Abstract
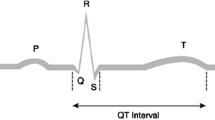
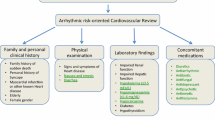
The development of tyrosine kinase inhibitors (TKI) represents a major milestone in oncology. However, their use has been found to be associated with serious toxicities that impinge on various vital organs including the heart. Sixteen TKIs have been approved for use in oncology as of 30 September 2012, and a large number of others are in development or under regulatory review. Cardiovascular safety of medicinal products is a major public health issue that has concerned all the stakeholders. This review focuses on three specific cardiovascular safety aspects of TKIs, namely their propensity to induce QT interval prolongation, left ventricular (LV) dysfunction and hypertension (both systemic and pulmonary). Analyses of information in drug labels, the data submitted to the regulatory authorities and the published literature show that a number of TKIs are associated with these undesirable effects. Whereas LV dysfunction and systemic hypertension are on-target effects related to the inhibition of ligand-related signalling pathways, QT interval prolongation appears to be an off-target class III electrophysiologic effect, possibly related to the presence of a fluorine-based pharmacophore. If not adequately managed, these cardiovascular effects significantly increase the morbidity and mortality in a population already at high risk. Hitherto, the QT effect of most QT-prolonging TKIs (except lapatinib, nilotinib, sunitinib and vandetanib) is relatively mild at clinical doses and has not led to appreciable morbidity clinically. In contrast, LV dysfunction and untreated hypertension have resulted in significant morbidity. Inevitably, dilemmas arise in determining the risk/benefit of a TKI therapy in an individual patient who develops any of these effects following the treatment of the TKI-sensitive cancer. QT interval prolongation, hypertension and LV dysfunction can be managed effectively by using reliable methods of measurement and careful monitoring of patients whose clinical management requires optimisation by a close collaboration between an oncologist and a cardiologist, an evolving subspecialty referred to as cardio-oncology. Despite their potential adverse clinical impact, the effects of TKIs on hypertension and LV function are generally inadequately characterised during their development. As has been the case with QT liability of drugs, there is now a persuasive case for a regulatory requirement to study TKIs systematically for these effects. Furthermore, since most of these novel drugs are studied in trials with relatively small sample sizes and approved on an expedited basis, there is also a compelling case for their effective pharmacovigilance and on-going reassessment of their risk/benefit after approval.
Similar content being viewed by others
References
Krause DS, Van Etten RA. Tyrosine kinases as targets for cancer therapy. N Engl J Med. 2005;353:172–87.
Strevel EL, Siu LL. Cardiovascular toxicity of molecularly targeted agents. Eur J Cancer. 2009;45(Suppl 1):318–31.
des Guetz G, Uzzan B, Chouahnia K, et al. Cardiovascular toxicity of anti-angiogenic drugs. Target Oncol. 2011;6:197–202.
Shah RR. The significance of QT interval in drug development. Br J Clin Pharmacol. 2002;54:188–202.
Shah RR. Cardiac repolarisation and drug regulation: assessing cardiac safety 10 years after the CPMP guidance. Drug Saf. 2007;30:1093–110.
Shah RR. Drug-induced QT interval prolongation: does ethnicity of the thorough QT study population matter? Br J Clin Pharmacol. 2013;75:347–58.
Committee for Medicinal Products for Human Use. ICH note for guidance: the nonclinical evaluation of the potential for delayed ventricular repolarization (QT interval prolongation) by human pharmaceuticals (ICH S7B) (CHMP/ICH/423/02). EMA, London (2005). http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002841.pdf (Accessed Sep 22 2012).
Committee for Medicinal Products for Human Use. ICH note for guidance: the clinical evaluation of QT/QTc interval prolongation and proarrhythmic potential for non-antiarrhythmic drugs (ICH E14) (CHMP/ICH/2/04). EMA, London (2005). http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002879.pdf (Accessed Sep 22 2012).
Strevel EL, Ing DJ, Siu LL. Molecularly targeted oncology therapeutics and prolongation of the QT interval. J Clin Oncol. 2007;25:3362–71.
Ederhy S, Cohen A, Dufaitre G, et al. QT interval prolongation among patients treated with angiogenesis inhibitors. Target Oncol. 2009;4:89–97.
