Abstract
Introduction
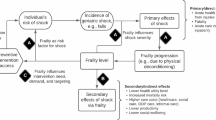
The clinical importance of frailty is increasing. Existing economic evaluations of interventions to manage frailty have limited time horizons, but even in older populations there may be important longer-term differences in costs and outcomes. This paper reports on the development of a cost-effectiveness model to predict publicly funded health and aged care costs and quality-adjusted life years (QALYs) over the remaining lifetime of frail Australians and a model-based cost-utility analysis of a physiotherapy-based intervention for frail individuals.
Methods
A cohort-based state transition (Markov) model was developed to predict costs and QALYs over the remaining lifetime of a frail population. Frailty is defined using the phenotypic definition of frailty, and the model comprises health states that describe frailty status, residential status, the experience of bone fractures and depression, and death. Model input parameters were estimated and calibrated using the Dynamic Analyses to Optimise Ageing dataset, supplemented with data from the published literature.
Results
The cost-effectiveness model was subject to a range of validation approaches, which did not negate the validity of the model. The evaluated physiotherapy-based frailty intervention has an expected incremental cost per QALY gained of Australian $8129 compared to usual care, but there is a probability of 0.3 that usual care is more effective and less costly than the intervention.
Discussion
Frailty reduces quality of life, is costly to manage and it’s prevalence is increasing, but new approaches to managing frailty need to demonstrate value for money. The value of the reported cost-effectiveness model is illustrated through the estimation of all important costs and effects of a physiotherapy-based frailty intervention, which facilitates comparisons with funding decisions for other new technologies in Australia.


Similar content being viewed by others
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in older people. Lancet. 2013;381(9868):752–62.
Milte C, Walker R, Luszcz M, Lancsar E, Kaambwa B, Ratcliffe J. How important is health status in defining quality of life for older people? An exploratory study of the views of older South Australians. Appl Health Econ Health Policy. 2014;12(1):73–84.
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–92.
National Institute for Health and Clinical Excellence. Dementia, disability and frailty in later life—mid-life approaches to delay or prevent onset. NICE guideline. http://www.nice.org.uk/guidance/ng16. Accessed 27 May 2016 (20 October 2015).
Cameron ID, Fairhall N, Langron C, Lockwood K, Monaghan N, Aggar C, et al. A multifactorial interdisciplinary intervention reduces frailty in older people: randomized trial. BMC Med. 2013;11(1):65.
Fairhall N, Sherrington C, Kurrle SE, Lord SR, Lockwood K, Howard K, et al. Economic evaluation of a multifactorial, interdisciplinary intervention versus usual care to reduce frailty in frail older people. J Am Med Directors Assoc. 2015;16(1):41–8.
Karnon J, Brennan A, Akehurst R. A critique and impact analysis of decision modeling assumptions. Med Decis Mak. 2007;27(4):491–9.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults evidence for a phenotype. J Gerontol Ser A. 2001;56(3):M146–57.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–36.
Organisation for Economic Co-operation and Development (OECD). Stat. Purchasing power parities for GDP and related indicators. 2016. http://stats.oecd.org/#.
Australian Institute of Health and Welfare. Health expenditure Australia 2013–2014. Health and welfare expenditure series no. 54. Cat. no. HWE 63. Canberra: AIHW; 2015.
Pharmaceutical Benefits Advisory Committee. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (version 4.4). Canberra: Department of Health; 2015. http://www.pbac.pbs.gov.au/section-d/section-d-cea/d4-variables-in-the-economic-evaluation.html. Accessed 27 May 2016.
Tom SE, Adachi JD, Anderson FA, Boonen S, Chapurlat RD, Compston JE, et al. Frailty and fracture, disability, and falls: a multiple country study from the global longitudinal study of osteoporosis in women. J Am GeriatrSoc. 2013;61:327–34.
