Abstract
Background
Methods for near-real-time monitoring of new drugs in electronic healthcare data are needed.
Objective
In a novel application, we prospectively monitored ischemic, bleeding, and mortality outcomes among patients initiating prasugrel versus clopidogrel in routine care during the first 2 years following the approval of prasugrel.
Methods
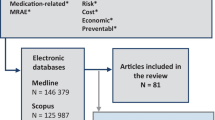
Using the HealthCore Integrated Research Database, we conducted a prospective cohort study comparing prasugrel and clopidogrel initiators in the 6 months following the introduction of prasugrel and every 2 months thereafter. We identified patients who initiated antiplatelets within 14 days following discharge from hospitalizations for myocardial infarction (MI) or acute coronary syndrome. We matched patients using high-dimensional propensity scores (hd-PSs) and followed them for ischemic (i.e., MI and ischemic stroke) events, bleed (i.e., hemorrhagic stroke and gastrointestinal bleed) events, and all-cause mortality. For each outcome, we applied sequential alerting algorithms.
Results
We identified 1,282 eligible new users of prasugrel and 8,263 eligible new users of clopidogrel between September 2009 and August 2011. In hd-PS matched cohorts, the overall MI rate difference (RD) comparing prasugrel with clopidogrel was −23.1 (95 % confidence interval [CI] −62.8–16.7) events per 1,000 person-years and RDs were −0.5 (−12.9–11.9) and −2.8 (−13.2–7.6) for a composite bleed event outcome and death from any cause, respectively. No algorithms generated alerts for any outcomes.
Conclusions
Near-real-time monitoring was feasible and, in contrast to the key pre-marketing trial that demonstrated the efficacy of prasugrel, did not suggest that prasugrel compared with clopidogrel was associated with an increased risk of gastrointestinal and intracranial bleeding.






Similar content being viewed by others
References
Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–15.
Bhatt DL. Prasugrel in clinical practice. N Engl J Med. 2009;361:940–2.
Schneeweiss S. Developments in post-marketing comparative effectiveness research. Clin Pharmacol Ther. 2007;82:143–56.
Wiviott SD, Antman EM, Gibson CM, et al. Evaluation of prasugrel compared with clopidogrel in patients with acute coronary syndromes: design and rationale for the TRial to assess Improvement in Therapeutic Outcomes by optimizing platelet InhibitioN with prasugrel Thrombolysis In Myocardial Infarction 38 (TRITON-TIMI 38). Am Heart J. 2006;152:627–35.
Schneeweiss S, Gagne JJ, Glynn RJ, Ruhl M, Rassen JA. Assessing the comparative effectiveness of newly marketed medications: methodological challenges and implications for drug development. Clin Pharmacol Ther. 2011;90:777–90.
Resnic FS, Gross TP, Marinac-Dabic D, et al. Automated surveillance to detect postprocedure safety signals of approved cardiovascular devices. JAMA. 2010;304:2019–27.
Wahl PM, Gagne JJ, Wasser TE, et al. Early steps in the development of a claims-based targeted healthcare safety monitoring system and application to three empirical examples. Drug Saf. 2012;35:407–16.
Gagne JJ, Glynn RJ, Rassen JA, et al. Active safety monitoring of newly marketed medications in a distributed data network: application of a semi-automated monitoring system. Clin Pharmacol Ther. 2012;92:80–6.
Gagne JJ, Rassen JA, Walker AM, Glynn RJ, Schneeweiss S. Active safety monitoring of new medical products using electronic healthcare data: selecting alerting rules. Epidemiology. 2012;23:238–46.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158:915–20.
Schneeweiss S. A basic study design for expedited safety signal evaluation based on electronic healthcare data. Pharmacoepidemiol Drug Saf. 2010;19:858–68.
Wahl PM, Rodgers K, Schneeweiss S, et al. Validation of claims-based diagnostic and procedure codes for cardiovascular and gastrointestinal serious adverse events in a commercially-insured population. Pharmacoepidemiol Drug Saf. 2010;19:596–603.
Tirschwell DL, Longstreth WT Jr. Validating administrative data in stroke research. Stroke. 2002;33:2465–70.
Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ. Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol. 2001;154:854–64.
Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64:749–59.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20:512–22.
