Abstract
Background and Objective
A topical formulation of diclofenac (FLECTOR diclofenac epolamine topical system (FDETS)) is approved in adults for the treatment of acute pain due to minor strains, sprains, and contusions; however, its safety and efficacy have not been investigated in a pediatric population. This study assessed the safety and efficacy of the FLECTOR (diclofenac epolamine) topical system in children.
Methods
This was an open-label, single-arm, phase IV study at ten USA-based family medicine or pediatric practices in children aged 6–16 years with a clinically significant minor soft tissue injury sustained within the preceding 96 h and at least moderate spontaneous pain on the Wong-Baker FACES® Pain Rating Scale. The FLECTOR topical system was applied twice daily until pain resolution or Day 14. The primary endpoint was local tolerability and systemic safety. Key secondary endpoints were diclofenac plasma concentrations and analgesic efficacy.
Results
104 patients were enrolled; 52 were 6–11 years old, and 52 were 12–16 years old (mean age 11.6 years). The maximum tolerability score experienced by any patient was 1 (faint redness). Fourteen adverse events (none serious) in nine patients (8.7%) were considered possibly treatment-related. Reduction in pain during the study was somewhat greater for patients aged 6–11 versus 12–16 years (p < 0.011). The diclofenac plasma concentration tended to be higher in the younger age group compared with older patients: 1.83 versus 1.46 ng/mL at the first assessment and 2.49 versus 1.11 ng/mL at the last assessment (p = 0.002).
Conclusion
The FLECTOR topical system safely and effectively provided pain relief for minor soft tissue injuries in the pediatric population, with minimal systemic nonsteroidal anti-inflammatory drug exposure and low potential risk of local or systemic adverse events.
Clinical Trial Registration
ClinicalTrials.gov identifier NCT02132247.
Plain Language Summary
In this post-marketing clinical trial, the safety and efficacy at relieving pain of the FLECTOR diclofenac epolamine topical system (FDETS), a nonsteroidal anti-inflammatory drug (NSAID) formulation in a medicated patch, was assessed in a pediatric population (aged 6–16 years) with clinically significant minor soft tissue injuries. The safety and efficacy profiles in the pediatric population were consistent with previous data in adults. Both diclofenac plasma concentrations and reduction in pain during the study were greater for younger patients (aged 6–11 vs. 12–16 years), but plasma concentrations were much less than after diclofenac was taken orally in previous studies. This study shows that FDETS can safely and effectively provide pain relief for soft tissue injuries in children, with minimal systemic NSAID exposure and a low potential risk of either local or systemic adverse events.
Similar content being viewed by others
1 Introduction
Topical non-steroidal anti-inflammatory drugs (NSAIDs) are effective in a variety of acute and chronic pain conditions, including osteoarthritis [1,2,3,4,5], and systematic reviews of randomized, double-blind, comparative studies have shown topical diclofenac to be effective for acute and chronic pain, including strains and sprains, with low rates of systemic or local adverse events (AEs) [6, 7]. The use of topical systems (formerly known as patches) for the administration of NSAIDs has several key advantages, including drug delivery directly to the injury site, markedly reduced plasma concentrations relative to systemic formulations, lower risk of systemic AEs, and avoidance of first-pass metabolism and potential drug-drug interactions [1,2,3, 8, 9]. Furthermore, topical systems provide a route of administration for patients who are unable to take oral medication [9], and, of the various topical preparations of diclofenac, diclofenac patches are associated with lower rates of application site AEs than when formulated as gels or topical solutions [7]. Diclofenac as an epolamine salt is available as the topical formulation, FLECTOR diclofenac epolamine topical system (FDETS). The FDETS consists of an adhesive material containing 1.3% (180 mg) of active ingredient (diclofenac epolamine) to be directly applied to the painful area up to twice a day [10]. Each 10 × 14 cm FDETS releases diclofenac epolamine from a non-woven polyester felt backing. The adhesive side of FDETS is covered by a polypropylene film-release liner, which is removed before application.