Garcia-Alvarez A, Garcia-Albeniz X, Esteve J, Rovira M, et al. Cardiotoxicity of tyrosine-kinase-targeting drugs. Cardiovasc Hematol Agents Med Chem. 2010;8:11–21.
Force T, Kolaja KL. Cardiotoxicity of kinase inhibitors: the prediction and translation of preclinical models to clinical outcomes. Nat Rev Drug Discov. 2011;10:111–26.
Qi WX, Min DL, Shen Z, et al. Risk of venous thromboembolic events associated with VEGFR-TKIs: a systematic review and meta-analysis. Int J Cancer 2012 (Epub ahead of print).
Sonpavde G, Je Y, Schutz F, et al. Venous thromboembolic events with vascular endothelial growth factor receptor tyrosine kinase inhibitors: a systematic review and meta-analysis of randomized clinical trials. Crit Rev Oncol Hematol. 2013 (Epub ahead of print).
Choueiri TK, Schutz FA, Je Y, et al. Risk of arterial thromboembolic events with sunitinib and sorafenib: a systematic review and meta-analysis of clinical trials. J Clin Oncol. 2010;28:2280–5.
Schutz FA, Je Y, Richards CJ, et al. Meta-analysis of randomized controlled trials for the incidence and risk of treatment-related mortality in patients with cancer treated with vascular endothelial growth factor tyrosine kinase inhibitors. J Clin Oncol. 2012;30:871–7.
Food and Drug Administration Product Reviews and Labels. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm (Accessed Oct 28 2012).
Food and Drug Administration Oncologic Drugs Advisory Committee Documents. http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/OncologicDrugsAdvisoryCommittee/default.htm (Accessed Oct 28 2012).
European Medicines Agency European Public Assessment Reports Assessment History and Product Information. http://www.emea.europa.eu/ema/index.jsp?curl=pages/medicines/landing/epar_search.jsp&mid=WC0b01ac058001d124 (Accessed Oct 28 2012).
Health Canada Summary Basis of Decision. http://www.hc-sc.gc.ca/dhp-mps/prodpharma/sbd-smd/drug-med/index-eng.php (Accessed Oct 28 2012).
National Cancer Institute NCI Drug Dictionary. http://www.cancer.gov/drugdictionary (Accessed Oct 28 2012). doi:10.1007/s40264-013-0050-x
Chen MH, Kerkela R, Force T. Mechanisms of cardiomyopathy associated with tyrosine kinase inhibitor cancer therapeutics. Circulation. 2008;118:84–95.
Force T. Introduction to cardiotoxicity reviews. Circ Res. 2010;106:19–20.
Scheffler M, Di Gion P, Doroshyenko O, et al. Clinical pharmacokinetics of tyrosine kinase inhibitors: focus on 4-anilinoquinazolines. Clin Pharmacokinet. 2011;50:371–403.
Di Gion P, Kanefendt F, Lindauer A, et al. Clinical pharmacokinetics of tyrosine kinase inhibitors: focus on pyrimidines, pyridines and pyrroles. Clin Pharmacokinet. 2011;50:551–603.
Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9:28–39.
van Cruijsen H, van der Veldt A, Hoekman K. Tyrosine kinase inhibitors of VEGF receptors: clinical issues and remaining questions. Front Biosci. 2009;14:2248–68.
Roodhart JM, Langenberg MH, Witteveen E, et al. The molecular basis of class side effects due to treatment with inhibitors of the VEGF/VEGFR pathway. Curr Clin Pharmacol. 2008;3:132–43.
Shah DR, Shah RR, Morganroth J. Tyrosine kinase inhibitors: Their on-target toxicities as potential indicators of efficacy. Drug Saf. 2013 (in press).
Asnacios A, Naveau S, Perlemuter G. Gastrointestinal toxicities of novel agents in cancer therapy. Eur J Cancer. 2009;45(Suppl 1):332–42.
Dienstmann R, Braña I, Rodon J, et al. Toxicity as a biomarker of efficacy of molecular targeted therapies: focus on EGFR and VEGF inhibiting anticancer drugs. Oncologist. 2011;16:1729–40.
Lu Z, Wu CY, Jiang YP, et al. Suppression of phosphoinositide 3-kinase signalling and alteration of multiple ion currents in drug-induced long QT syndrome. Sci Transl Med. 2012;4:131ra50.
