Abstract
Background
Prior studies have evaluated the use of various constituents of cannabis for their anti-seizure effects. Specifically, cannabidiol, a non-psychoactive component of cannabis, has been investigated for treatment-resistant epilepsy, but more information is needed particularly on its use in a pediatric population.
Objective
The objective of this study was to evaluate the pharmacokinetics and safety of a synthetic pharmaceutical-grade cannabidiol oral solution in pediatric patients with treatment-resistant epilepsy.
Methods
In this open-label study, pediatric patients (aged 1 to ≤ 17 years) with treatment-resistant epilepsy received cannabidiol oral solution administered as add-on to their current antiepileptic drug regimen. Patients received a single dose (5, 10, or 20 mg/kg) on day 1 and twice-daily dosing on days 4 through 10 (10-mg/kg [cohort 1], 20-mg/kg [cohort 2], or 40-mg/kg [cohort 3] total daily dose). Serial blood samples were collected on day 1 before dosing and up to 72 h post-dose, and on day 10 before dosing and up to 24 h post-dose. Blood samples to assess trough concentrations of cannabidiol were collected on day 6 (for patients aged 12 to ≤ 17 years), day 8 (for patients aged 2 to ≤ 17 years), and day 9 (for patients aged 6 to ≤ 17 years).
Results
Overall, 61 patients across three cohorts received one of three doses of cannabidiol oral solution (mean age, 7.6 years). The age composition was similar in the three cohorts. There was a trend for increased cannabidiol exposure with increased cannabidiol oral solution dosing, but overall exposure varied. Approximately 2–6 days of twice-daily dosing provided steady-state concentrations of cannabidiol. A bi-directional drug interaction occurred with cannabidiol and clobazam. Concomitant administration of clobazam with 40 mg/kg/day of cannabidiol oral solution resulted in a 2.5-fold increase in mean cannabidiol exposure. Mean plasma clobazam concentrations were 1.7- and 2.2-fold greater in patients receiving clobazam concomitantly with 40 mg/kg/day of cannabidiol oral solution compared with 10 mg/kg/day and 20 mg/kg/day. Mean plasma norclobazam values were 1.3- and 1.9-fold higher for patients taking clobazam plus 40 mg/kg/day of cannabidiol oral solution compared with the 10-mg/kg/day and 20-mg/kg/day groups. All doses were generally well tolerated, and common adverse events that occurred at > 10% were somnolence (21.3%), anemia (18.0%), and diarrhea (16.4%).
Conclusions
Inter-individual variability in systemic cannabidiol exposure after pediatric patient treatment with cannabidiol oral solution was observed but decreased with multiple doses. Short-term administration was generally safe and well tolerated.
Trial Registration
ClinicalTrials.gov (NCT02324673).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In the USA, the prevalence of epilepsy and seizure disorders in children has been estimated at 1% [1]. Currently, several non-pharmacologic interventions, such as resective surgery, dietary intervention (e.g., ketogenic diet), neurostimulation (e.g., vagus nerve stimulation or responsive neurostimulation), and pharmacologic therapies, are used to treat children with epilepsy [2, 3]. Despite the availability of several treatment options, a prospective observational study of 470 previously untreated children, adolescents, and adults with epilepsy showed that only 47% of patients had a response to initial monotherapy and only an additional 13% responded to a second monotherapy [4]. Of the 70 patients who received combination therapy, only 23% of patients who received two drugs were seizure free; further, no patients who received three drugs were free of seizures [4]. Therefore, there remains an unmet need for novel treatments.
Cannabidiol is a novel compound with central nervous system activity and, unlike other cannabinoids (e.g., tetrahydrocannabinol), produces no euphoria. Cannabidiol has a low affinity for the endogenous cannabinoid receptors and may modulate neuronal hyperexcitability through other mechanisms [5]. The possible mechanisms of anticonvulsive action include an anti-inflammatory effect on the nervous system, inverse agonism (or antagonism) at the cannabinoid receptors, modulation of neuronal channels, and enhancement of anandamide action [6,7,8,9,10,11]. Given these attributes, cannabidiol is being evaluated as a potential therapeutic option for several disorders, including seizures, chemotherapy-induced nausea and vomiting, spasticity, tics, post-traumatic stress disorder, and neuropathic pain, with seizures being, by far, the most frequently investigated condition [12, 13]. Indeed, previous studies have shown potential benefit of pure cannabidiol in decreasing the number of seizures in patients with treatment-resistant epilepsy associated with different forms of epilepsy, including Dravet syndrome and Lennox–Gastaut syndrome [14,15,16,17,18,19].
