 53]; they did however tend to include motor skill training [46, 47, 54, 66], or parental elements [44, 66], and/or allocate additional time for physical activity [38, 53, 66]. Introducing additional providers also led to increased physical activity in two out of three high-quality interventional studies, where external gym trainers [49] and professional coaches [65] led physical activity sessions.
Given the increasing amount of time children now spend in childcare, care providers feasibly play an important role in shaping children’s health behaviours. It is not possible here to disentangle which elements of training resulted in positive physical activity change, but encouraging care providers to build on their skill-base and/or confidence in multi-component interventions may be important. Moreover, qualitative literature suggests that care providers perceive themselves to be both a positive [99–101] and a negative [99, 102, 103] influence on children’s physical activity, yet no quantitative studies to date have specifically focused on care-providers own behaviour as a potential determinant. Doing so may be timely given providers believe they can influence children’s activity and that young children should be active, but many are not aware of how much physical activity young children require [104].
Despite an obvious lack of observational research informing intervention development, the majority of interventional studies (68%) were classified as multi-level [11, 42, 44, 46–48, 50–52, 54–56, 58, 63–76], targeting determinants across a range of domains. Though these studies used notionally similar exposures, e.g. targeting children, their parents and changing the preschool environment, inconsistent results were seen. As with all multi-faceted interventions, it is therefore difficult to tease out which components were effective and may explain in part why so few determinants were consistently associated with change in physical activity. Determinants across interpersonal and organisational levels may act synergistically or may counteract each other leading to null results. Although we attempted to determine how each interventional component influenced activity, no formal mediation analyses were identified and further exploration of how elements within an interventional result in positive change would be beneficial. For example, mixed-methods process evaluations may help to delineate determinants of children’s physical activity and aid future intervention development.
4.3 Future Research Directions
This review highlights where research evidence and gaps exist. A large number of (interventional) studies have targeted determinants such as child motor/skills training; child and parental knowledge; provision of extra time for physical activity or curriculum materials; and provider training, with the studies overall showing no or indeterminate effects. Comparatively few studies have assessed a wide range of other determinants such as child/parent goal setting, and provider monitoring or social support. There is also a lack of studies assessing paternal determinants, and where this information is provided, studies tend to use maternal report. Only one determinant has been assessed in the community domain and none in the policy domain; no studies have been conducted to assess determinants in developing countries. Focusing research where such gaps exist will yield novel evidence, potentially prevent wastage of resources and promote physical activity change.
Moreover, little work has been conducted to explore how children’s activity levels change from infancy to the preschool period, with only six studies including children aged 2 years or younger [57, 58, 69, 70, 83, 84]. Questions remain about the optimal method for assessing physical activity in infants and toddlers [105]. Moreover, assessing physical activity across developmental periods may necessitate different measurement and processing protocols, complicating the assessment of change in physical activity. Nevertheless, given that the early years represent a period of rapid development and a crucial window for positive habit formation, it is important to determine for whom, how and why physical activity may change throughout early childhood, and whether behaviour and potential inequalities in health manifest and remain in later years.
Finally, determinants may be time or situation specific. Very few prospective observational studies have assessed determinants of physical activity change in young children. Including both prospective and interventional studies (and treating interventional components as determinants in the latter) allowed us to identify a wider range of factors that have been posited to effect change in physical activity. This review also indicates that determinants may differ within the same cohort depending on measurement method and follow-up period [i.e. in the CLAN study, there was no association between sex and counts per epoch at first follow-up [60] but a positive association between (male) sex and MVPA at second follow-up [61]]. Prospective studies allow assessment of change in behaviour over relatively long periods of time; interventions, with generally much shorter follow-up periods than prospective studies, may be able to capture more short-term fluctuations in behaviour. Both types of study also tend to assess differing types of determinants. Prospective studies have focused on child’s sex and parental psychosocial and temporal factors, whereas interventional studies target child skill and knowledge, parental knowledge and behaviour, and elements in the preschool environment including care-provider training and provision of curriculum materials. Both types of study are therefore beneficial to establish whether a determinant is associated with behaviour change, and whether change is sustained over time. In combination, a more comprehensive picture of the determinants’ landscape in children 0–6 years of age can emerge; this will ensure future research focuses on where gaps in the current evidence exist, whilst focusing work on areas where potential positive gains in changing young children’s physical activity are most likely to be made.