Amir E, Seruga B, Martinez-Lopez J, et al. Oncogenic targets, magnitude of benefit, and market pricing of antineoplastic drugs. J Clin Oncol. 2011;29:2543–9.
Shah RR, Roberts SA, Shah DR. A fresh perspective on comparing the FDA and the CHMP/EMA: approval of antineoplastic tyrosine kinase inhibitors. Br J Clin Pharmacol. 2013. doi:10.1111/bcp.12085.
Sanguinetti MC, Jiang C, Curran ME, et al. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell. 1995;81:299–307.
Vandenberg JI, Perry MD, Perrin MJ, et al. hERG K(+) channels: structure, function, and clinical significance. Physiol Rev. 2012;92:1393–478.
Milon D, Daubert JC, Saint-Marc C, et al. Torsade depointes. Apropos of 54 cases [Article in French]. Ann Fr Anesth Reanim. 1982;1:513–20.
Salle P, Rey JL, Bernasconi P, et al. Torsades de pointe. Apropos of 60 cases. Ann Cardiol Angeiol (Paris). 1985;34:381–8.
Fung MC, Hsiao-hui Wu H, Kwong K, et al. Evaluation of the profile of patients with QTc prolongation in spontaneous adverse event reporting over the past three decades—1969–98. Pharmacoepidemiol Drug Saf. 2000;9(Suppl 1):S24.
Garnett CE, Beasley N, Bhattaram VA, et al. Concentration-QT relationships play a key role in the evaluation of proarrhythmic risk during regulatory review. J Clin Pharmacol. 2008;48:13–8.
Rock EP, Finkle J, Fingert HJ, et al. Assessing proarrhythmic potential of drugs when optimal studies are infeasible. Am Heart J. 2009;157:827–36.
Morganroth J, Shah RR, Scott JW. Evaluation and management of cardiac safety using the electrocardiogram in oncology clinical trials: focus on cardiac repolarization (QTc interval). Clin Pharmacol Ther. 2010;87:166–74.
Shah RR, Morganroth J. Early investigation of QTc liability: the role of multiple ascending dose (MAD) study. Drug Saf. 2012;35:695–709.
Piekarz RL, Frye AR, Wright JJ, et al. Cardiac studies in patients treated with depsipeptide, FK228, in a phase II trial for T-cell lymphoma. Clin Cancer Res. 2006;12:3762–73.
Varterasian M, Meyer M, Fingert H, et al. Baseline heart rate-corrected QT and eligibility for clinical trials in oncology. J Clin Oncol. 2003;21:3378–9.
Dong Q, Fu XX, Du LL, et al. Blocking of the human ether-à-go-go-related gene channel by imatinib mesylate. Biol Pharm Bull. 2013;36:268–75.
Dogan E, Yorgun H, Petekkaya I, et al. Evaluation of cardiac safety of lapatinib therapy for ErbB2-positive metastatic breast cancer: a single center experience. Med Oncol. 2012;29:3232–9.
Baselga J, Bradbury I, Eidtmann H, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379:633–40.
Kim TD, le Coutre P, Schwarz M, et al. Clinical cardiac safety profile of nilotinib. Haematologica. 2012;97:883–9.
AstraZeneca CAPRELSA REMS Program. http://www.caprelsarems.com/learn.aspx (Accessed Jan 20 2013).
Leboulleux S, Bastholt L, Krause T, et al. Vandetanib in locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 2 trial. Lancet Oncol. 2012;13:897–905.
Zang J, Wu S, Tang L, et al. Incidence and risk of QTc interval prolongation among cancer patients treated with vandetanib: a systematic review and meta-analysis. PLoS One. 2012;7:e30353.
Barros F, Gomez-Varela D, Viloria CG, et al. Modulation of human erg K+ channel gating by activation of a G protein-coupled receptor and protein kinase C. J Physiol. 1998;511(Pt 2):333–46.
Thomas D, Zhang W, Karle CA, et al. Deletion of protein kinase A phosphorylation sites in the HERG potassium channel inhibits activation shift by protein kinase A. J Biol Chem. 1999;274:27457–62.
Kiehn J, Karle C, Thomas D, et al. HERG potassium channel activation is shifted by phorbol esters via protein kinase A-dependent pathways. J Biol Chem. 1998;273:25285–91.