A highly purified plant-based form of oral cannabidiol formulation was approved by the US Food and Drug Administration in 2018 for the treatment of Dravet and Lennox–Gastaut syndromes in patients aged ≥ 2 years [20]. Two randomized, phase III clinical trials in children, adolescents, and adults with Lennox–Gastaut syndrome demonstrated that plant-based cannabidiol decreased the monthly frequency of seizures [17, 19]. A clinical trial on the safety and pharmacokinetic (PK) parameters of cannabidiol (5- to 20-mg/kg/day doses) for the treatment of seizures in 34 children (aged 4–10 years) with Dravet syndrome reported common adverse events (AEs) of pyrexia, somnolence, decreased appetite, sedation, vomiting, ataxia, and abnormal behavior in three or more patients at all doses tested [21]. Additional open-label studies have shown that cannabidiol was efficacious in decreasing median monthly seizure frequency in treatment-resistant epilepsies of multiple etiologies [18, 22].
Currently, there are still limited published data on the PK parameters and drug interactions related to cannabidiol use in the pediatric epilepsy population. The objective of this study was to characterize the PK parameters and short-term tolerability of pharmaceutical-grade synthetic cannabidiol oral solution in pediatric patients with treatment-resistant epilepsy. The current study is the first to examine the synthetic cannabidiol formulation in humans.
2 Methods
2.1 Patient Population
Individuals aged 1–17 years who weighed between ≥ 9 and ≤ 90 kg and had treatment-resistant epilepsy were eligible for inclusion. Epilepsy was considered “treatment resistant” if patients had recurrent seizures despite adequate trials of three or more antiepileptic drugs and one or more prior adequate treatment courses with two or more antiepileptic drugs in combination. Patients were required to have been on a stable-dose antiepileptic drug regimen for ≥ 30 days prior to day 0 and to remain on that regimen for the entire duration of the study. Vagus nerve stimulation and adherence to a ketogenic diet were not counted as part of the antiepileptic drug regimen in this trial. However, the settings for vagus nerve stimulator treatment had to remain stable during the study. Similarly, for individuals on a ketogenic diet, the fat-to-carbohydrate ratio and daily protein intake needed to remain stable during the study. Additional inclusion criteria were use of contraception by both male and female individuals of childbearing age, lack of pregnancy in female individuals, willingness to comply with study procedures, and general good health, as determined by the investigator. Patients were excluded if they had any clinically significant abnormality, suicidal ideation or history of attempted suicide, history of allergic reaction to study drug, or known infection with hepatitis B or C or human immunodeficiency virus. The initiation of felbamate < 6 months before the screening visit and the use of any cannabinoids (e.g., cannabidiol, hemp oil, marijuana) in the 30 days before screening were not permitted. Patients with electrocardiogram results that were considered clinically significant by the investigator at time of enrollment, or a history of such results, were excluded.
Because cannabidiol inhibits or is a substrate for some members of the cytochrome P450 (CYP) protein family, particularly CYP2C19, and others such as CYP3A4, CYP3A5, and CYP3A7 [11, 23, 24], patients who received CYP inhibitors, inducers, or sensitive substrates with a narrow therapeutic index (Electronic Supplementary Material) were excluded from participation, as were patients with any disorder or history of a condition (e.g., malabsorption) that could have interfered with drug absorption, distribution, metabolism, or excretion. Patients were asked to refrain from consuming grapefruit, Seville oranges, and products made from these fruits (e.g., grapefruit juice, Seville orange marmalade).
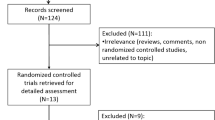
2.2 Study Design
This open-label, multiple-ascending dose, phase I/II study consisted of an up to 28-day screening phase, a 10-day treatment phase, and a 7-day follow-up period (Fig. 1). Patients who completed the study could be enrolled in an open-label extension study; data from that study will be published in a follow-on manuscript. Patients were randomly assigned to one of three cohorts: cannabidiol oral solution of 10 mg/kg/day (80 mg/mL; cohort 1), 20 mg/kg/day (300 mg/mL; cohort 2), or 40 mg/kg/day (300 mg/mL; cohort 3). These total daily doses were selected based on the tolerability and safety profiles reported for various cannabidiol product concentrations [25] and the anticipated body weight range of participants. The active ingredient in the cannabidiol oral solution is a synthetic pharmaceutical-grade cannabidiol produced by INSYS Manufacturing LLC (Chandler, AZ, USA), according to Current Good Manufacturing Practice. The three dosing cohorts were evaluated sequentially, starting with the 10-mg/kg cohort. Enrollment of approximately 20 patients per cohort was targeted, with each cohort consisting of five infants (aged 1 to < 2 years), nine children (aged 2 to < 12 years), and six adolescents (aged 12 to ≤ 17 years). Based on compatibility testing conducted by the sponsor, patients were allowed to receive cannabidiol oral solution via a gastronomy tube, if needed.