FDETS is indicated for the treatment of acute pain due to minor strains, sprains and contusions [10]. Studies in adults with minor soft tissue injuries—including sports injuries and back pain—treated with FDETS have shown rapid and effective pain relief, with a low frequency of AEs [11,12,13,14,15,16]. Post hoc analysis of data from two double-blind, randomized, placebo-controlled studies (n = 274) in adult patients with acute ankle sprain showed that the diclofenac epolamine 1.3% topical patch resulted in clinically important pain reduction within approximately 3–4 h (p < 0.05 vs. placebo), with pain relief occurring as early as 1.27 h after application, compared with 3.76 h for the placebo patch [14]. Furthermore, a review of previously unpublished clinical and pharmacokinetic data supported the efficacy of FDETS in providing relevant clinical pain relief through local accumulation of diclofenac in the target site, without evidence of systemic effects [17]. More specifically, in a pediatric population, no topical or systemic AEs were reported when retrospective data from 176 children and adolescents aged 8–15 years with acute sports-related trauma injuries not severe enough to warrant surgical intervention or immobilization treated with FDETS one plaster twice daily for 3–14 (commonly 7) days [15].
While FDETS is approved for use in adults, the US Food and Drug Administration (FDA) requires a phase IV trial to be conducted to confirm the safety and efficacy of FDETS in a pediatric population. The present study assessed the safety and analgesic efficacy of FDETS in pediatric patients with clinically significant minor soft tissue injuries in USA-based practices compared with data from a previous study in adults.
2 Methods
This was an open-label, single-arm, phase IV non-randomized study conducted at ten family medicine or pediatric practices in the USA between May 2014 and October 2016. The study protocol was reviewed and approved by the FDA Division of Anesthesia, Analgesia, and Addiction Products (DAAAP) as adequate to assess the safety and efficacy of the FDETS for the treatment of minor soft tissue injuries in pediatric patients aged 6 through 16 years of age. A central institutional review board approved the protocol at each participating site, and the study was conducted according to the ethical principles of human research established by the Declaration of Helsinki and its amendments. At Visit 1, prior to enrolment, all children and their parent or legally authorized representative were given a verbal description of the study and required to read a Patient Information Sheet describing the intended research, including procedures, visit schedule, storage of investigational product, and diary completion instructions. Informed consent was required for all participants and/or their legal guardians. Two different consent documents were prepared: a Parental Permission Form, to be completed for all children by their parent/legally authorized representative, and a Children’s Assent Form, for completion by children 10–16 years of age. All participants and their legal guardians were given a copy of the applicable consent documents.
There was one protocol amendment that increased the eligibility interval from < 48 to < 96 h after injury occurrence to increase the likelihood of enrolling children with an acute injury.
2.1 Patients
The study included children aged 6–16 years with a clinically significant minor soft tissue injury sustained within the preceding 96 h, and spontaneous pain of at least moderate severity, defined as a score of ≥ 3 on the 6-point Wong-Baker FACES® Pain Rating Scale [18]. Post-menarche girls were required to have a negative pregnancy test.
Patients were excluded if their injury was midline or major, involved the spine, digits, or hands, or if they had open skin lesions within the injured area. In accordance with the Warnings and Precautions of the package insert, patients with severe cardiac, renal, or hepatic impairment were excluded from the study. Other exclusion criteria included the use of a long-acting NSAID since sustaining the injury, or topical medication within the past 48 h. A complete list of inclusion and exclusion criteria is provided in the Online Resource 1 [Online Supplemental Material (OSM)]. Given the known very low diclofenac exposure following FDETS usage compared to oral diclofenac, specific monitoring for cardiovascular or renal events was not undertaken.
2.2 Treatment and Assessment
Eligible patients were given 28 FDETS, each containing 180 mg of diclofenac epolamine, equivalent to 140 mg of diclofenac sodium. Data from a pharmacokinetic study in healthy adult volunteers show that approximately 5–6% of the diclofenac epolamine content of a patch is released during the 12- to 24-h application period [19].
Study personnel demonstrated to patients and parents/guardians how to apply FDETS at the injury site and applied the first topical system at the end of the inclusion visit. After that, patients or their parents/guardians were instructed to apply one FDETS in the morning and another 12 h later, each day until they returned to the clinic for the final visit (pain resolution or Day 14), and were requested to have a topical system in place at the time of each visit.
If the site of injury was such that the edges of the FDETS were going to overlap after application, it was trimmed to avoid overlap, and if a patch needed to be replaced because of exposure to water (e.g., during bathing or swimming), a third topical system could be used in a single day.
