Abstract
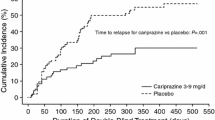
Brexpiprazole (Rxulti®, Rexulti®) is an oral atypical antipsychotic agent approved for the treatment of schizophrenia in the EU (in adult patients) and the USA, as well as in some other countries, including Japan. Like aripiprazole, it is a partial agonist at dopamine D2 and serotonin 5-HT1A receptors and an antagonist at serotonin 5-HT2A receptors. However, brexpiprazole displays less intrinsic activity at D2 receptors and, coupled with actions at 5HT1A, 5HT2A and noradrenaline α1B receptors that are at least as potent as its action at D2 receptors, is predicted to demonstrate a lower propensity for activating adverse events and extrapyramidal symptoms than aripiprazole. Brexpiprazole 2–4 mg/day produced statistically significant and clinically meaningful improvements in overall symptomatology and psychosocial functioning compared with placebo in adults with acute exacerbation of schizophrenia. As maintenance treatment, brexpiprazole 1–4 mg/day significantly delayed the time to relapse compared with placebo in patients who were already stabilized on the drug and was associated with stabilization or continued improvement in patients’ symptoms and functioning. Brexpiprazole was generally well tolerated, exhibiting an adverse event profile characterized by a relatively low incidence of activating and sedating adverse effects, small changes in QT interval and metabolic parameters that were not clinically significant, and moderate weight gain. Clinical evidence to date suggests it usefully extends the range of therapeutic options for schizophrenia.

Similar content being viewed by others
References
Stepnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia. Molecules. 2018;23(8):2087.
Chong HY, Teoh SL, Wu DB, et al. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–73.
Remington G, Addington D, Honer W, et al. Guidelines for the pharmacotherapy of schizophrenia in adults. Can J Psychiatry. 2017;62(9):604–16.
Grover S, Chakrabarti S, Kulhara P, et al. Clinical practice guidelines for management of schizophrenia. Indian J Psychiatry. 2017;59:19–33.
Keating D, McWilliams S, Schneider I, et al. Pharmacological guidelines for schizophrenia: a systematic review and comparison of recommendations for the first episode. BMJ Open. 2017;7:e013881.
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78.
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J Biol Psychiatry. 2013;14(1):2–44.
van Os J, Kapur S. Schizophrenia. Lancet. 2009;374(9690):635–45.
Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms in schizophrenia: an update. Curr Treat Options Psychiatry. 2016;3:133–50.
Hill SK, Bishop JR, Palumbo D, et al. Effect of second-generation antipsychotics on cognition: current issues and future challenges. Expert Rev Neurother. 2010;10(1):43–57.
Nielsen RE, Levander S, Kjaersdam Telléus G, et al. Second-generation antipsychotic effect on cognition in patients with schizophrenia—a meta-analysis of randomized clinical trials. Acta Psychiatr Scand. 2015;131(3):185–96.
Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114:169–79.
Solmi M, Murru A, Pacchiarotti I, et al. Safety, tolerability, and risks associated with first- and second-generation antipsychotics: a state-of-the-art clinical review. Ther Clin Risk Manag. 2017;13:757–77.
Correll CU. From receptor pharmacology to improved outcomes: individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry. 2010;25(Suppl 2):S12–21.
Barnes TR, Schizophrenia Consensus Group of British Association for Psychopharmacology. Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2011;25:567–620.
Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62.
Patel KR, Cherian J, Gohil K, et al. Schizophrenia: overview and treatment options. Pharm Ther. 2014;39(9):638–45.
Leucht S, Cipriani A, Spineli L, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;382(9896):951–62.
Das S, Barnwal P, Winston A, et al. Brexpiprazole: so far so good. Ther Adv Psychopharmacol. 2016;6(1):39–54.
Garnock-Jones KP. Brexpiprazole: a review in schizophrenia. CNS Drugs. 2016;30(4):335–42.
Maeda K, Sugino H, Akazawa H, et al. Brexpiprazole I: in vitro and in vivo characterization of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. 2014;350(3):589–604.
Maeda K, Lerdrup L, Sugino H, et al. Brexpiprazole II: antipsychotic-like and procognitive effects of a novel serotonin-dopamine activity modulator. J Pharmacol Exp Ther. 2014;350(3):605–14.
Stahl SM. Mechanism of action of brexpiprazole: comparison with aripiprazole. CNS Spectr. 2016;21:1–6.
Croxtall JD. Aripiprazole: a review of its use in the management of schizophrenia in adults. CNS Drugs. 2012;26(2):155–83.
Hope J, Castle D, Keks NA. Brexpiprazole: a new leaf on the partial dopamine agonist branch. Australas Psychiatry. 2018;26(1):92–4.
European Medicines Agency. RXULTI 0.24–4 mg film coated tablets: EU summary of product characteristics. 2018. https://www.ema.europa.eu. Accessed 19 Sept 2018.
Otsuka Pharmaceutical Co Ltd. REXULTI® (brexpiprazole) tablets, for oral use: US prescribing information. 2015. https://www.accessdata.fda.gov. Accessed 20 Sept 2018.