Rassen JA, Schneeweiss S. Using high-dimensional propensity scores to automate confounding control in a distributed medical product safety surveillance system. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):41–9.
Toh S, Gagne JJ, Rassen JA, Fireman BH, Kulldorff M, Brown JS. Confounding adjustment in comparative effectiveness research conducted within distributed research networks. Med Care. 2013;51:S4–10.
Rassen JA, Glynn RJ, Brookhart MA, Schneeweiss S. Covariate selection in high-dimensional propensity score analyses of treatment effects in small samples. Am J Epidemiol. 2011;173:1404–13.
Gagne JJ, Walker AM, Glynn RJ, Rassen JA, Schneeweiss S. An event-based approach for comparing the performance of methods for prospective medical product monitoring. Pharmacoepidemiol Drug Saf. 2012;21:631–9.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 273–4.
Goldberg NH, Schneeweiss S, Kowal MK, Gagne JJ. Availability of comparative efficacy data at the time of drug approval in the United States. JAMA. 2011;305:1786–9.
Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012;367(14):1297–309.
Gagne JJ, Fireman B, Ryan PB, et al. Design considerations in an active medical product safety monitoring system. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):32–40.
Choudhry NK, Avorn J, Glynn RJ, et al. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–97.
Dregan A, Toschke MA, Wolfe CD, Rudd A, Ashworth M, Gulliford MC. Utility of electronic patient records in primary care for stroke secondary prevention trials. BMC Public Health. 2011;11:86.
Staa TP, Goldacre B, Gulliford M, et al. Pragmatic randomised trials using routine electronic health records: putting them to the test. BMJ. 2012;344:e55.
Gagne JJ. You can observe a lot (about medical products) by watching (those who use them). Epidemiology. 2013;24:700–2.
Gagne JJ, Bykov K, Willke RJ, Kahler KH, Subedi P, Schneeweiss S. Treatment dynamics of newly marketed drugs and implications for comparative effectiveness research. Value Health. 2013;16:1054–62.
Behrman RE, Benner JS, Brown JS, McClellan M, Woodcock J, Platt R. Developing the sentinel system—a national resource for evidence development. N Engl J Med. 2011;364:498–9.
Platt R, Carnahan RM, Brown JS, et al. The U.S. Food and Drug Administration‘s Mini-Sentinel program: status and direction. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):1–8.
Acknowledgments
This work was presented as a poster at the 28th International Conference on Pharmacoepidemiology and Therapeutic Risk Management, August 2012, Barcelona, Spain, and as a symposium presentation at the International Society for Pharmacoepidemiology Mid-Year Meeting, April 2013, Munich, Germany. Funded by the National Library of Medicine (RO1-LM010213), the National Center for Research Resources (RC1-RR028231), the National Heart Lung and Blood Institute (RC4-HL106373), and HealthCore Inc. through the Brigham-HealthCore Methods Development Collaboration. Dr. Rassen was supported by a career development award from the Agency for Healthcare Research and Quality (AHRQ) (K01-HS018088). Dr. Schneeweiss was the Principal Investigator of the Brigham and Women’s Hospital DEcIDE Center on Comparative Effectiveness Research and the DEcIDE Methods Center, both funded by the AHRQ. No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Drs. Gagne, Rassen, and Schneeweiss are co-investigators of the FDA-funded Mini-Sentinel project (PI: Dr. Richard Platt); however, no FDA funding supported this research and the opinions expressed here are those of the authors and not necessarily of Mini-Sentinel or the FDA. Dr. Schneeweiss is PI of investigator-initiated grants from Pfizer, Novartis, and Boehringer-Ingelheim to the Brigham and Women’s Hospital. Dr. Bohn served as a consultant to Sanofi prior to the development of this manuscript. Dr. Sridhar is employee of HealthCore. Dr. Daniel was an employee of HealthCore during part of the study period. Ms. Patrick and Dr. Choudhry have no other relevant conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gagne, J.J., Rassen, J.A., Choudhry, N.K. et al. Near-Real-Time Monitoring of New Drugs: An Application Comparing Prasugrel Versus Clopidogrel. Drug Saf 37, 151–161 (2014). https://doi.org/10.1007/s40264-014-0136-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-014-0136-0