4.4 Strengths and Limitations
This is the first systematic review, to our knowledge, to specifically explore determinants of change of physical activity in children aged 6 years and under across prospective cohort and interventional studies. Given that cohort and interventional studies offered the most appropriate design to extract determinants of change, our research strategy was restricted to prospective studies. We applied rigorous review methods and did not exclude papers based on language, but it is possible that all relevant publications may not have been included, as illustrated by the identification of an additional study at the data-extraction phase. As this review was restricted to published studies, publication bias cannot be discounted. One determinant (sex) was assessed in the same study twice and contributed by more than one paper [60, 61]; however, in general, our methods reduced potential bias by lending more weight to determinants assessed in four or more studies. The inclusion of a range of study types and measures of activity is both a strength and a limitation of this review; studies using pedometers and questionnaires tended to report positive interventional effects. Studies also used differing accelerometer cut points and adjusted for differing covariates in regression models. This heterogeneity highlights how differing study methods may influence findings and intervention success. All studies were conducted in high-income countries and approximately half of the studies had small final sample sizes (n < 50; studies = 15), which may have limited their statistical power to detect significant associations. Although we attempted to standardise outcomes across studies, five and 23 different outcome measures were used in prospective and interventional studies, respectively, preventing the use of meta-analysis here.
5 Conclusions
This review identified a range of predominantly interpersonal and organisational determinants of change in young children’s physical activity; however, only parental monitoring of their child’s physical activity emerged as a consistently positive determinant of change, with provider training positively associated with change in children’s MVPA. Maternal role modelling was also positively associated with change in all three studies in which it was examined. Many determinants were explored in fewer than four studies, and multiple determinants were targeted within each interventional study. This heterogeneity in the determinants considered, and also in outcome measures used, limited the ability to identify consistent evidence for specific determinants. Future work should investigate potentially important lesser-explored or overlooked modifiable family- and childcare-related determinants; explore how determinants influence physical activity throughout the day and week; and deconstruct how the multiple elements within an intervention result in positive behaviour change. Assessment of determinants in the community and policy domains, in addition to studies conducted in developing countries, is also required. Such information will provide more robust evidence about the determinants of change in activity in preschool-aged young children, which is needed to inform the development of successful targeted interventions to increase activity levels in this population.
References
NHS Digital. National Child Measurement Programme—England, 2014–15. 2015. http://content.digital.nhs.uk/searchcatalogue?productid=19405&q=NCMP&sort=Relevance&size=10&page=1#top. Accessed 15 Jan 2016.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90.
Lakshman R, Elks CE, Ong KK. Childhood obesity. Circulation. 2012;126:1770–9.
Herman KM, Craig CL, Gauvin L, et al. Tracking of obesity and physical activity from childhood to adulthood: the Physical Activity Longitudinal Study. Int J Pediatr Obes. 2009;4:281–8.
Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9.
Bluford DA, Sherry B, Scanlon KS. Interventions to prevent or treat obesity in preschool children: a review of evaluated programs. Obesity. 2007;15:1356–72.
Bond M, Wyatt K, Lloyd J, et al. Systematic review of the effectiveness of weight management schemes for the under fives. Obes Rev. 2011;12:242–53.
Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity. 2010;18:S27–35.
Monasta L, Batty GD, Macaluso A, et al. Interventions for the prevention of overweight and obesity in preschool children: a systematic review of randomized controlled trials. Obes Rev. 2011;12:e107–18.
de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91:831–40.
Fitzgibbon M, Stolley M, Schiffer L, et al. Two-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146:618–25.
Mo-suwan L, Pongprapai S, Junjana C, et al. Effects of a controlled trial of a school-based exercise program on the obesity indexes of preschool children. Am J Clin Nutr. 1998;68:1006–11.
Timmons BW, Leblanc AG, Carson V, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37:773–92.
LeBlanc AG, Spence JC, Carson V, et al. Systematic review of sedentary behaviour and health indicators in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37:753–72.
McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77.
Hinkley T, Crawford D, Salmon J, et al. Preschool children and physical activity: a review of correlates. Am J Prev Med. 2008;34:435–41.
Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sport Exerc. 2000;32:963–75.
Brug J, Oenema A, Ferreira I. Theory, evidence and intervention mapping to improve behaviour nutrition and physical activity interventions. Int J Behav Nutr Phys Act. 2005;2:2.