In addition to the Day 1 visit, patients were asked to return to the clinic on Days 2, 4, 7, and 14, but were allowed to exit the study at any time for any reason. Therefore, the final study visit was defined as Day 14 or the day after pain resolution. Because of inconsistent visit times by patients, visits were categorized as follows: screening, Days 1–2 after treatment initiation, Days 3–4, Days 5–7, Days 8–11, and Days 12–15. On Day 2 (24 h after first application) and at the final visit, a blood sample was collected for the assessment of diclofenac concentration.
Pre-treatment baseline pain was assessed in the clinic prior to the first FDETS application. The Wong-Baker FACES® Pain Rating Scale (0 = No hurt; 5 = Hurts worst) [18] was used to assess pain severity. Patients were administered the Pain scale by the study personnel at the site on the occasion of the first in-clinic visit (inclusion visit). During the treatment period at home, pain was self-assessed by patients using the same scale and it was recorded in their personal diary. At each post-enrollment visit, the pain score, AEs, local tolerability (application site reactions), and vital signs were recorded by the study personnel, and at the final visit, the Investigator assessed the patient’s global response to therapy. Local tolerance was evaluated following patch removal by the Investigator using an application-site scoring scheme (described in Sect. 2.4), with a fresh patch to be applied on completion of the examination. AEs were categorized using the Medical Dictionary for Regulatory Activities (MedDRA) codes.
Patients were asked to rate their pain in the morning and evening of each day and record this information in a diary; the first diary entry was made on the evening after the first FDETS was applied in the clinic. Patients were monitored throughout the study for AEs and were also asked to record any AEs, local tolerability issues, and/or concomitant medication/treatment in their diaries.
Patients were instructed not to use any other topical medication within the injured area for the duration of the study, as well as any medications that may interact with diclofenac, or pose a risk to patients (e.g., selective serotonin reuptake inhibitors, lithium, antidiabetic agents, or anticoagulants), any over-the-counter analgesics, short- or long-acting NSAIDs, narcotic analgesics, systemic steroidal anti-inflammatory agents, or immunosuppressive therapy. Patients were permitted to use rest-ice-compression-elevation (RICE) techniques both before and during the study. Any unused topical systems were to be returned to the clinic at the final visit.
2.3 Bioanalytic Assay
Two 5 mL blood samples were collected from each patient for the assessment of diclofenac concentration, the first at Visit 2, 24 h after initial patch application on Day 1, and the second on the day of discontinuation from the study (i.e., following pain resolution or at the latest on Day 14). Both sample collections were made while the patch was still applied to the injury site. It should be noted that these were not at specific pre-dose timepoints, as the study protocol directed patch application in the evening and on the morning of the following day. Therefore, two to three patches may have been applied by the time of the first blood draw, depending on the time of the first visit.
Diclofenac concentrations were determined in plasma at inVentiv Health Clinique, inc., Québec (Canada) (now Syneos Health), according to a fully validated method described using high performance liquid chromatography (HPLC), with tandem mass spectrometry detection (MS-MS) having a quantitation range of 50–50,000 pg/mL (0.05–50 ng/mL).
The analytical methodology is provided in detail as OSM Resource 2.
2.4 Outcomes
The primary endpoint of this study was local tolerability (redness, swelling) and systemic safety. AEs were categorized using MedDRA codes. Local tolerability was assessed at each clinical visit using a seven-item scale, where a score of 0 = no skin changes; 1 = faint redness; 2 = moderate redness; 3 = intense redness; 4 = redness with edema and papules; 5 = redness with weeping vesicles, blisters, or bullae; and 6 = redness with an extension of effect beyond the margin of the contact site.
Secondary endpoints included an assessment of the analgesic efficacy of FDETS, assessed by both patients and investigators on an ordinal scale, and stratified by age (6–11 years and 12–16 years) and diclofenac plasma concentrations in children in comparison to data obtained in a comparative study of FDETS versus oral diclofenac in adults (Study CRO-PK-01-72; data on file, IBSA). The study protocol and results of CRO-PK-01-72 are summarized in OSM Resource 3. Analgesic efficacy was assessed by patients using the Wong-Baker FACES® Pain Rating Scale (from 0 = no hurt to 5 = most hurt) [18]. Investigators provided an assessment of global response to therapy on a 5-point scale from 1 = no clinical improvement in pain intensity and/or functional performance to 5 = restoration of normal functional performance in the absence of any pain. For comparative purposes, pain score data were compared with data from another study in adults (00GB/Fp05; data on file, IBSA).