Davis MJ, Wu X, Nurkiewicz TR, et al. Regulation of ion channels by protein tyrosine phosphorylation. Am J Physiol Heart Circ Physiol. 2001;281:H1835–62.
Marx SO, Kurokawa J, Reiken S, et al. Requirement of a macromolecular signalling complex for beta adrenergic receptor modulation of the KCNQ1-KCNE1 potassium channel. Science. 2002;295:496–9.
Chen J, Sroubek J, Krishnan Y, et al. PKA phosphorylation of HERG protein regulates the rate of channel synthesis. Am J Physiol Heart Circ Physiol. 2009;296:H1244–54.
Sroubek J, McDonald TV. Protein kinase A activity at the endoplasmic reticulum surface is responsible for augmentation of human ether-a-go-go-related gene product (HERG). J Biol Chem. 2011;286:21927–36.
Krishnan Y, Li Y, Zheng R, et al. Mechanisms underlying the protein-kinase mediated regulation of the HERG potassium channel synthesis. Biochim Biophys Acta. 2012;1823:1273–84.
Zhang Y, Wang H, Wang J, et al. Normal function of HERG K+ channels expressed in HEK293 cells requires basal protein kinase B activity. FEBS Lett. 2003;534:125–32.
Zhang DY, Wang Y, Lau CP, et al. Both EGFR kinase and Src-related tyrosine kinases regulate human ether-à-go-go-related gene potassium channels. Cell Signal. 2008;20:1815–21.
Himmel HM, Hoffmann M. QTc shortening with a new investigational cancer drug: a brief case study. J Pharmacol Toxicol Methods. 2010;62:72–81.
Morgan TK Jr, Sullivan ME. An overview of class III electrophysiological agents: a new generation of antiarrhythmic therapy. Prog Med Chem. 1992;29:65–108.
Park BK, Kitteringham NR. Effects of fluorine substitution on drug metabolism: pharmacological and toxicological implications. Drug Metab Rev. 1994;26:605–43.
Park BK, Kitteringham NR, O’Neill PM. Metabolism of fluorine-containing drugs. Annu Rev Pharmacol Toxicol. 2001;41:443–70.
Elice F, Rodeghiero F, Falanga A, et al. Thrombosis associated with angiogenesis inhibitors. Best Pract Res Clin Haematol. 2009;22:115–28.
Girardi F, Franceschi E, Brandes AA. Cardiovascular safety of VEGF-targeting therapies: current evidence and handling strategies. Oncologist. 2010;15:683–94.
Minami M, Matsumoto S, Horiuchi H. Cardiovascular side-effects of modern cancer therapy. Circ J. 2010;74:1779–86.
Keefe D, Bowen J, Gibson R, et al. Noncardiac vascular toxicities of vascular endothelial growth factor inhibitors in advanced cancer: a review. Oncologist. 2011;16:432–44.
Mellor HR, Bell AR, Valentin JP, et al. Cardiotoxicity associated with targeting kinase pathways in cancer. Toxicol Sci. 2011;120:14–32.
Sonpavde G, Bellmunt J, Schutz F, et al. The double edged sword of bleeding and clotting from VEGF inhibition in renal cancer patients. Curr Oncol Rep. 2012;14:295–306.
Mir O, Ropert S, Alexandre J, et al. Hypertension as a surrogate marker for the activity of anti-VEGF agents. Ann Oncol. 2009;20:967–70.
Chu TF, Rupnick MA, Kerkela R, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet. 2007;370:2011–9.
Qi WX, Shen Z, Lin F, et al. Incidence and risk of hypertension with vandetanib in cancer patients: a systematic review and meta-analysis of clinical trials. Br J Clin Pharmacol. 2012;75:919–30.
Robinson ES, Khankin EV, Karumanchi SA, et al. Hypertension induced by vascular endothelial growth factor signalling pathway inhibition: mechanism and potential use as a biomarker. Semin Nephrol. 2010;30:591–601.
Maitland ML, Kasza KE, Karrison T, et al. Ambulatory monitoring detects sorafenib-induced blood pressure elevations on the first day of treatment. Clin Cancer Res. 2009;15:6250–7.
Veronese ML, Mosenkis A, Flaherty KT, et al. Mechanisms of hypertension associated with BAY 43-9006. J Clin Oncol. 2006;24:1363–9.