Study design. After screening period, patients were randomly assigned to three dosing cohorts of cannabidiol oral solution (cohort 1:10 mg/kg/day; cohort 2: 20 mg/kg/day; and cohort 3: 40 mg/kg/day). Patients received a single dose (5 mg/kg, 10 mg/kg, or 20 mg/kg, respectively) on day 1, and no drug was given on days 2 and 3. Patients received 5 mg/kg, 10 mg/kg, or 20 mg/kg twice daily (10 mg/kg/day, 20 mg/kg/day or 40 mg/kg/day, respectively) from day 4 to day 10
On day 1, patients received a single dose (morning; 5, 10, or 20 mg/kg) followed by a preset volume of water or clear liquid; no doses were received on days 2 and 3, and then multiple doses (morning and evening dose) were received on days 4 through 10 (10-, 20-, or 40-mg/kg total daily dose split into two daily doses; Fig. 1). The parent(s) or caregiver(s) of each eligible patient were offered the opportunity for all visits to be completed in an inpatient setting if they preferred. Otherwise, the following inpatient schedule was used: patients were admitted as inpatients on the final screening day (day 0) and remained in the medical facility at least until they received the morning dose on day 8. Patients were readmitted as inpatients on the morning of day 10 and released on the morning of day 11 (first day of the follow-up period) after completing the study assessments.
2.3 Study Assessments
Pharmacokinetic sampling schemes were adjusted based on age to avoid excessive blood loss. All blood samples were collected in 2-mL potassium ethylene diamine tetra acetic acid (K2-EDTA) plasma tubes for patients aged < 2 years and in 4-mL K2-EDTA plasma tubes for patients aged ≥ 2 years. For the PK analysis of cannabidiol and its primary metabolite 7-hydroxy-cannabidiol (7-OH cannabidiol) concentrations, serial blood samples were collected on day 1 pre-dose (for patients aged 2 to < 6 years and patients aged 6 to ≤ 17 years) and at 2, 4, 8, and 12 h post-dose (for all patients; Table 1). Additional samples were obtained at 1, 3, 16, 24 (day 2), and 48 h (day 3) after initial dosing on day 1 in patients aged 2 to < 6 years and patients aged 6 to ≤ 17 years. Samples were also taken at 6, 36, and 72 h (before the scheduled morning cannabidiol dose on day 4) after initial dosing on day 1 in patients aged 6 to ≤ 17 years. On day 10 (multiple dose), plasma was collected pre-dose and at 2, 4, 8, and 12 h (before administration of the second daily dose) post-dose in all patients. On day 10, additional samples were collected at 6 h (age 6 to ≤ 17 years only), and 1, 3, and 24 h post-dose in patients aged ≥ 2 years (Table 1). In addition, samples for trough cannabidiol and 7-OH cannabidiol concentrations were evaluated on day 6 (for patients aged 12 to ≤ 17 years), day 8 (for patients aged 2 to ≤ 17 years), and day 9 (for patients aged 6 to ≤ 17 years) prior to the morning dose.
On plasma collection days, with the exception of preset volumes of water or clear liquid to be consumed immediately after drug administration, patients were not to have liquid or solid food for 1 h (age < 2 years) or 2 h (age ≥ 2 years) before and after drug administration.
Cannabidiol has been shown to impact the metabolism of clobazam in pediatric patients, resulting in elevated plasma concentrations of norclobazam, an active metabolite of clobazam [21, 26]. Therefore, plasma concentrations of clobazam and norclobazam were determined on days 1, 8, and 10 before dosing in patients aged ≥ 2 years who were receiving clobazam as part of their established antiepileptic drug regimen treatment.
Plasma concentrations of cannabidiol and 7-OH cannabidiol were determined using an API 5000™ liquid chromatography-mass spectrometry system (AB Sciex, Concord, ON, Canada) equipped with a high-performance liquid chromatography column. The procedure has been validated to detect cannabidiol and 7-OH cannabidiol concentrations ranging from 0.100 to 50.0 ng/mL, based on the analysis of 0.2 mL of plasma. Clobazam and norclobazam concentrations were analyzed with a validated assessment range from 1.00 to 500 ng/mL, based on the analysis of 0.1 mL of plasma. For both cannabidiol and clobazam, the quantitation was performed using a weighted 1/x2 linear least-squares regression analysis generated from calibration standards. Quality control samples from high, medium, and low pools were processed with each sample run; the sample run was validated when at least two-thirds of the qualifying quality control samples were within 15% of their theoretical values and ≥ 50% of quality control samples at each level met this criterion.