Department of Health. Start active, stay active: a report on physical activity from the four home countries’ Chief Medical Officers. London, UK; 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf. Accessed 29 Nov 2015.
Department of Health and Aging. Get up and grow: healthy eating and physical activity for early childhood. Canberra, ACT: Australian Government; 2010. http://www.health.gov.au/internet/main/publishing.nsf/content/phd-early-childhood-nutrition-resources. Accessed 16 Sept 2016.
Fisher A, Reilly JJ, Kelly LA, et al. Fundamental movement skills and habitual physical activity in young children. Med Sci Sport Exerc. 2005;37:684–8.
Jones R, Okely A. Physical activity recommendations for early childhood. In: Tremblay RE, Boivin M, Peters R, editors. Encyclopedia of early childhood development. Montreal: CEECD, SKC-ECD; 2011.
Reilly JJ. Low levels of objectively measured physical activity in preschoolers in child care. Med Sci Sport Exerc. 2010;42:502–7.
Sallis J, Owen N, Fotheringham MJ. Behavioral epidemiology: a systematic framework to classify phases of research on health promotion and disease prevention. Ann Behav Med. 2000;22:294–8.
De Craemer M, De Decker E, De Bourdeaudhuij I, et al. Correlates of energy balance-related behaviours in preschool children: a systematic review. Obes Rev. 2012;13:13–28.
Mitchell J, Skouteris H, McCabe M, et al. Physical activity in young children: a systematic review of parental influences. Early Child Dev Care. 2012;182:1411–37.
Hinkley T, Salmon J, Okely AD, et al. Correlates of preschool children’s physical activity. Am J Prev Med. 2012;43:159–67.
Li Y, Kwan MYW, King-Dowling S, et al. Determinants of physical activity during early childhood: a systematic review. Adv Phys Educ. 2015;5:116–27.
Lakshman R, Paes V, Hesketh K, et al. Protocol for systematic reviews of determinants/correlates of obesity-related dietary and physical activity behaviors in young children (preschool 0 to 6 years): evidence mapping and syntheses. BMC Syst Rev. 2013;2:28.
Mazarello Paes V, Hesketh K, O’Malley C, et al. Determinants of sugar-sweetened beverage consumption in young children: a systematic review. Obes Rev. 2015;16(11):903–13.
Centre for Reviews and Dissemination (CRD). Systematic reviews: CRD’s guidance for understaking reviews in healthcare. 3rd edn. York, UK: CRD, University of York; 2008.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Thomas J, Sutcliffe K, Harden A, et al. Children and healthy eating: a systematic review of barriers and facilitators. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2003.
Evidence for Policy and Practice Information (EPPI) and Co-ordinating Centre IoE, University of London. EPPI—Centre Methods for Conducting Systematic Reviews. http://eppi.ioe.ac.uk/cms/. Accessed 10 Jul 2015.
Wijndaele K, Lakshman R, Landsbaugh JR, et al. Determinants of early weaning and use of unmodified cow’s milk in infants: a systematic review. JADA. 2009;109:2017–28.
Trost SG, Owen N, Bauman AE, et al. Correlates of adults’ participation in physical activity: review and update. Med Sci Sport Exerc. 2002;34:1996–2001.
Hannon JC, Brown BB. Increasing preschoolers’ physical activity intensities: an activity-friendly preschool playground intervention. Prev Med. 2008;46:532–6.
Trost SG, Fees B, Dzewaltowski D. Feasibility and efficacy of a “move and learn” physical activity curriculum in preschool children. J Phys Act Health. 2008;5:88–103.
Stratton G, Mullan E. The effect of multicolor playground markings on children’s physical activity level during recess. Prev Med. 2005;41:828–33.
Alhassan S, Sirard JR, Robinson TN. The effects of increasing outdoor play time on physical activity in Latino preschool children. Int J Pediatr Obes. 2007;2:153–8.
Cardon G, Labarque V, Smits D, et al. Promoting physical activity at the pre-school playground: the effects of providing markings and play equipment. Prev Med. 2009;48:335–40.
Cottrell L, Spangler-Murphy E, Minor V, et al. A kindergarten cardiovascular risk surveillance study: CARDIAC-Kinder. Am J Health Behav. 2005;29:595–606.
Van Cauwenberghe E, De Bourdeaudhuij I, Maes L, et al. Efficacy and feasibility of lowering playground density to promote physical activity and to discourage sedentary time during recess at preschool: a pilot study. Prev Med. 2012;55:319–21.