Mezuk B, Edwards L, Lohman M, Choi M, Lapane K. Depression and frailty in later life: a synthetic review. Int J Geriatr Psychiatry. 2012;27(9):879–92.
Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, et al. Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol Ser A Biol Sci Med Sci. 2006;61(3):262–6.
Anstey KJ, Byles JE, Luszcz MA, Mitchell P, Steel D, Booth H, et al. Cohort profile: the dynamic analyses to optimize ageing (DYNOPTA) project. Int J Epidemiol. 2009;39(1):44–51.
Theou O, Cann L, Blodgett J, Wallace LMK, Brothers TD, Rockwood K. Modifications to the frailty phenotype criteria: systematic review of the current literature and investigation of 262 frailty phenotypes in the Survey of Health, Ageing, and Retirement in Europe. Ageing Res Rev. 2015;21:78–94.
Vasiliadis HM, Dionne PA, Préville M, Gentil L, Berbiche D, Latimer E. The excess healthcare costs associated with depression and anxiety in elderly living in the community. Am J Geriatr Psychiatry. 2013;21(6):536–48.
Watts JJ, Abimanyi-Ochom J, Sanders KM. Osteoporosis costing all Australians: a new burden of disease analysis–2012 to 2022. Osteoporosis Australia. 2013 (ISBN: 978-0-9923698-1-1).
Sanders KM, Seeman E, Ugoni AM, Pasco JA, Martin TJ, Skoric B, et al. Age- and gender-specific rate of fractures in Australia: a population-based study. Osteoporos Int. 1999;10(3):240–7.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–92.
Brazier JE, Green C, Kanis JA. A systematic review of health state utility values for osteoporosis-related conditions. Osteoporos Int. 2002;13(10):768–76.
Vemer P, Corro Ramos I, van Voorn GA, Al MJ, Feenstra TL. AdViSHE: a validation-assessment tool of health-economic models for decision makers and model users. Pharmacoeconomics. 2016;34(4):349–61.
Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, Osteoporotic Fractures in Men Research Group, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57:492–8.
Karnon J, Vanni T. Calibrating models in economic evaluation: a comparison of alternative measures of goodness of fit, parameter search strategies and convergence criteria. Pharmacoeconomics. 2011;29(1):51–62.
Pharmaceutical Benefits Scheme. Sorafenib; 200 mg tablet 60; Nexavar® Public Summary Document—March 2015 PBAC Meeting. 2015. http://www.pbs.gov.au/info/industry/listing/elements/pbac-meetings/psd/2015-03/sorafenib-nexavar-psd-03-2015. Accessed on 31 August 2016.
Pharmaceutical Benefits Scheme. Lenvatinib: 4 mg capsule, 3010 mg capsule, 30, Lenvima® Public Summary Document—March 2016 PBAC Meeting. 2016. http://www.pbs.gov.au/info/industry/listing/elements/pbac-meetings/psd/2016-03/lenvatinib-lenvima-psd-03-2016. Accessed on 31 August 2016.
Looman WM, Huijsman R, Bouwmans-Frijters CAM, Stolk EA, Fabbricotti IN. Cost-effectiveness of the ‘Walcheren Integrated Care Model’ intervention for community-dwelling frail elderly. Fam Pract. 2016;33(2):154–60.
Sandberg M, Jakobsson U, Midlöv P, Kristensson J. Cost-utility analysis of case management for frail older people: effects of a randomised controlled trial. Health Econ Rev. 2015;5:12.
Tanajewski L, Franklin M, Gkountouras G, Berdunov V, Edmans J, Conroy S, et al. Cost-effectiveness of a specialist geriatric medical intervention for frail older people discharged from acute medical units: economic evaluation in a two-centre randomised controlled trial (AMIGOS). PLoS One. 2015;10(5):e0121340.
Australian Bureau of Statistics. Life Tables, States, Territories and Australia. 2012–2014. http://www.abs.gov.au/ausstats/abs@.nsf/mf/3302.0.55.001. Accessed on 30 May 2016.