Safety assessments, including monitoring of treatment-emergent AEs and vital signs, were conducted throughout the study. Electrocardiogram measurements were obtained at screening and on days 1, 4, 8, and 11 before treatment administration. Clinical serum chemistry assessments included alanine aminotransferase, albumin, alkaline phosphatase, aspartate aminotransferase, bicarbonate, bilirubin (total and direct), blood urea nitrogen, calcium, chloride, creatinine, follicle-stimulating hormone, glucose, phosphorus, potassium, protein (total), sodium, and uric acid concentrations.
2.4 Data Analyses
The PK population included all patients who received at least one dose of the study medication and had at least one post-dose cannabidiol and/or 7-OH cannabidiol plasma concentration measurement. The safety population included all patients who received at least one dose of the study medication. Pharmacokinetic analyses were performed using Phoenix® WinNonlin® Version 6.4 (Certara L.P., Princeton, NJ, USA) or SAS® Version 9.4 or higher (SAS Institute, Inc., Cary, NC, USA). A non-compartmental method was used to derive all PK parameters. Pharmacokinetic data were summarized by study day and scheduled time and stratified by dose using descriptive statistics (sample size [n], mean, standard deviation, coefficient of variation, median, minimum, maximum, and geometric mean and geometric coefficient of variation [as appropriate for PK parameters]). All observed data were analyzed; missing values were not imputed.
3 Results
Of the 84 patients screened, 61 patients (72.6%) were enrolled and randomly assigned to receive cannabidiol oral solution (cohort 1 [10 mg/kg/day], n = 20; cohort 2 [20 mg/kg/day], n = 20, and cohort 3 [40 mg/kg/day], n = 21). Background antiepileptic drugs and concomitant medications were the most common eligibility-related reasons for screen failure. All 61 patients were included in the PK and safety populations and completed the study. The age group composition of all cohorts was similar (infants, n = 5 [all cohorts]; children, n = 9 [cohorts 1 and 2] or n = 10 [cohort 3]; and adolescents, n = 6 [all cohorts]) as was mean age (7.5–7.8 years; Table 2) and mean weight (24.3–29.7 kg; Table 2).
3.1 Pharmacokinetics
3.1.1 Cannabidiol
Single-dose administration of cannabidiol oral solution showed inter-individual variability with differences in systemic exposure between cohorts (Table 3). The median time to the maximum plasma concentration of cannabidiol after a single dose for all cohorts ranged from 2 to 4 h post-dose, indicating slow absorption of cannabidiol oral solution with a broad absorption phase when given without food. No dose-related differences in geometric mean terminal half-life were observed after a single dose.
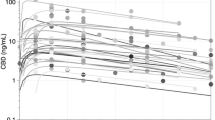
After the administration of multiple doses of cannabidiol (day 10), there was a trend toward increased exposure, defined as area under the concentration–time curve in plasma during the dosing interval (AUC(0–τ)), that was associated with increased cannabidiol oral solution dosing across cohorts (Fig. 2). After approximately 2–6 days of twice-daily dosing, apparent steady-state concentrations of cannabidiol were achieved. The median time to the maximum plasma concentration ranged between 2 and 3 h and was independent of dose. Maximum plasma concentration (Cmax) and total cannabidiol exposure (AUC(0–τ)) increased proportionally with dose, such that an approximate four-fold increase was observed over the 10- to 40-mg/kg/day dose range. Apparent clearance was dose independent (Table 3). An accumulation of cannabidiol was observed after up to 7 days of twice-daily dosing. Accumulation was 1.1- to 11.8-fold based on Cmax and 1.8- to 16.5-fold across all doses, based on the area under the concentration–time curve.