Kim JJ, Vaziri SA, Rini BI, et al. Association of VEGF and VEGFR2 single nucleotide polymorphisms with hypertension and clinical outcome in metastatic clear cell renal cell carcinoma patients treated with sunitinib. Cancer. 2012;118:1946–54.
Steeghs N, Gelderblom H, Roodt JO, et al. Hypertension and rarefaction during treatment with telatinib, a small molecule angiogenesis inhibitor. Clin Cancer Res. 2008;14:3470–6.
GlaxoSmilthKline Clinical Study Register A meta-analysis of the cumulative incidence of hypertension in the first month of treatment with pazopanib across three RCC studies: VEG102616, VEG105192 and VEG107769 (Study number 115227). http://www.gsk-clinicalstudyregister.com/result_detail.jsp?protocolId=115227&studyId=7FE7FADD-D3FA-4BD6-9BF5-0845FF2A2C90&compound=pazopanib&type=Compound&letterrange=L-P (Accessed Oct 25 2012).
Quintás-Cardama A, Kantarjian H, O’brien S, et al. Pleural effusion in patients with chronic myelogenous leukemia treated with dasatinib after imatinib failure. J Clin Oncol. 2007;25:3908–14.
Guignabert C, Montani D. Key roles of Src family tyrosine kinases in the integrity of the pulmonary vascular bed. Eur Respir J. 2013;41:3–4.
Pullamsetti SS, Berghausen EM, Dabral S, et al. Role of Src tyrosine kinases in experimental pulmonary hypertension. Arterioscler Thromb Vasc Biol. 2012;32:1354–65.
Schermuly RT, Dony E, Ghofrani HA, et al. Reversal of experimental pulmonary hypertension by PDGF inhibition. J Clin Invest. 2005;115:2811–21.
Ghofrani HA, Seeger W, Grimminger F. Imatinib for the treatment of pulmonary arterial hypertension. N Engl J Med. 2005;353:1412–3.
Tapper EB, Knowles D, Heffron T, et al. Portopulmonary hypertension: imatinib as a novel treatment and the Emory experience with this condition. Transplant Proc. 2009;41:1969–71.
ten Freyhaus H, Dumitrescu D, Bovenschulte H, et al. Significant improvement of right ventricular function by imatinib mesylate in scleroderma-associated pulmonary arterial hypertension. Clin Res Cardiol. 2009;98:265–7.
Chhina MK, Nargues W, Grant GM, et al. Evaluation of imatinib mesylate in the treatment of pulmonary arterial hypertension. Future Cardiol. 2010;6:19–35.
ten Freyhaus H, Dumitrescu D, Berghausen E, et al. Imatinib mesylate for the treatment of pulmonary arterial hypertension. Expert Opin Investig Drugs. 2012;21:119–34.
Antoniu SA. Targeting PDGF pathway in pulmonary arterial hypertension. Expert Opin Ther Targets. 2012;16:1055–63.
Ghofrani HA, Morrell NW, Hoeper MM, et al. Imatinib in pulmonary arterial hypertension patients with inadequate response to established therapy. Am J Respir Crit Care Med. 2010;182:1171–7.
Hatano M, Yao A, Shiga T, et al. Imatinib mesylate has the potential to exert its efficacy by down-regulating the plasma concentration of platelet-derived growth factor in patients with pulmonary arterial hypertension. Int Heart J. 2010;51:272–6.
Ciuclan L, Bonneau O, Hussey M, et al. A novel murine model of severe pulmonary arterial hypertension. Am J Respir Crit Care Med. 2011;184:1171–82.
Ciuclan L, Hussey MJ, Burton V, et al. Imatinib attenuates hypoxia-induced pulmonary arterial hypertension pathology via reduction in 5-hydroxytryptamine through inhibition of tryptophan hydroxylase 1 expression. Am J Respir Crit Care Med. 2013;187:78–89.
Kojonazarov B, Sydykov A, Pullamsetti SS, et al. Effects of multikinase inhibitors on pressure overload-induced right ventricular remodeling. Int J Cardiol. 2012 (Epub ahead of print).
Schmidinger M, Zielinski CC, Vogl UM, et al. Cardiac toxicity of sunitinib and sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2008;26:5204–12.
Kerkelä R, Grazette L, Yacobi R, et al. Cardiotoxicity of the cancer therapeutic agent imatinib mesylate. Nat Med. 2006;12:908–16.
