Abstract
Background
Current guidelines recommend direct-acting oral anticoagulants (DOACs) over warfarin in patients with atrial fibrillation (AF) and valvular heart disease (VHD) without a mechanical valve or moderate to severe mitral stenosis. However, real-world data to support the safety and efficacy of DOACs in this patient population are lacking.
Objective
Our objective was to assess the safety and effectiveness of DOACs in patients with AF and VHD.
Methods
This retrospective chart review evaluated patients aged ≥ 18 years with a diagnosis of AF and at least moderate VHD on echocardiogram. Patients were included if they received ≥ 1 month of DOAC therapy from December 2016 to December 2018. Patients were excluded if they received dual antiplatelet therapy or had additional indications for anticoagulation. The primary outcomes were incidence of stroke or systemic embolism (SSE) and major bleeding.
Results
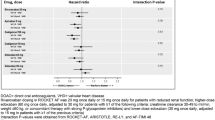
In total, 200 patients were included (disease type: aortic, n = 50; mitral, n = 50; tricuspid, n = 50; multivalve, n = 50). Most patients received apixaban (n = 133 [66.5%]) followed by rivaroxaban (n = 50 [25%]) and dabigatran (n = 17 [8.5%]). No patients received edoxaban. The mean CHA2DS2-VASc score was 4.25 and was similar among DOAC cohorts (p = 0.380). The overall SSE rate was 3.5% and was highest for dabigatran (n = 3 [17.6%]) compared with the other DOACs (apixaban, n = 1 [0.8%]; rivaroxaban, n = 3 [6%]; p = 0.001). Rates were similar among different valve types (aortic, n = 3 [6%]; mitral, n = 1 [2%]; tricuspid, n = 2 [4%]; multivalve, n = 1 [2%]; p = 0.653). The overall rate of major bleeding was 5.5% and did not differ among the DOACs (apixaban, n = 5 [3.8%]; rivaroxaban, n = 4 [8%]; dabigatran, n = 2 [11.8%]; p = 0.264) or valve type (aortic, n = 3 [6%]; mitral, n = 2 [4%]; tricuspid, n = 2 [4%]; multivalve, n = 4 [8%]; p = 0.787).
Conclusions
In patients with AF and VHD, rates of major bleeding were similar among the DOACs and valve types; however, more patients receiving dabigatran experienced SSE. Further studies are needed to validate these findings.
Similar content being viewed by others
References
January T, Wann L, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;139:1–49.
Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008;133:160S–98S.
Eliquis (apixaban) [prescribing information]. Princeton: Bristol-Myers Squibb; 2019. Available online from https://packageinserts.bms.com/pi/pi_eliquis.pdf. Accessed 8 Feb 2020.
Savaysa (edoxaban) [prescribing information]. Parsippany: Daiichi Sankyo; 2019. Available online from https://dsi.com/prescribing-information-portlet/getPIContent?productName=Savaysa&inline=true. Accessed 8 Feb 2020.
Pradaxa (dabigatran) [prescribing information. Ridegefield: Boeringer Ingelheim Pharmaceuticals Inc; 2019. Available online from https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Pradaxa/Pradaxa.pdf. Accessed 8 Feb 2020.
Xarelto (rivaroxaban) [prescribing information]. Titusville; Janssen Pharmaceuticals Inc; 2019. Available online from http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/XARELTO-pi.pdf. Accessed 8 Feb 2020.
Kannel WB, Wolf PA, Benjamin EJ, et al. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82:2N–9N.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8.
Pan K, Singer D, Ovbiagele B, et al. Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6:e005835.
Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Lip G, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–72.
Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess one-year risk of major bleeding in atrial fibrillation patients: the euro heart survey. Chest. 2010;138:1093–100.
Granger C, Alexander J, McMurray J, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Giugliano R, Ruff C, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Connolly S, Ezekowitz M, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Patel M, Mahaffey K, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Lip G, Keshishian A, Li X, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients. Stroke. 2018;49:2933–44.
Huang W, Singer D, Wu Y, et al. Association of intracranial hemorrhage risk with non-vitamin K antagonist oral anticoagulant use vs aspirin use. JAMA Neurol. 2018;75(12):1511–8.
Windecker S, Tijssen J, Giustino G, et al. Trial design: rivaroxaban for the prevention of major cardiovascular events after transcatheter aortic valve replacement: rationale and design of the GALILEO study. Am Heart J. 2017;184:81–7.
Cooper TP. Rivaroxaban (Xarelto): Increase in all-cause mortality, thromboembolic and bleeding events in patients after transcatheter aortic valve replacement in a prematurely stopped clinical trial (Dear Healthcare Professional letter dated October 3, 2018). Available online from http://www.hpra.ie/docs/default-source/default-document-library/important-safety-information---xarelto-(rivaroxaban)-(oct-2018).pdf?sfvrsn=0. Accessed 8 Feb 2020.
Acknowledgements
The author extends special thanks to Janki Patel, PharmD, for her contributions to this study. Dr. Patel contributed by screening patients for inclusion into the analysis.
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Schwarze is on the speaker’s bureau for Pfizer/BMS. Dr. Hampton, Dr. Tellor, Dr. Armbruster, and Dr. Theodos have no potential conflicts of interest that might be relevant to this work.
Rights and permissions
About this article
Cite this article
Hampton, M.L., Tellor, K.B., Armbruster, A.L. et al. Evaluation of the Safety and Effectiveness of Direct-Acting Oral Anticoagulants in Patients with Atrial Fibrillation and Coexisting Valvular Heart Disease. Am J Cardiovasc Drugs 20, 611–617 (2020). https://doi.org/10.1007/s40256-020-00398-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-020-00398-x