Australian Institute of Health and Welfare (AIHW). Residential aged care and Home Care. 2013–2014. http://www.aihw.gov.au/aged-care/residential-and-home-care-2013-14/admissions/. Accessed on 29 May 2016.
Klotzbuecher CM, Ross PD, Landsman PB, Abbott Iii TA, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721–39.
Australian Government, Department of Health. Aged care subsidies and supplements: new increased rates of payment from 1 July 2011. 2011. http://www.health.gov.au/internet/main/publishing.nsf/Content/37144F4345C.
Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99–103.
Acknowledgements
Funding provided by the NHMRC for the Centre for Research Excellence in Frailty and Healthy Ageing (ID 1102208) is acknowledged. Investigators of the NHMRC funded Frailty Intervention Trial (ID402791), in particular Nicola Fairhall, are acknowledged for completing the supporting clinical trial and economic evaluation alongside the clinical trial of the evaluated intervention. The data on which this research is based were drawn from several Australian longitudinal studies including the following: the Australian Diabetes, Obesity and Lifestyle (AusDiab) study, the Australian Longitudinal Study of Ageing (ALSA), the Australian Longitudinal Study of Women’s Health (ALSWH), the Blue Mountains Eye Study (BMES), the Canberra Longitudinal Study of Ageing (CLS), the Household, Income and Labour Dynamics in Australia study (HILDA), the Melbourne Longitudinal Studies on Healthy Ageing (MELSHA), the Personality And Total Health Through Life Study (PATH), and the Sydney Older Persons Study (SOPS). These studies were pooled and harmonised for the Dynamic Analyses to Optimise Ageing (DYNOPTA) Project. DYNOPTA was funded by an NHMRC Grant (ID 410215). All study researchers would like to thank the participants for volunteering their time to be involved in the respective studies. Details of all studies contributing data to DYNOPTA, including individual study leaders and funding sources, are available on the DYNOPTA website (http://dynopta.anu.edu.au). The findings and views reported in this paper are those of the authors and not those of the original studies or their respective funding agencies.
Author information
Authors and Affiliations
Contributions
Jonathan Karnon conceptualised the study, led the model development, implementation and analysis, and finalised the manuscript. Hossein Haji Ali Afzali co-supervised the development and implementation of the model and the literature reviews and reviewed and edited the manuscript. Gregorius Virgianto Arpuji Anggoro Putro, Phyu Win Thant, Ameline Dompok, Ingrid Cox, Owen Henry Chikhwaza, Xian Wang, Mercy Mukui Mwangangi and Matahari Farransahat contributed to the development and implementation of the model, undertook literature reviews to estimate model input parameters and drafted the first version of the manuscript. Ian Cameron advised on the interpretation of the clinical trial results and reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Ian Cameron was the lead investigator on the clinical trial of the evaluated frailty intervention. All other authors have no competing interests to declare.
Funding
Hossein Haji Ali Afzali is part-funded by the NHMRC Centre for Research Excellence in Frailty and Healthy Ageing (ID 1102208). No other funding was received for this study.
Availability of data and materials
The Frailty Cost-Effectiveness model, implemented in an Excel workbook, is available for use by external parties. Interested users are required to sign a License Application Form. No charge is made to academic organisations, but commercial organisations must pay an appropriate fee. In either case, it is a requirement to acknowledge the use of the Frailty Cost-Effectiveness model in any publications that make use of it, and to provide the corresponding author (JK) with the reference for each publication. It is not possible to provide access to the DYNOPTA dataset, as separate applications for data access are required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Karnon, J., Afzali, H.H.A., Putro, G.V.A.A. et al. A Cost-Effectiveness Model for Frail Older Persons: Development and Application to a Physiotherapy-Based Intervention. Appl Health Econ Health Policy 15, 635–645 (2017). https://doi.org/10.1007/s40258-017-0324-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0324-z