2.5 Statistical Analysis
Based on previous studies in adults, a population of 100 patients would have 80% power to detect a mean change from baseline of 0.354 in pain intensity score (on a 0–5 scale) with a two-sided alpha of 0.05. In a population of this size, the 95% confidence intervals (CIs) for an AE incidence of 10% would be 4.9–17.6%.
Data were analyzed in all patients who applied ≥ 1 FDETS, with separate analyses undertaken in children aged 6–11 and 12–16 years. The two age classes were defined by the FDA according to regulatory and scientific standards [20]. The lower limit of the younger pediatric subgroup was set under the assumption that 6 years of age approximates the age at which children have sufficient size and aggressiveness to be at increased risk of minor soft tissue injuries requiring pain therapy, and the upper limit of 16 years represents the maximum age for a pediatric population according to the FDA.
Continuous variables were expressed as means with standard deviation and range. Categorical variables were expressed as number and percentage. The two age groups were compared using the t-test for continuous variables and Fisher’s exact test for categorical variables. A mixed model, adjusting for multiple assessments per patient, was used for analysis of plasma diclofenac concentrations.
Twice-daily pain scores from patient diaries expressed as a proportion of the pre-treatment pain score for each patient were analyzed. A pain score of 1.0 indicated no change from baseline, while 0.0 indicated no discernible pain. Analyses were truncated at Day 13 (morning) in order to remove time periods with too few patients. Statistical analyses used a generalized estimating equation (GEE) model on all post-treatment pain scores with categorical factors for age category (6–11 years, 12–16 years, and adults) and assessment period (Day 0 evening, Day 1 morning–Day 1 evening, Day 2 morning–Day 2 evening, etc.). Multiple values from the same patient were treated as repeated measures using an independent correlation structure. The three individual group comparisons were not adjusted for multiplicity, and imputation for missing data was not performed. Global responses in the two age groups were compared using Fisher’s exact test.
For the pharmacokinetic analysis, individual, median, and mean steady-state diclofenac concentrations for each of the two age subgroups were calculated. Data from blood draws > 13 h after the last FDETS application were excluded. The comparable adult data came from the separate CRO-PK-01-72 Study, with blood drawn from 0 to 24 h on Day 4 after steady-state concentrations were reached. The 90% CI of the difference between the estimated geometric means of plasma diclofenac concentrations after FDETS application in the adult and pediatric studies was calculated. In addition, the mean steady-state diclofenac concentrations from the pediatric study were compared with the mean maximum serum concentration resulting from a single 50 mg oral diclofenac tablet in the adult study.
Statistical analyses of the three FDETS treatment groups used a GEE model with a single factor for treatment. Multiple values from the same patient were treated as repeated measures using an exchangeable correlation structure. The three individual group comparisons were not adjusted for multiplicity. Data were analyzed using SAS version 9.2 (SAS Institute, Inc., Cary, NC, USA).
3 Results
3.1 Patients
A total of 104 patients were included, aged 6–11 years (n = 52) and 12–16 years (n = 52). 100 patients provided two blood samples as planned, and four patients provided only one sample. Ninety patients completed the protocol with pain resolution, 12 completed without pain resolution (i.e., pain score > 0), and two patients withdrew from the study with pain: one because of a fracture, and the other because of an excluded concomitant treatment.
Sixty-eight patients (65.4%) were male, and 36 were female (34.6%); most (70.2%) were Caucasian (Table 1). The mean age of the overall population was 11.6 years. The most common site of injury was the ankle (n = 37), followed by the knee (n = 11), foot (n = 11), and wrist (n = 10).
Aside from the expected differences in weight and height, there were no notable differences in patient characteristics between the age groups, except baseline pain was greater for the older versus the younger cohort (3.37 vs. 3.58, respectively; p = 0.075).
The mean number of treatment days was 9.5, and patients used a mean of 19.8 FDETS during the study (mean 2.1 per day). Six patients trimmed the FDETS to fit the injury site.