O’Dwyer MV, Fairclough SJ, Knowles Z, et al. Effect of a family focused active play intervention on sedentary time and physical activity in preschool children. Int J Behav Nutr Phys Act. 2012;9:117.
O’Dwyer MV, Fairclough SJ, Ridgers ND, et al. Effect of a school-based active play intervention on sedentary time and physical activity in preschool children. Health Educ Res. 2013;28:931–42.
Annesi JJ, Smith A, Tennant G. Effects of a cognitive-behaviourally based physical activity treatment for 4- and 5-year-old children attending US preschools. Int J Behav Med. 2013;20:562–6.
Annesi JJ, Smith AE, Tennant G. Effects of the start for life treatment on physical activity in primarily African American preschool children of ages 3–5 years. Psychol Health Med. 2013;18:300–9.
Engelen L, Bundy AC, Naughton G, et al. Increasing physical activity in young primary school children—it’s child’s play: a cluster randomised controlled trial. Prev Med. 2013;56:319–25.
De Bock F, Genser B, Raat H, et al. A participatory physical activity intervention in preschools: a cluster randomized controlled trial. Am J Prev Med. 2013;45:64–74.
Bonvin A, Barral J, Kakebeeke TH, et al. Effect of a governmentally-led physical activity program on motor skills in young children attending child care centers: a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:90.
Jones R, Riethmuller A, Hesketh K, et al. Promoting fundamental movement skill development and physical activity in early childhood settings: a cluster randomized controlled trial. Pediatr Exerc Sci. 2011;23:600–15.
Alhassan S, Nwaokelemeh O, Ghazarian M, et al. Effects of locomotor skill program on minority preschoolers’ physical activity levels. Pediatr Exerc Sci. 2012;24:435–49.
Alhassan S, Nwaokelemeh O, Lyden K, et al. A pilot study to examine the effect of additional structured outdoor playtime on preschoolers’ physical activity levels. Child Care Pract. 2013;19:23–35.
Annesi JJ, Smith AE, Tennant G. Cognitive-behavioural physical activity treatment in African-American pre-schoolers: effects of age, sex, and BMI. J Paediatr Child Health. 2013;49:E128–32.
Fitzgibbon ML, Stolley MR, Schiffer L, et al. Diet and physical activity Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14:1616–25.
Fitzgibbon ML, Stolley MR, Schiffer L, et al. Hip-Hop to Health Jr. obesity prevention effectiveness trial: postintervention results. Obesity. 2011;19:994–1003.
Whaley SE, McGregor S, Jiang L, et al. A WIC-based intervention to prevent early childhood overweight. J Nutr Educ Behav. 2010;42:S47–51.
Klohe-Lehman DM, Freeland-Graves J, Clarke KK, et al. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. J Am Coll Nutr. 2007;26:196–208.
Telford A, Salmon J, Timperio A, et al. Examining physical activity among 5- to 6- and 10- to 12-year-old children: the children’s leisure activities study. Pediatr Exerc Sci. 2005;17:266–80.
Ball K, Cleland VJ, Timperio AF, et al. Socioeconomic position and children’s physical activity and sedentary behaviors: longitudinal findings from the CLAN study. J Phys Act Health. 2009;6:289–98.
Cleland V, Timperio A, Salmon J, et al. A longitudinal study of the family physical activity environment and physical activity among youth. Am J Health Promot. 2011;25:159–67.
Cleland V, Crawford D, Baur LA, et al. A prospective examination of children’s time spent outdoors, objectively measured physical activity and overweight. Int J Obes. 2008;32:1685–93.
De Bock F, Fischer JE, Hoffmann K, et al. A participatory parent-focused intervention promoting physical activity in preschools: design of a cluster-randomized trial. BMC Public Health. 2010;10:49.
De Craemer M, De Decker E, Verloigne M, et al. The effect of a kindergarten-based, family-involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: the ToyBox-study. Int J Behav Nutr Phys Act. 2014;11:38.
Eliakim A, Nemet D, Balakirski Y, et al. The effects of nutritional-physical activity school-based intervention on fatness and fitness in preschool children. J Pediatr Endocrinol Metab. 2007;20:711–8.
Yin Z, Ph D, Parra-Medina D, et al. Míranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child Obes. 2012;8:429–39.