Otsuka Pharmaceutical Co., Ltd. REXULTI® 1 mg, 2 mg tablets: Japanese prescribing information. 2018. http://www.pmda.go.jp. Accessed 19 Dec 2018.
McKeage KA. Adjunctive brexpiprazole: a review in major depressive disorder. CNS Drugs. 2016;30(2):91–9.
Marder SR, Hakala MJ, Gislum M, et al. An interventional, multicenter, randomized, double-blind, placebo-controlled, active reference, flexible dose study of brexpiprazole in adults with acute schizophrenia [abstract no. FC71]. In: 24th European Congress of Psychiatry; 2016.
US National Institutes of Health. ClinicalTrials.gov identifier NCT01810380. 2017.http://www.clinicaltrials.gov. Accessed 5 Sept 2018.
Kane JM, Skuban A, Ouyang J, et al. A multicenter, randomized, double-blind, controlled phase 3 trial of fixed-dose brexpiprazole for the treatment of adults with acute schizophrenia. Schizophr Res. 2015;164(1–3):127–35.
Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2015;172(9):870–80.
Ishigooka J, Iwashita S, Tadori Y. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia in Japan: a 6-week, randomized, double-blind, placebo-controlled study. Psychiatry Clin Neurosci. 2018;72(9):692–700.
Marder SR, Hakala MJ, Josiassen MK, et al. Brexpiprazole in patients with schizophrenia: overview of short- and long-term phase 3 controlled studies. Acta Neuropsychiatr. 2017;29(5):278–90.
Correll CU, Skuban A, Hobart M, et al. Efficacy of brexpiprazole in patients with acute schizophrenia: review of three randomized, double-blind, placebo-controlled studies. Schizophr Res. 2016;174(1–3):82–92.
Weiss C, Therrien F, Jin N, et al. Effect of brexpiprazole on patient functioning in patients with acute exacerbation of schizophrenia: results from three short-term, randomized, double-blind, placebo-controlled studies [abstract no. M211]. Neuropsychopharmacology. 2017;43(Suppl 1):S246–7.
Weiss C, MacKenzie E, Therrien F, et al. Symptomatic and functional response to brexpiprazole treatment in patients with acute schizophrenia by age [abstract no. T50]. Schizophr Bull. 2018;44(Suppl 1):S133.
Citrome L, Ota A, Nagamizu K, et al. The effect of brexpiprazole (OPC-34712) and aripiprazole in adult patients with acute schizophrenia: results from a randomized, exploratory study. Int Clin Psychopharmacol. 2016;31(4):192–201.
US National Institutes of Health. ClinicalTrials.gov identifier NCT02054702. 2015. http://www.clinicaltrials.gov. Accessed 21 Sept 2018.
Meade N, Shi L, Meehan S, et al. Efficacy and safety of brexpiprazole in patients with schizophrenia presenting with severe psychotic symptoms during an acute exacerbation [abstract no. 124 plus poster]. In: 29th Annual US Psychiatric and Mental Health Congress; 2018.
Fleischhacker WW, Hobart M, Ouyang J, et al. Efficacy and safety of brexpiprazole (OPC-34712) as maintenance treatment in adults with schizophrenia: a randomized, double-blind, placebo-controlled study. Int J Neuropsychopharmacol. 2017;20(1):11–21.
Therrien F, Weiss C, Jin N, et al. Effect of brexpiprazole on patient functioning in patients with schizophrenia: results from a long-term, randomized, double-blind, placebo-controlled, maintenance study [abstract no. M208]. Neuropsychopharmacology. 2017;43(Suppl 1):S244–5.
Weiller E, Hobart M, Pfister S, et al. Effect of brexpiprazole on long-term remission in adults with schizophrenia: results from a randomized, double-blind, placebo-controlled, maintenance study [abstract no. SU115]. Schizophr Bull. 2017;43(Suppl 1):S202–3.
Hakala M, Gislum M, Skuban A, et al. Long-term safety and tolerability of brexpiprazole in patients with schizophrenia [abstract no. O7.5]. Schizophr Bull. 2018;44(Suppl 1):S94–5.
Ishigooka J, Iwashita S, Tadori Y, et al. Long-term safety and effectiveness of brexpiprazole in Japanese patients with schizophrenia: a 52-week, open-label study. Psychiatry Clin Neurosci. 2018;72(6):445–53.
Forbes A, Hobart M, Ouyang J, et al. A long-term, open-label study to evaluate the safety and tolerability of brexpiprazole as maintenance treatment in adults with schizophrenia. Int J Neuropsychopharmacol. 2018;21(5):433–41.
Baker R, Jin N, Weiller E, et al. Effect of brexpiprazole on long-term remission in adults with schizophrenia: results of an open-label, long-term study [abstract no P.3.d.037]. Eur Neuropsychopharmacol. 2017;27(Suppl 4):S952.
Kane JM, Skuban A, Hobart M, et al. Overview of short- and long-term tolerability and safety of brexpiprazole in patients with schizophrenia. Schizophr Res. 2016;174:93–8.