Mean plasma cannabidiol concentration–time profile on multiple-dose on day 10 in a infants, b childrena, and c adolescents. Data shown are geometric means; error bars represent standard deviations. aFor cohort 2 (20 mg/kg/day), two children missed one or more doses between the evening of day 8 and assessment at day 9 and were not included in the analysis for this cohort
3.1.2 7-OH Cannabidiol
Pharmacokinetic results of the primary metabolite, 7-OH cannabidiol, generally reflected those observed for cannabidiol (Table 4; ESM). The geometric mean molar ratios of 7-OH cannabidiol/cannabidiol exposures across age strata ranged from 0.38 to 1.07 for Cmax on day 1 and from 0.49 to 0.85 for Cmax on day 10, and from 0.54 to 1.36 for total exposure (AUC(0–∞) and AUC(0–12)) on day 1 and from 0.65 to 0.98 for total exposure (AUC(0–12)) on day 10. The ratio of 7-OH cannabidiol to the parent compound (cannabidiol) was not affected by cannabidiol dose or patient age. The geometric mean of the terminal half-life of 7-OH cannabidiol was similar to or shorter than that of cannabidiol (Table 4).
3.1.3 Age Assessment
The mean (SD) plasma cannabidiol concentration-time profiles following multiple-dose administrations of cannabidiol oral solution (cohort 1 [10 mg/kg/day], cohort 2 [20 mg/kg/day], and cohort 3 [40 mg/kg/day]) by age categories are shown in Fig. 3a-c. Statistical comparisons for age effects on cannabidiol exposure after multiple doses are presented in Table 5. The point estimates for infants vs. children or for infants vs. adolescents for Cmax and AUC(0–τ) ranged from 38.7 to 46.8%. There were no major differences between children and adolescents. At the lower dose levels (20 mg/kg/day or 10 mg/kg/day), exposure in infants was also lower than in adolescents; there were no consistent trends for children. The 90% confidence intervals contained 100% for most of the age category comparisons at the lower dose levels.
3.1.4 Influence of Clobazam Use
Approximately half of the patients (52.5%) in the study received concomitant clobazam. In patients receiving clobazam plus cannabidiol oral solution at a dose of 40 mg/kg/day, mean cannabidiol exposure on day 10 increased approximately 2.5-fold compared with patients not receiving clobazam (geometric mean AUC(0–τ), 3130 ng·h/mL vs. 1245 ng·h/mL, respectively; Table 6), indicating a drug–drug interaction with clobazam. The Cmax of cannabidiol was approximately 2.4-fold higher in patients receiving clobazam compared with patients not receiving clobazam. Similarly, a trend for increased 7-OH cannabidiol concentrations with clobazam administration was seen with an approximately 3.06-fold higher Cmax and a 3.14-fold higher AUC(0–τ) in patients receiving clobazam compared with patients not receiving clobazam. On day 10, mean plasma clobazam concentrations were increased 1.7- and 2.2-fold in patients receiving clobazam concomitantly with cannabidiol oral solution of 40 mg/kg/day compared with 10 mg/kg/day and 20 mg/kg/day (857 ng/mL vs. 500 ng/mL and 390 ng/mL), respectively. Similarly, mean plasma norclobazam concentrations on day 10 were increased 1.3- and 1.9-fold in patients receiving clobazam concomitantly with cannabidiol oral solution of 40 mg/kg/day compared with 10 mg/kg/day and 20 mg/kg/day (6111 ng/mL vs. 4750 ng/mL and 3224 ng/mL), respectively. Additionally, cannabidiol appeared to increase clobazam and norclobazam concentrations in a dose-dependent manner, and mean clobazam and norclobazam concentrations were increased up to 2.8-fold on day 10 (pre-dose) compared with day 1 (baseline, prior to administration of cannabidiol).
3.2 Safety
All doses of cannabidiol oral solution were generally well tolerated. Overall, the most common AEs included somnolence (21.3%), anemia (18.0%), and diarrhea (16.4%; Table 7), and most AEs were mild (26.2%) or moderate (13.1%). The incidence of diarrhea, increased weight, somnolence, and psychomotor hyperactivity increased as the dose of cannabidiol oral solution increased. Of the 13 patients who reported somnolence, seven (53.8%) were receiving the highest dose of cannabidiol oral solution (40 mg/kg/day) and concomitant clobazam. An increase in alanine aminotransferase was reported in a 16-year-old male individual receiving cannabidiol oral solution of 40 mg/kg/day; the patient had a slightly elevated alanine aminotransferase level (normal range: 5–30 U/L) at screening (43 U/L), which increased to 102 U/L on day 8 and decreased to 68 U/L by day 11. The reported AE of “alanine aminotransferase increased” was of moderate severity and its relationship to the study drug was considered to be “probable”. The AE resolved without any action, and the patient completed the study without any interruption in dose administration.