3.2 Safety
Tolerability score was the primary study outcome. At screening, 93% of patients had a tolerability score of zero (no skin changes) on the local tolerability assessment scale (7% had a score of 1), increasing to 100% with a score of 0 by the end of the study among those still using FDETS (n = 33) (Table 2). The highest score seen during the study was 1 (faint redness).
Thirty-two study participants experienced 54 AEs; 26 events occurred in 14 patients in the group aged 6–11 years (26.9%), and 28 events in 18 patients in the group aged 12–16 years (34.6%). There were no serious AEs.
The most common AEs were headache (n = 9), pruritus (n = 7), nausea (n = 3), stomach discomfort (n = 3), dizziness (n = 2), fatigue (n = 2), upper abdominal pain (n = 2), erythema (n = 2), and epistaxis (n = 2; Table 3). Events occurring in a single patient were motion sickness, abdominal pain, loose stools, vomiting, lice infestation, concussion, excoriation, scratch, muscle spasms, myalgia, enuresis, cough, nasopharyngitis, exfoliative dermatitis, dry skin, flushing, and vasovagal syncope.
All AEs were of mild or moderate severity (44 mild and 10 moderate). Fourteen events in nine patients (8.7%) were deemed at least possibly related to FDETS—six events in three patients aged 6–11 years and eight events in six patients aged 12–16 years. The most common was pruritus, of which there were nine events in six patients (five events in two patients aged 6–11 years and four events in four patients aged 12–16 years). Other possibly treatment-related AEs occurred once in one patient each: nausea (6–11 years), headache (12–16 years), exfoliative dermatitis (12–16 years), dry skin (12–16 years), and erythema (12–16 years). Vital signs remained within normal limits throughout the study.
3.3 Pain Response
Pain scores declined somewhat more rapidly for patients aged 6–11 years compared with patients aged 12–16 years, with the latter profile similar to that of data from another study in adults (Fig. 1). The results of multivariate regression analysis revealed that the reduction in pain over the course of the study was significantly greater for patients aged 6–11 years than for either 12- to 16-year-olds or adults (Fig. 1).
Change from baseline in pain scores. Data from the two pediatric cohorts (6–11 years and 12–16 years) were compared with similar data from another study in adults (00GB/Fp05) included in the Flector New Drug Application submission to the US Food and Drug Administration. P values were derived from a generalized estimating equation (GEE) model with factors for treatment and day, and an independent correlation structure for repeated measures
Analysis of clinic visit pain scores demonstrated a decline to “0” over the course of the study for 90 patients (87%), and the majority of those who did not reach “0” (11/14) had a score of “1”, with fewer patients in the younger versus older cohort having residual pain (4/7.7% vs. 10/19.2%, p = 0.149).
According to the physician’s assessment of global response to treatment, all but one patient in each age group showed clinical improvement, and 87 (83.7%) patients were restored to normal function with no pain: 47 (90.4%) in the 6- to 11-year age group and 40 (76.9%) patients in the 12- to 16-year age group (p = 0.110).
3.4 Pharmacokinetics
The mean diclofenac concentration for all patients, adjusted for six patients who only received a partial patch, was 1.65 ng/mL at the 24-h time point (first assessment) and 1.80 ng/mL at the final visit (last assessment). Diclofenac concentration tended to be slightly higher in the younger age group compared with older patients: 1.83 versus 1.46 ng/mL, respectively, at the first assessment and 2.49 versus 1.11 ng/mL, respectively, at the last assessment. The higher concentration in the younger age group persisted after excluding samples collected >13 h post-application and after dose adjustment associated with trimming the topical system (n = 6), and were statistically significant at the last assessment (p = 0.002).
An analysis of diclofenac plasma concentrations in pediatric patients was compared with data from adult patients following diclofenac patch administration in the previous study (CRO-PK-01-72). It showed significantly higher concentrations for the youngest patients in comparison to either older pediatric patients or adults, with the latter two cohorts being similar (Fig. 2). Mean/median plasma values for all three cohorts were, however, less than 1/500th of those obtained from adults treated with 50 mg of oral diclofenac (Fig. 2).