Bellows LL, Davies PL, Anderson J, et al. Effectiveness of a physical activity intervention for Head Start preschoolers: a randomized intervention study. Am J Occup Ther. 2013;67:28–36.
Davison KK, Lawson HA, Coatsworth JD. The family-centered action model of intervention layout and implementation (FAMILI): the example of childhood obesity. Health Promot Pract. 2012;13:454–61.
Davis AM, Gallagher K, Taylor M, et al. An in-home intervention to improve nutrition, physical activity, and knowledge among low-income teen mothers and their children: results from a pilot study. J Dev Behav Pediatr. 2013;34:609–15.
Verbestel V, De Coen V, Van Winckel M, et al. Prevention of overweight in children younger than 2 years old: a pilot cluster-randomized controlled trial. Public Health Nutr. 2013;17(6):1–9.
De Coen V, De Bourdeaudhuij I, Vereecken C, et al. Effects of a 2-year healthy eating and physical activity intervention for 3–6-year-olds in communities of high and low socio-economic status: the POP (Prevention of Overweight among Pre-school and school children) project. Public Health Nutr. 2012;15:1737–45.
Elder JP, Crespo NC, Corder K, et al. Childhood obesity prevention and control in city recreation centres and family homes: the MOVE/me Muevo Project. Pediatr Obes. 2014;9:218–31.
Fitzgibbon MML, Stolley MMR, Schiffer L, et al. Family-based Hip-Hop to Health: outcome results. Obesity. 2013;21:1–19.
Ostbye T, Krause KMK, Stroo M, et al. Parent-focused change to prevent obesity in preschoolers: results from the KAN-DO study. Prev Med. 2013;55:188–95.
Puder JJ, Marques-Vidal P, Schindler C, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ. 2011;343:d6195.
Stark LJ, Spear S, Boles R, et al. A pilot randomized controlled trial of a clinic and home-based behavioral intervention to decrease obesity in preschoolers. Obesity. 2011;19:134–41.
Saakslahti A, Numminen P, Varstala V, et al. Physical activity as a preventive measure for coronary heart disease risk factors in early childhood. Scand J Med Sci Sports. 2004;14:143–9.
Taylor RW, Murdoch L, Carter P, et al. Longitudinal study of physical activity and inactivity in preschoolers: the FLAME study. Med Sci Sport Exerc. 2009;41:96–102.
Reilly JJ, Jackson DM, Montgomery C, et al. Total energy expenditure and physical activity in young Scottish children: mixed longitudinal study. Lancet. 2004;363:211–2.
Bellows L, Anderson J. The Food Friends Get Movin’ with Mighty Moves: a physical activity program for preschoolers. J Nutr Educ Behav. 2013;45:473–5.
Davison K, Jurkowski J, Li K, et al. A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act. 2013;10:3.
Østbye T, Malhotra R, Stroo M, et al. The effect of the home environment on physical activity and dietary intake in preschool children. Int J Obes. 2013;37:1314–21.
Jones R, Wells M, Okely A, et al. Is an online healthy lifestyles program acceptable for parents of preschool children? Nutr Diet. 2011;68:149–54.
Wen LM, Baur LA, Simpson JM, et al. Sustainability of effects of an early childhood obesity prevention trial over time. JAMA Pediatr. 2015;169:543.
Craggs C, Corder K, van Sluijs EMF, et al. Determinants of change in physical activity in children and adolescents: a systematic review. Am J Prev Med. 2011;40:645–58.
Ornelas IJ, Perreira KM, Ayala GX. Parental influences on adolescent physical activity: a longitudinal study. Int J Behav Nutr Phys Act. 2007;4:3.
Hennessy E, Hughes SO, Goldberg JP, et al. Parent–child interactions and objectively measured child physical activity: a cross-sectional study. Int J Behav Nutr Phys Act. 2010;7:71.
Hesketh KR, McMinn AM, Griffin SJ, et al. Maternal awareness of young children’s physical activity: levels and cross-sectional correlates of overestimation. BMC Public Health. 2013;13:924.
Hessler K. Physical activity behaviors of rural preschoolers. Pediatr Nurs. 2009;35:246–53.
Irwin JD, He M, Bouck LM, et al. Preschoolers’ physical activity behaviours: parents’ perspectives. Can J Public Health. 2005;96:299–303.
Pagnini DL, Wilkenfeld RL, King LA, et al. Mothers of pre-school children talk about childhood overweight and obesity: the Weight of Opinion Study. J Paediatr Child Health. 2007;43:806–10.