Three serious treatment-emergent AEs were reported (thrombophlebitis, apnea, and skin rash). Thrombophlebitis and apnea were considered by the investigator to be unrelated to the study drug; the skin rash was considered probably related to the study drug. The skin rash was reported by a 16-year-old male individual receiving 40 mg/kg/day of cannabidiol oral solution; the event occurred after the last scheduled dose (day 10), resulted in study discontinuation, and resolved with routine medical management. The serious AE of thrombophlebitis at the insertion site of a central catheter was reported in an 8-year-old female individual receiving 20 mg/kg/day of cannabidiol oral solution. The event of thrombophlebitis resulted in temporary discontinuation of study medication and resolved after enoxaparin therapy. The serious AE of apnea was reported in a 14-month-old male individual receiving 40 mg/kg/day of cannabidiol on day 10. This apneic episode was short (< 1 min) and resolved with oxygen administration from a nasal cannula with no additional apnea episodes. No deaths were reported. No notable mean changes from baseline were observed in other clinical chemistry laboratory assessments, vital signs, or electrocardiogram readings.
4 Discussion
Previous studies have shown that cannabidiol is effective in controlling the frequency of seizures due to epilepsy of multiple etiologies in children and adults [17,18,19, 21, 22]. To our knowledge, this is the first study of a synthetic cannabidiol formulation in humans and provides PK data in a pediatric population. We used a formulation that is 99.5% pure without the impurities, such as tetrahydrocannabinol and other cannabis molecules, which may be present in a non–US Food and Drug Administration-approved plant-based formulation. Additionally, synthetic cannabidiol used in the study has high chiral purity compared with plant material. It has been reported that the (+)-CBD isomer (synthetic) was more active than the (−)-CBD isomer (natural) in binding to CBD receptor CB1 and CB2.
In our study, patients received the study drug under fasting conditions. However, food has been reported to significantly increase cannabidiol exposure [27]. The food effect on cannabidiol absorption and the drug–drug interactions with other antiepileptic medications will need to be taken into account [5].
In this open-label, multiple ascending dose study of a pharmaceutical-grade synthetic cannabidiol oral solution in pediatric patients with treatment-resistant epilepsy, inter-individual variability in systemic exposure to cannabidiol was observed and 7-OH cannabidiol exhibited formation rate-limited PK parameters. Steady-state cannabidiol exposures occurred after approximately 2–6 days of treatment and appeared to increase in a dose-dependent manner. The total variability in cannabidiol exposures was higher after a single-dose administration on day 1 but decreased as patients received additional treatment doses (i.e., day 10). Increased exposures may partly represent the accumulation of cannabidiol over time. The doses of cannabidiol (10 mg/kg/day, 20 mg/kg/day, and 40 mg/kg/day) tested in this study are similar to doses used in other clinical trials of plant-based cannabidiol formulations in pediatric populations and adults [17, 18, 21].
Co-administration of clobazam was associated with increased cannabidiol exposure (2.5-fold increase in patients receiving clobazam compared with those not receiving clobazam) in the high-dose group (40 mg/kg/day). In addition, mean plasma clobazam and norclobazam concentrations were increased in patients receiving 40 mg/kg/day of cannabidiol oral solution compared with 10 and 20 mg/kg/day of cannabidiol oral solution. The bi-directional interaction between these two compounds could be because both are substrates for CYP3A4 even though other influencing factors such as other concomitant drugs, gender, and age may not be ruled out. In this study, the sample size for each age group per cohort was too small for additional analysis. Therefore, close serum concentration monitoring for both medications along with clinical monitoring may be needed in pediatric patients receiving clobazam concomitantly with cannabidiol.
Overall, synthetic cannabidiol oral solution was considered safe at all doses examined and generally well tolerated in this pediatric population. When compared with previous reports on plant-derived pharmaceutical formulations, the AEs reported in this study were generally similar [14, 28]. The incidence of some AEs (diarrhea, flatulence, somnolence, and psychomotor hyperactivity) appeared to be dose related, with higher cannabidiol oral solution doses eliciting more AEs. The event of somnolence occurred most often in patients taking concomitant clobazam, as previously reported with a plant-derived cannabidiol formulation in pediatric patients [14, 15, 26, 28].
This PK study of synthetic cannabidiol oral solution included different age groups (infants, children, and adolescents) and ascending doses, and evaluated PK parameters over an extended time period (up to 4 days after a single dose and 7 days after multiple doses). However, this study is limited by the small sample size per age group (n = 5–10), short treatment duration (10 days), sampling in patients aged 1 to < 2 years that was sparser than that for patients aged 2 to ≤ 17 years, high variability in cannabidiol exposure, drug–drug interaction between cannabidiol and clobazam, and differences in the distribution of concomitant drugs across age groups and cohorts. Furthermore, patients were receiving additional concomitant antiepileptic medications, which may have influenced the PK and safety profiles. Another limitation of this study is that plasma concentrations of concomitant antiepileptic drugs were not measured.