Eramo A, Skuban A, Ouyang J, et al. Incidence, onset, duration and severity of akathisia with brexpiprazole (OPC-34712) in acute schizophrenia: a pooled analysis of two pivotal studies [poster no. 78]. In: American Society of Clinical Psychopharmacology Annual Meeting; 2015.
Ivkovic J, Lindsten A, George V, et al. Effect of brexpiprazole on prolactin: an analysis of short- and long-term studies in schizophrenia. J Clin Psychopharmacol. 2019;39(1):13–9.
Newcomer JW, Eriksson H, Zhang P, et al. Changes in metabolic parameters and body weight in brexpiprazole-treated patients with acute schizophrenia: pooled analyses of phase 3 clinical studies. Curr Med Res Opin. 2018;34(12):2197–205.
Citrome L. The ABC’s of dopamine receptor partial agonists—aripiprazole, brexpiprazole and cariprazine: the 15-min challenge to sort these agents out. Int J Clin Pract. 2015;69(11):1211–20.
Frankel JS, Schwartz TL. Brexpiprazole and cariprazine: distinguishing two new atypical antipsychotics from the original dopamine stabilizer aripiprazole. Ther Adv Psychopharmacol. 2017;7(1):29–41.
Garnock-Jones KP. Cariprazine: a review in schizophrenia. CNS Drugs. 2017;31:513–25.
Bak M, Fransen A, Janssen J, et al. Almost all antipsychotics result in weight gain: a meta-analysis. PLoS One. 2014;9(4):e94112.
Ribeiro ELA, de Mendonça Lima T, Vieira MEB, et al. Efficacy and safety of aripiprazole for the treatment of schizophrenia: an overview of systematic reviews. Eur J Clin Pharmacol. 2018;74(10):1215–33.
Oh GH, Yu JC, Choi KS, et al. Simultaneous comparison of efficacy and tolerability of second-generation antipsychotics in schizophrenia: mixed-treatment comparison analysis based on head-to-head trial data. Psychiatry Investig. 2015;12:46–54.
Kane JM, Barnes TR, Correll CU, et al. Evaluation of akathisia in patients with schizophrenia, schizoaffective disorder, or bipolar I disorder: a post hoc analysis of pooled data from short- and long-term aripiprazole trials. J Psychopharmacol. 2010;24(7):1019–29.
Nasrallah HA. Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles. Mol Psychiatr. 2008;13:27–35.
Stahl SM. Mechanism of action of cariprazine. CNS Spectr. 2016;21:123–7.
Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161(2 Suppl):1–56.
Citrome L. Activating and sedating adverse effects of second-generation antipsychotics in the treatment of schizophrenia and major depressive disorder: absolute risk increase and number needed to harm. J Clin Psychopharmacol. 2017;37(2):138–47.
Weiss C, Weiller E, Baker RA, et al. The effects of brexpiprazole and aripiprazole on body weight as monotherapy in patients with schizophrenia and as adjunctive treatment in patients with major depressive disorder: an analysis of short-term and long-term studies. Int Clin Psychopharmacol. 2018;33(5):255–60.
Ng-Mak D, Tongbram V, Ndirangu K, et al. Efficacy and metabolic effects of lurasidone versus brexpiprazole in schizophrenia: a network meta-analysis. J Comp Eff Res. 2018. https://doi.org/10.2217/cer-2018-0016.
Oosterhof CA, El Mansari M, Blier P. Acute effects of brexpiprazole on serotonin, dopamine, and norepinephrine systems: an in vivo electrophysiologic characterization. J Pharm Exp Ther. 2014;351(3):585–95.
Yoshimi N, Fujita Y, Ohgi Y, et al. Effects of brexpiprazole, a novel serotonin-dopamine activity modulator, on phencyclidine-induced cognitive deficits in mice: a role for serotonin 5-HT1A receptors. Pharmacol Biochem Behav. 2014;124(Suppl C):245–9.
Yoshimi N, Futamura T, Hashimoto K. Improvement of dizocilpine-induced social recognition deficits in mice by brexpiprazole, a novel serotonin-dopamine activity modulator. Eur Neuropsychopharmacol. 2015;25(3):356–64.
Oosterhof CA, El Mansari M, Bundgaard C, et al. Brexpiprazole alters monoaminergic systems following repeated administration: an in vivo electrophysiological study. Int J Neuropsychopharmacol. 2015;19(3):1–12.
Acknowledgements
During the peer review process, the manufacturer of brexpiprazole was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
James Frampton is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
The manuscript was reviewed by: S. Das, Department of Clinical Pharmacology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India; M. Markovic, Department of Pharmacy, Hackensack University Medical Center, Hackensack Meridian Health, Hackensack, NJ, USA; P. Stępnicki, Department of Synthesis and Chemical Technology of Pharmaceutical Substances, Medical University of Lublin, Poland.
Rights and permissions
About this article
Cite this article
Frampton, J.E. Brexpiprazole: A Review in Schizophrenia. Drugs 79, 189–200 (2019). https://doi.org/10.1007/s40265-019-1052-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-1052-5