Lenihan DJ, Cardinale D, Cipolla CM. The compelling need for a cardiology and oncology partnership and the birth of the International CardiOncology Society. Prog Cardiovasc Dis. 2010;53:88–93.
Cheng H, Force T. Why do kinase inhibitors cause cardiotoxicity and what can be done about it? Prog Cardiovasc Dis. 2010;53:114–20.
Dasanu CA, Padmanabhan P, Clark BA 3rd, et al. Cardiovascular toxicity associated with small molecule tyrosine kinase inhibitors currently in clinical use. Expert Opin Drug Saf. 2012;11:445–57.
Montaigne D, Hurt C, Neviere R. Mitochondria death/survival signalling pathways in cardiotoxicity induced by anthracyclines and anticancer-targeted therapies. Biochem Res Int. 2012;Article ID 951539.
Van den Akker NM, Winkel LC, Nisancioglu MH, et al. PDGF-B signalling is important for murine cardiac development: its role in developing atrioventricular valves, coronaries, and cardiac innervation. Dev Dyn. 2008;237:494–503.
Cheng H, Kari G, Dicker AP, et al. A novel preclinical strategy for identifying cardiotoxic kinase inhibitors and mechanisms of cardiotoxicity. Circ Res. 2011;109:1401–9.
Force T, Krause DS, Van Etten RA. Molecular mechanisms of cardiotoxicity of tyrosine kinase inhibitors. Nat Rev Cancer. 2007;7:332–44.
Kerkela R, Woulfe KC, Durand JB, et al. Sunitinib-induced cardiotoxicity is mediated by off-target inhibition of AMP-activated protein kinase. Clin Transl Sci. 2009;2:15–25.
Hasinoff BB. The cardiotoxicity and myocyte damage caused by small molecule anticancer tyrosine kinase inhibitors is correlated with lack of target specificity. Toxicol Appl Pharmacol. 2010;244:190–5.
Hasinoff BB, Patel D. Mechanisms of myocyte cytotoxicity induced by the multikinase inhibitor sorafenib. Cardiovasc Toxicol. 2010;10:1–8.
Hasinoff BB, Patel D. The lack of target specificity of small molecule anticancer kinase inhibitors is correlated with their ability to damage myocytes in vitro. Toxicol Appl Pharmacol. 2010;249:132–9.
Subbiah IM, Lenihan DJ, Tsimberidou AM. Cardiovascular toxicity profiles of vascular-disrupting agents. Oncologist. 2011;16:1120–30.
Force T, Kerkela R. Cardiotoxicity of the new cancer therapeutics- mechanisms of, and approaches to, the problem. Drug Discov Today. 2008;13:778–84.
Yang B, Papoian T. Tyrosine kinase inhibitor (TKI)-induced cardiotoxicity: approaches to narrow the gaps between preclinical safety evaluation and clinical outcome. J Appl Toxicol. 2012 (Epub ahead of print).
Eschenhagen T, Force T, Ewer MS, et al. Cardiovascular side effects of cancer therapies: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2011;13:1–10.
Steingart RM, Bakris GL, Chen HX, et al. Management of cardiac toxicity in patients receiving vascular endothelial growth factor signalling pathway inhibitors. Am Heart J. 2012;163:156–63.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this review and have not received any financial support for writing it. RRS was formerly a Senior Clinical Assessor at the Medicines and Healthcare products Regulatory Agency (MHRA), London, UK, and the ICH E14 Topic Leader, representing the EU. JM is the Chief Cardiac Consultant to eResearchTechnology Inc. (eRT), Philadelphia, PA, USA, which provides cardiac safety services to drug development companies. Both RRS and JM now provide expert consultancy services on QT liability of drugs and development of new drugs to a number of pharmaceutical companies. DRS is a first-year house officer at a district general hospital and has no consultancy relationships.
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed in this article are those of the authors and do not necessarily reflect the views or opinions of their affiliates, any regulatory authorities or any of their advisory bodies.
Rights and permissions
About this article
Cite this article
Shah, R.R., Morganroth, J. & Shah, D.R. Cardiovascular Safety of Tyrosine Kinase Inhibitors: With a Special Focus on Cardiac Repolarisation (QT Interval). Drug Saf 36, 295–316 (2013). https://doi.org/10.1007/s40264-013-0047-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0047-5