5 Conclusion
Steady-state cannabidiol exposures after administration of pharmaceutical-grade synthetic cannabidiol oral solution appeared to increase in a dose-dependent manner. Cannabidiol exposure varied among patients. Cannabidiol oral solution was generally safe at all doses studied and well tolerated in this pediatric population. Future studies are warranted to evaluate dose titration for efficacy and to assess the long-term safety profile of cannabidiol oral solution.
References
Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129(2):256–64.
Ostendorf AP, Ng YT. Treatment-resistant Lennox–Gastaut syndrome: therapeutic trends, challenges and future directions. Neuropsychiatr Dis Treat. 2017;13:1131–40.
Glauser T, Ben-Menachem E, Bourgeois B, et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54(3):551–63.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342(5):314–9.
Campbell CT, Phillips MS, Manasco K. Cannabinoids in pediatrics. J Pediatr Pharmacol Ther. 2017;22(3):176–85.
Vilela LR, Lima IV, Kunsch EB, et al. Anticonvulsant effect of cannabidiol in the pentylenetetrazole model: pharmacological mechanisms, electroencephalographic profile, and brain cytokine levels. Epilepsy Behav. 2017;75:29–35.
Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. 2007;150(5):613–23.
Ross HR, Napier I, Connor M. Inhibition of recombinant human T-type calcium channels by delta9-tetrahydrocannabinol and cannabidiol. J Biol Chem. 2008;283(23):16124–34.
Ghovanloo MR, Shuart NG, Mezeyova J, Dean RA, Ruben PC, Goodchild SJ. Inhibitory effects of cannabidiol on voltage-dependent sodium currents. J Biol Chem. 2018;293(43):16546–58.
Bisogno T, Hanus L, De Petrocellis L, et al. Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol. 2001;134(4):845–52.
Gaston TE, Szaflarski JP. Cannabis for the treatment of epilepsy: an update. Curr Neurol Neurosci Rep. 2018;18(11):73.
Devinsky O, Cilio MR, Cross H, et al. Cannabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia. 2014;55(6):791–802.
Wong SS, Wilens TE. Medical cannabinoids in children and adolescents: a systematic review. Pediatrics. 2017;140(5):1–18.
Devinsky O, Marsh E, Friedman D, et al. Cannabidiol in patients with treatment-resistant epilepsy: an open-label interventional trial. Lancet Neurol. 2016;15(3):270–8.
Devinsky O, Cross JH, Laux L, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. 2017;376(21):2011–20.
Tzadok M, Uliel-Siboni S, Linder I, et al. CBD-enriched medical cannabis for intractable pediatric epilepsy: the current Israeli experience. Seizure. 2016;35:41–4.
Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the Lennox–Gastaut syndrome. N Engl J Med. 2018;378(20):1888–97.
Devinsky O, Verducci C, Thiele EA, et al. Open-label use of highly purified CBD (Epidiolex®) in patients with CDKL5 deficiency disorder and Aicardi, Dup15q, and Doose syndromes. Epilepsy Behav. 2018;86:131–7.
Thiele EA, Marsh ED, French JA, et al. Cannabidiol in patients with seizures associated with Lennox–Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391(10125):1085–96.
US Food and Drug Administration. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. 2018. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm611046.htm. Accessed 2 Jan 2018.
Devinsky O, Patel AD, Thiele EA, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90(14):e1204–11.
Szaflarski JP, Bebin EM, Comi AM, et al. Long-term safety and treatment effects of cannabidiol in children and adults with treatment-resistant epilepsies: expanded access program results. Epilepsia. 2018;59(8):1540–8.
Yamaori S, Ebisawa J, Okushima Y, Yamamoto I, Watanabe K. Potent inhibition of human cytochrome P450 3A isoforms by cannabidiol: role of phenolic hydroxyl groups in the resorcinol moiety. Life Sci. 2011;88(15–16):730–6.
Jiang R, Yamaori S, Okamoto Y, Yamamoto I, Watanabe K. Cannabidiol is a potent inhibitor of the catalytic activity of cytochrome P450 2C19. Drug Metab Pharmacokinet. 2013;28(4):332–8.
Bergamaschi MM, Queiroz RH, Zuardi AW, Crippa JA. Safety and side effects of cannabidiol, a Cannabis sativa constituent. Curr Drug Saf. 2011;6(4):237–49.