Plasma levels of diclofenac. Data from children aged 6–11 years and 12–16 years were compared to adults treated with either FDETS (two DETS/day for 4 days) or a single oral dose of 50 mg diclofenac sodium. Adult data were included in the Flector New Drug Application submission to the US Food and Drug Administration (Study CRO-PK-01-72). P values were derived from a generalized estimating equation (GEE) model with a factor for treatment, and an independent correlation structure for repeated measures. Cmax maximum plasma concentration
Using adjusted plasma diclofenac concentrations collected at < 13 h after the last patch application in order to remove concentrations that might be characteristic of the elimination phase, the geometric mean in the total pediatric population was estimated to be 1.07 ng/mL, compared with 1.18 ng/mL in the historical adult population from Study CRO-PK-01-72, a study in which both oral (diclofenac 50 mg) and topical (FDETS twice daily for 4 days) diclofenac exposure was assessed. These data yielded a 90% CI of 0.81–1.02 for the ratio of the pediatric-adult population geometric means, indicating that the two populations were equivalent with respect to plasma diclofenac exposure after patch application.
Since pain relief was somewhat more rapid in the youngest pediatric patients, particularly during the first 7 days of treatment, a repeated-measures analysis of variance was performed over Days 0–7, with maximum adjusted diclofenac plasma concentrations, baseline pain score, sex, center, age-category, and day in the model. Although baseline pain, age, and day were significant predictors of outcome (chi-square 13.06, p < 0.001; 6.35, p < 0.012; and 261.11, p < 0.001, respectively), the p-value for diclofenac plasma concentrations was not statistically significant (chi-square 0.19, p = 0.666).
4 Discussion
This study explored the safety and analgesic efficacy of FDETS in children aged 6–16 years with minor soft tissue injuries. There was a low potential risk of local or systemic AEs, and indeed, no serious AEs were observed in pediatric patients with minor soft tissue injuries receiving FDETS. The decline in pain scores for patients aged 12–16 years was similar to adults [11,12,13]. Systemic diclofenac exposure was minimal in the pediatric study population, as has been observed in adult patients treated with FDETS. Although there was minor age-related variability in mean diclofenac concentration 24 h after administration and at the final visit—slightly higher diclofenac plasma concentrations were observed in the subgroup of younger patients (6–11 years old)—this was somewhat to be expected considering the smaller surface and blood volume, in average, in this pediatric age class as compared to adults. However, the overall similarity between pharmacokinetic profiles and pain score data in pediatric subjects and an historical adult population is consistent with that obtained with FDETS in adults, and provides evidence that the FDETS delivers diclofenac and reduces pain in a similar manner in both pediatric and adult subjects. The data suggest that diclofenac plasma concentrations in children aged 6–16 years would not be expected to be higher than in adults following application of the FDETS according to current labeling, and safety data generated in the current pediatric study further suggest they are unlikely to experience safety issues not previously reported in older subjects.
The safety profile for FDETS in children was also similar to that in adults [11,12,13], with the most common AEs being headache (8.7%) and pruritus (6.7%). In the pediatric population, gastrointestinal (GI) events occurred in 9.6% of patients, of which nausea occurred in 2.9%, abdominal discomfort in 2.9%, and upper abdominal pain in 1.9%, only one of which (nausea) was considered to be treatment-related. A pooled analysis of published FDETS data (n = 890) indicated a similarly low incidence of GI AEs: nausea in 1.5%, abdominal discomfort in 0.6%, and abdominal pain in 0.4% [21]. In particular, the low incidence of GI AEs following application of FDETS makes it an attractive treatment option for children.
Faint redness was the only response to FDETS noted by the Investigators in local tolerability assessments. This was consistent with data in adults showing that FDETS exhibited local tolerability comparable to a placebo topical system [11, 13]. There were no unique safety signals in the pediatric population that might change the product's risk profile in this patient group compared with adults.
The analgesic response over the first 7 days of treatment was greater in the patients aged 6–11 years than in patients aged 12–16 years, and the overall response was significantly better in comparison to both the older pediatric cohort as well as an adult historical control group. The superior analgesic response in the young pediatric patients was not correlated with diclofenac plasma concentrations as these were quite low and correspondingly variable, suggesting that plasma concentrations may not be correlated with tissue concentrations attained under the topical system.