Stenhammar C, Wells M, Ahman A, et al. “Children are exposed to temptation all the time”—parents’ lifestyle-related discussions in focus groups. Acta Paediatr. 2011;101:208–15.
Ferrari M, Tweed S, Anneke Rummens J, et al. Health materials and strategies for the prevention of immigrants’ weight-related problems. Qual Health Res. 2009;19:1259–72.
Seal N, Yurkovich E. Physical activity within rural families of overweight preschool children: a pilot. Online J Rural Nurs Health Care. 2009;9:56–68.
Hesketh KR, Goodfellow L, Ekelund U, et al. Activity levels in mothers and their preschool children. Pediatrics. 2014;133:e973–80.
Moore LL, Lombardi DA, White MJ, et al. Influence of parents’ physical activity levels on activity levels of young children. J Pediatr. 1991;118:215–9.
Oliver M, Schofield GM, Schluter PJ. Parent influences on preschoolers’ objectively assessed physical activity. J Sci Med Sport. 2010;13:403–9.
Trost SG, Ward DS, Senso M. Effects of child care policy and environment on physical activity. Med Sci Sport Exerc. 2010;42:520–5.
Copeland KA, Kendeigh CA, Saelens BE, et al. Physical activity in child-care centers: do teachers hold the key to the playground? Health Educ Res. 2011;27:81–100.
Pagnini D, Wilkenfeld R, King L, et al. Early childhood sector staff perceptions of child overweight and obesity: the Weight of Opinion Study. Health Promot J Aust. 2007;18:149–54.
Cammisa M, Montrone R, Caroli M. Development and results of a new methodology to perform focus group with preschool children on their beliefs and attitudes on physical activity. Int J Pediatr Obes. 2011;6(Suppl 2):22–7.
van Zandvoort M, Tucker P, Irwin JD, et al. Physical activity at daycare: issues, challenges and perspectives. Early years. 2010;30:175–88.
De Craemer M, De Decker E, De Bourdeaudhuij I, et al. Physical activity and beverage consumption in preschoolers: focus groups with parents and teachers. BMC Public Health. 2013;13:278.
Hesketh KR, van Sluijs EM, Blaine RE, et al. Assessing care providers’ perceptions and beliefs about physical activity in infants and toddlers: baseline findings from the Baby NAP SACC study. BMC Public Health. 2015;15:1–7.
Prioreschi A, Micklesfield LK. A scoping review examining physical activity measurement and levels in the first 2 years of life. Child Care Health Dev. 2016;42(6):775–83.
Wen LM, Baur LA, Simpson JM, et al. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. BMJ. 2012;344:e3732.
Acknowledgements
The authors gratefully acknowledge the helpful comments provided by Prof. Simon Griffin and the three anonymous reviewers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This is independent research funded by the UK National Institute for Health Research School for Public Health Research (NIHR SPHR). The views expressed are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health. The NIHR SPHR is a partnership between the Universities of Sheffield, Bristol, Cambridge, UCL; The London School for Hygiene and Tropical Medicine; The Peninsula College of Medicine and Dentistry; the LiLaC collaboration between the Universities of Liverpool and Lancaster; and Fuse, the Centre for Translational Research in Public Health, a collaboration between Newcastle, Durham, Northumbria, Sunderland and Teesside Universities. This work was also supported by the Medical Research Council [Unit Programme numbers MC_UU_12015/7 and MC_UU_12015/2], and undertaken under the auspices of the Centre for Diet and Activity Research, a United Kingdom Clinical Research Collaboration (UKCRC) Public Health Research Centre of Excellence which is funded by the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the NIHR, and the Wellcome Trust (RES-590-28-0002). KH is a Sir Henry Wellcome Postdoctoral Fellow (Wellcome Trust Grant 107337/Z/15/Z).
Conflict of interest
Kathryn Hesketh, Claire O’Malley, Veena Mazarello Paes, Helen Moore, Carolyn Summerbell, Ken Ong, Rajalakshmi Lakshman and Esther van Sluijs declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hesketh, K.R., O’Malley, C., Paes, V.M. et al. Determinants of Change in Physical Activity in Children 0–6 years of Age: A Systematic Review of Quantitative Literature. Sports Med 47, 1349–1374 (2017). https://doi.org/10.1007/s40279-016-0656-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-016-0656-0