Abstract
Background
The US Food and Drug Administration Adverse Event Reporting System (FAERS), a post-marketing safety database, can be used to differentiate brand versus generic safety signals.
Objective
To explore the methods for identifying and analyzing brand versus generic adverse event (AE) reports.
Methods
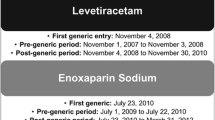
Public release FAERS data from January 2004 to March 2015 were analyzed using alendronate and carbamazepine as examples. Reports were classified as brand, generic, and authorized generic (AG). Disproportionality analyses compared reporting odds ratios (RORs) of selected known labeled serious adverse events stratifying by brand, generic, and AG. The homogeneity of these RORs was compared using the Breslow-Day test. The AG versus generic was the primary focus since the AG is identical to brand but marketed as a generic, therefore minimizing generic perception bias. Sensitivity analyses explored how methodological approach influenced results.
Results
Based on 17,521 US event reports involving alendronate and 3733 US event reports involving carbamazepine (immediate and extended release), no consistently significant differences were observed across RORs for the AGs versus generics. Similar results were obtained when comparing reporting patterns over all time and just after generic entry. The most restrictive approach for classifying AE reports yielded smaller report counts but similar results.
Conclusion
Differentiation of FAERS reports as brand versus generic requires careful attention to risk of product misclassification, but the relative stability of findings across varying assumptions supports the utility of these approaches for potential signal detection.





Similar content being viewed by others
References
Generic Pharmaceutical Association (GPhA). 2016 Generic drug savings and access in the United States report. http://www.gphaonline.org/media/generic-drug-savings-2016/index.html. Accessed 28 Nov 2016.
Crawford P, et al. Are there potential problems with generic substitution of antiepileptic drugs? A review of issues. Seizure. 2006;15(3):165–76.
Del Tacca M, et al. Lack of pharmacokinetic bioequivalence between generic and branded amoxicillin formulations. A post-marketing clinical study on healthy volunteers. Br J Clin Pharmacol. 2009;68(1):34–42.
Colombo GL, et al. Off-patent generic medicines vs. off-patent brand medicines for six reference drugs: a retrospective claims data study from five local healthcare units in the Lombardy Region of Italy. PLoS One. 2013;8(12):e82990.
Erickson SC, et al. Clinical and pharmacy utilization outcomes with brand to generic antiepileptic switches in patients with epilepsy. Epilepsia. 2011;52(7):1365–71.
Kim SH, et al. Efficacy and tolerability of a generic and a branded formulation of atorvastatin 20 mg/d in hypercholesterolemic Korean adults at high risk for cardiovascular disease: a multicenter, prospective, randomized, double-blind, double-dummy clinical trial. Clin Ther. 2010;32(11):1896–905.
Tsadok MA, et al. Amiodarone-induced thyroid dysfunction: brand-name versus generic formulations. CMAJ. 2011;183(12):E817–23.
Borgheini G. The bioequivalence and therapeutic efficacy of generic versus brand-name psychoactive drugs. Clin Ther. 2003;25(6):1578–92.
Drugs@FDA Glossary of Terms. http://www.fda.gov/Drugs/InformationOnDrugs/ucm079436.htm#ANDA. Accessed 28 Nov 2016.
Faasse K, C T, Gamble G, Petrie KJ. The effect of an apparent change to a branded or generic medication on drug effectiveness and side effects. Psychosom Med. 2013;75:90–6.
Kesselheim AS, et al. Variations in patients’ perceptions and use of generic drugs: results of a national survey. J Gen Intern Med. 2016;31(6):609–14.
Kesselheim AS, et al. Prevalence and predictors of generic drug skepticism among physicians: results of a national survey. JAMA Intern Med. 2016;176(6):845–7.
US Food and Drug Administration. List of authorized generic drugs. 2014. http://www.fda.gov/drugs/developmentapprovalprocess/howdrugsaredevelopedandapproved/approvalapplications/abbreviatednewdrugapplicationandagenerics/ucm126389.htm. 22 May 2014.
Ahmad SR. Adverse drug event monitoring at the Food and Drug Administration. J Gen Intern Med. 2003;18(1):57–60.
FDA Adverse Event Reporting System (FAERS). https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Surveillance/AdverseDrugEffects/default.htm. Accessed 24 Apr 2017.
Sakaeda T, et al. Data mining of the public version of the FDA adverse event reporting system. Int J Med Sci. 2013;10(7):796–803.
Medical Dictionary for Regulatory Activities. Standardised MedDRA Queries. 2015. http://www.meddra.org/standardised-meddra-queries. Cited 3 Jan 2015.
Medical Dictionary for Regulatory Activities. MedDRA hierarchy. 2015. http://www.meddra.org/how-to-use/basics/hierarchy. Cited 3 Jan 2015.
Postmarketing reporting of adverse drug experiences. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=314.80. Accessed 22 Sept 2016.
Request for waiversto postmarketing safety reporting requirements. http://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/ucm074850.htm#REQUESTSFORWAIVERSTOPOSTMARKETINGSAFETYREPORTINGREQUIREMENTS. Accessed 22 Sept 2016.
Almenoff J, et al. Perspectives on the use of data mining in pharmaco-vigilance. Drug Saf. 2005;28(11):981–1007.
Egberts AC, Meyboom RH, van Puijenbroek EP. Use of measures of disproportionality in pharmacovigilance: three Dutch examples. Drug Saf. 2002;25(6):453–8.
Rahman MM, et al. Comparison of brand versus generic antiepileptic drug adverse event reporting rates in the US Food and Drug Administration Adverse Event Reporting System (FAERS). Epilepsy Res. 2017;135:71–8.
Authorized Generics. http://www.authorizedgenerics.com/default.asp?contentID=29. Accessed 19 Sept 2016.
Guidance for Industry. E2E pharmacovigilance planning. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM073107.pdf. Accessed 24 Apr 2017.
Iyer G, et al. An algorithm to identify generic drugs in the FDA adverse event reporting system. Drug Saf. 2017. doi:https://doi.org/10.1007/s40264-017-0550-1
Drugs@FDA. Lamotrigine. http://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=BasicSearch.process. Accessed 01 Dec 2016.
Acknowledgements
The authors thank Wenlei Jiang, PhD (FDA) and Saranrat Wittayanukorn, PhD (FDA) for their thoughtful contributions to the study design and data analysis.
Funding for this work was made possible by the FDA through grant 1U01FD005272. Views expressed do not necessarily reflect the official policies of the Department of Health and Human Services, nor does any mention of trade names, commercial practices, or organization imply endorsement by the US Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the US Food and Drug Administration through Grant 1U01FD005272.
Conflict of interest
In the past 3 years, Richard Hansen has provided expert testimony for Boehringer Ingelheim and Daiichi Sankyo. No other authors declare a potential conflict of interest. The sponsor of this study (FDA) has provided suggestions for study design, interpretation of the results and development of the manuscripts. However, the ultimate decisions came from all the authors. Views expressed do not necessarily reflect the official policies of the Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rahman, M.M., Alatawi, Y., Cheng, N. et al. Methodological Considerations for Comparison of Brand Versus Generic Versus Authorized Generic Adverse Event Reports in the US Food and Drug Administration Adverse Event Reporting System (FAERS). Clin Drug Investig 37, 1143–1152 (2017). https://doi.org/10.1007/s40261-017-0574-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0574-4