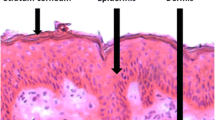
Children treated with FDETS had low systemic exposure to diclofenac. Although the younger cohort had significantly higher diclofenac plasma concentrations than either the older pediatric patients or an adult historical control group, it is not clear whether this is due to differences in the histology of the skin of the younger children or other factors. Most importantly, however, plasma concentrations of diclofenac following oral dosing with diclofenac in adults were > 500-fold greater than those resulting from FDETS exposure of either children or adults (Study CRO-PK-01-72), highlighting the principal advantage of FDETS over any systemic analgesic, including NSAIDs and acetaminophen.
The topical route of drug administration is attractive for treating children with minor soft tissue injuries because they sometimes have difficulty swallowing tablets or capsules, and because their skin is well perfused but relatively thin [22]. Importantly, the data show FDETS has excellent local and systemic tolerability with no evidence of allergic reactions.
4.1 Limitations
The present study has three main limitations: the first limitation is the absence of blinding (i.e., the open-label design); the second is the lack of a concurrent control group (e.g., a placebo topical system); and the third is the use of historical adult data.
5 Conclusions
This study demonstrates that FDETS can safely and effectively provide pain relief for minor soft tissue injuries in pediatric patients, with minimal systemic NSAID exposure and low potential risk of either local or systemic AEs. The safety, efficacy, and pharmacokinetic profile of the FLECTOR topical system in the pediatric population was consistent with data in adults obtained from a previous study.
References
Stanos S. Topical analgesics. Phys Med Rehabil Clin N Am. 2020;31:233–44. https://doi.org/10.1016/j.pmr.2020.02.002.
McPherson ML, Cimino NM. Topical NSAID formulations. Pain Med. 2013;14(Suppl 1):S35–9. https://doi.org/10.1111/pme.12288.
Derry S, Wiffen PJ, Kalso EA, Bell RF, Aldington D, Phillips T, et al. Topical analgesics for acute and chronic pain in adults—an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;5: CD008609. https://doi.org/10.1002/14651858.CD008609.pub2.
Honvo G, Leclercq V, Geerinck A, Thomas T, Veronese N, Charles A, et al. Safety of topical non-steroidal anti-inflammatory drugs in osteoarthritis: outcomes of a systematic review and meta-analysis. Drugs Aging. 2019;36:45–64. https://doi.org/10.1007/s40266-019-00661-0.
Makris UE, Kohler MJ, Fraenkel L. Adverse effects of topical nonsteroidal antiinflammatory drugs in older adults with osteoarthritis: a systematic literature review. J Rheumatol. 2010;37:1236–43. https://doi.org/10.3899/jrheum.090935.
Wiffen PJ, Xia J. Systematic review of topical diclofenac for the treatment of acute and chronic musculoskeletal pain. Curr Med Res Opin. 2020;36:637–50. https://doi.org/10.1080/03007995.2020.1716703.
Taylor RS, Fotopoulos G, Maibach H. Safety profile of topical diclofenac: a meta-analysis of blinded, randomized, controlled trials in musculoskeletal conditions. Curr Med Res Opin. 2011;27:605–22. https://doi.org/10.1185/03007995.2010.550606.
Seth AK. Transdermal drug therapy: emerging techniques and improved patient compliance. In: Misra A, Shahiwala A, editors. Novel drug delivery technologies. Singapore: Springer Nature; 2019. p. 261–89.
Derry S, Wiffen P, Moore A. Topical nonsteroidal anti-inflammatory drugs for acute musculoskeletal pain. JAMA. 2016;315:813–4. https://doi.org/10.1001/jama.2016.0249.
US Food and Drug Administration (FDA). Flector patch (diclofenac epolamine topical patch) 1.3%. Approved product label. 2007
Galer BS, Rowbotham M, Perander J, Devers A, Friedman E. Topical diclofenac patch relieves minor sports injury pain: results of a multicenter controlled clinical trial. J Pain Symptom Manage. 2000;19:287–94. https://doi.org/10.1016/s0885-3924(00)00125-1.
Gimbel J, Jacobs D, Pixton G, Paterson C. Effectiveness and safety of diclofenac epolamine topical patch 1.3% for the treatment of acute pain due to back strain: an open-label, uncontrolled study. Phys Sportsmed. 2011;39:11–8. https://doi.org/10.3810/psm.2011.02.1857.