Geffrey AL, Pollack SF, Bruno PL, Thiele EA. Drug–drug interaction between clobazam and cannabidiol in children with refractory epilepsy. Epilepsia. 2015;56(8):1246–51.
Taylor L, Gidal B, Blakey G, Tayo B, Morrison G. A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs. 2018;32(11):1053–67.
Sands TT, Rahdari S, Oldham MS, Caminha Nunes E, Tilton N, Cilio MR. Long-term safety, tolerability, and efficacy of cannabidiol in children with refractory epilepsy: results from an expanded access program in the US. CNS Drugs. 2018;33(1):47–60.
Acknowledgements
Technical editorial and medical writing assistance was provided by Mary Beth Moncrief, Ph.D., and Jill Gee, Ph.D., Synchrony Medical Communications, LLC, West Chester, PA, USA. INS011-14-029 Study Investigators: Maria Roberta Cilio, Dennis Dlugos, Michael Kohrman, Ian Miller, Steven Phillips, Roshan Raja, J. Ben Renfroe, Colin M. Roberts, Steven P. Sparagana, and James W. Wheless. Data were presented in part at the 2017 Annual Meeting of the American Epilepsy Society, December 1–5, 2017, Washington, DC, USA.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical Approval
The study protocol and amendments were approved by an institutional review board/ethics committee at each participating study center.
Informed Consent
All patients and/or parent(s)/caregiver(s) provided written informed consent and assent (as applicable) at enrollment.
Funding
This study was supported by INSYS Development Company, Inc. Support for technical editorial and medical writing assistance was provided by INSYS Development Company, Inc. Support for Open Access for this publication was provided by INSYS Development Company, Inc.
Conflict of interest
James W. Wheless reports that his institution received research funding from Acadia Pharmaceuticals Inc., GW Pharmaceuticals, plc., INSYS Development Company, Inc., LivaNova, Mallinckrodt, National Institutes of Health, Neurelis, Inc., NeuroPace, Inc., Shainberg Foundation, Upsher-Smith Laboratories, LLC, and Zogenix, Inc.; and has been a consultant and/or on speaker’s bureaus for CombiMatrix, Eisai Co., Ltd., GW Pharmaceuticals, plc., LivaNova, Lundbeck, Mallinckrodt, NeuroPace, Sun Pharmaceutical Industries, Ltd., Supernus Pharmaceuticals, Inc., and Upsher-Smith Laboratories, LLC. Dennis Dlugos reports that he received salary support from the National Institutes of Health, the Commonwealth of Pennsylvania Department of Health, and the Epilepsy Study Consortium, and he also received research program support for pre-study protocol development agreements with Bio-Pharm Solutions Inc., INSYS Development Company, Inc., and UCB, Inc. His institution received research support for clinical trials from INSYS Development Company, Inc. Ian Miller received honoraria and travel support from INSYS Development Company, Inc. and reports that his institution received study funding from INSYS Development Company, Inc. D. Alexander Oh was an employee of INSYS Development Company, Inc. and owns stock options for INSYS Development Company, Inc. Neha Parikh is an employee of INSYS Development Company, Inc. and owns stock options for INSYS Development Company, Inc. Steven Phillips reports that his institution received study funding from INSYS Development Company, Inc. J. Ben Renfroe reports that his institution received study funding from INSYS Development Company, Inc. Colin M. Roberts reports that his institution received study funding from INSYS Development Company, Inc. Isra Saeed reports that her institution received funding from INSYS Development Company, Inc. Steven P. Sparagana reports that his institution received study funding from INSYS Development Company, Inc. Jin Yu is an employee of INSYS Development Company, Inc. and owns stock options for INSYS Development Company, Inc. Maria Roberta Cilio reports that her institution received research support for clinical trials from INSYS Development Company, Inc; she also has been a consultant for BioMarin Pharmaceutical Inc., GW Pharmaceuticals plc., and Xenon Pharmaceuticals; and she received administrative support paid to her institution and drugs free of charge from GW Pharmaceuticals for previous studies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Below is the link to the electronic supplementary material.
Below is the link to the electronic supplementary material.
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wheless, J.W., Dlugos, D., Miller, I. et al. Pharmacokinetics and Tolerability of Multiple Doses of Pharmaceutical-Grade Synthetic Cannabidiol in Pediatric Patients with Treatment-Resistant Epilepsy. CNS Drugs 33, 593–604 (2019). https://doi.org/10.1007/s40263-019-00624-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-019-00624-4