Kuehl K, Carr W, Yanchick J, Magelli M, Rovati S. Analgesic efficacy and safety of the diclofenac epolamine topical patch 1.3% (DETP) in minor soft tissue injury. Int J Sports Med. 2011;32:635–43. https://doi.org/10.1055/s-0031-1275359.
Yanchick J, Magelli M, Bodie J, Sjogren J, Rovati S. Time to significant pain reduction following DETP application vs placebo for acute soft tissue injuries. Curr Med Res Opin. 2010;26:1993–2002. https://doi.org/10.1185/03007995.2010.493099.
Polieri T, Saponati G. Minor sport injuries in children: a new, safe, topical preparation containing DHEP (Diclofenac Epolamine). Med Sport (Roma). 2000;53:275–8.
Costantino C, Kwarecki J, Samokhin AV, Mautone G, Rovati S. Diclofenac epolamine plus heparin plaster versus diclofenac epolamine plaster in mild to moderate ankle sprain: a randomized, double-blind, parallel-group, placebo-controlled, multicentre, phase III trial. Clin Drug Investig. 2011;31:15–26. https://doi.org/10.2165/11585890-000000000-00000.
Petersen B, Rovati S. Diclofenac epolamine (Flector) patch: evidence for topical activity. Clin Drug Investig. 2009;29:1–9. https://doi.org/10.2165/0044011-200929010-00001.
Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14:9–17.
Rainsford KD, Kean WF, Ehrlich GE. Review of the pharmaceutical properties and clinical effects of the topical NSAID formulation, diclofenac epolamine. Curr Med Res Opin. 2008;24:2967–92. https://doi.org/10.1185/03007990802381364.
Pediatric Exclusivity Study Age Group. Available from URL: https://www.fda.gov/drugs/data-standards-manual-monographs/pediatric-exclusivity-study-age-group. Accessed 18 Nov 2021.
Brewer AR, Pierchala LA, Yanchick JK, Magelli M, Rovati S. Gastrointestinal tolerability of diclofenac epolamine topical patch 13%: a pooled analysis of 14 clinical studies. Postgrad Med. 2011;123:168–76. https://doi.org/10.3810/pgm.2011.07.2316.
Batchelor HK, Marriott JF. Formulations for children: problems and solutions. Br J Clin Pharmacol. 2015;79:405–18. https://doi.org/10.1111/bcp.12268.
Acknowledgements
Medical writing and editorial support for this article were provided by Catherine Rees and Marion Barnett on behalf of Springer Healthcare Communications, and Ray Hill, an independent medical writer. This assistance was funded by IBSA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This clinical trial was financially supported by IBSA Institut Biochimique SA, Pambio-Noranco, Switzerland.
Conflict of interest
FH is an IBSA consultant. At the time of the study, CAJ and CJ were employees of IBSA Pharma Inc., a wholly-owned subsidiary of IBSA. VF is an employee of IBSA CH. GL and PPW have no financial interests in either FDETS or IBSA CH or its affiliate.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
CAJ: contributed to protocol design and study management, reviewed study data, authored the CSR, and reviewed/revised the manuscript. FH: prepared the study statistical analysis plan (SAP), oversaw study data management and analysis, provided additional statistical analysis for the manuscript, and reviewed/revised the manuscript. VF: reviewed the manuscript. GL and PPW: reviewed and executed the protocol and reviewed the manuscript. CJ: contributed to protocol design and study management, reviewed study data and the clinical study report (CSR), and reviewed/revised the manuscript.
Ethics approval
A central institutional review board approved the protocol at each participating site, and the study was conducted according to the ethical principles of human research established by the Declaration of Helsinki and its amendments.
Consent to participate
Informed consent by way of a Parental Permission Form was obtained in writing from parents/legally authorized representatives and, in addition, children aged 10–16 years were required to sign a Children’s Assent Form, before the commencement of study procedures.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jones, C.A., Hoehler, F.K., Frangione, V. et al. Safety and Efficacy of the FLECTOR (Diclofenac Epolamine) Topical System in Children with Minor Soft Tissue Injuries: A Phase IV Non-randomized Clinical Trial. Clin Drug Investig 42, 43–51 (2022). https://doi.org/10.1007/s40261-021-01101-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-021-01101-x