Abstract
Background
Levosimendan, a calcium sensitizer and potassium channel opener, has been demonstrated to improve myocardial function without increasing oxygen consumption and to show protective effects in other organs. Recently, a prospective, randomized controlled trial (RCT) revealed an association between levosimendan use and a possible increased risk of bleeding postoperatively. Levosimendan’s anti-platelet effects have been shown in in vitro studies. Current studies do not provide sufficient data to support a relation between perioperative levosimendan administration and increased bleeding risk.
Purpose
Our goal was to investigate the relation between perioperative levosimendan administration and increased bleeding risk using a meta-analysis study design.
Methods
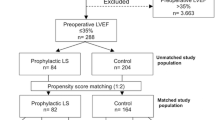
The PubMed, Ovid, EMBASE and Cochrane Library databases were searched for relevant RCTs before July 1, 2019. The outcome parameters included reoperation secondary to increased bleeding in the postoperative period, the amount of postoperative recorded blood loss, and the need for transfusion of packed red blood cells (RBCs) and other blood products.
Results
A total of 1160 patients in nine RCTs (576 in the levosimendan group and 584 in the control group) were included according to our inclusion criteria. Analysis showed that perioperative levosimendan administration neither increased the rate of reoperation secondary to bleeding nor increased the amount of postoperative chest tube drainage when compared with the control group. In terms of blood product transfusion, levosimendan did not influence the requirement for RBC transfusion, platelet transfusion nor fresh frozen plasma (FFP) transfusion. Levosimendan also did not shorten or prolong the aortic cross-clamp time or the cardiopulmonary bypass time.
Conclusion
The analyzed parameters, including reoperations due to bleeding, postoperative chest drainage and the requirement for blood products, revealed that levosimendan did not increase postoperative bleeding risk. More studies with a larger sample size are needed to address a more reliable conclusion due to study limitations.




Similar content being viewed by others
References
Papp Z, Edes I, Fruhwald S, De Hert SG, Salmenpera M, Leppikangas H, et al. Levosimendan: molecular mechanisms and clinical implications: consensus of experts on the mechanisms of action of levosimendan. Int J Cardiol. 2012;159(2):82–7. https://doi.org/10.1016/j.ijcard.2011.07.022.
Kivikko M, Antila S, Eha J, Lehtonen L, Pentikäinen PJ. Pharmacodynamics and safety of a new calcium sensitizer, levosimendan, and its metabolites during an extended infusion in patients with severe heart failure. J Clin Pharmacol. 2002;42(1):43–51.
Gödény I, Pollesello P, Édes I, Papp Z, Bagi Z. Levosimendan and its metabolite OR-1896 elicit KATP channel-dependent dilation in resistance arteries in vivo. Pharmacol Rep. 2013;65(5):1304–10.
Kandasamy A, Simon HA, Murthy P, Annadurai M, Ali MM, Ramanathan G. Comparison of levosimendan versus dobutamine in patients with moderate to severe left ventricular dysfunction undergoing off-pump coronary artery bypass grafting: a randomized prospective study. Ann Cardiac Anaesth. 2017;20(2):200–6. https://doi.org/10.4103/aca.ACA_195_16.
Lahtinen P, Pitkanen O, Musialowicz T. Levosimendan increases bleeding risk after heart valve surgery: a retrospective analysis of a randomized trial. J Cardiothorac Vasc Anesth. 2014;28(5):1238–42. https://doi.org/10.1053/j.jvca.2014.04.022.
Vivacqua A, Koch CG, Yousuf AM, Nowicki ER, Houghtaling PL, Blackstone EH, et al. Morbidity of bleeding after cardiac surgery: is it blood transfusion, reoperation for bleeding, or both? Ann Thorac Surg. 2011;91(6):1780–90. https://doi.org/10.1016/j.athoracsur.2011.03.105.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–805. https://doi.org/10.1177/0962280216669183.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Sahu MK, Das A, Malik V, Subramanian A, Singh SP, Hote M. Comparison of levosimendan and nitroglycerine in patients undergoing coronary artery bypass graft surgery. Ann Cardiac Anaesth. 2016;19(1):52–8. https://doi.org/10.4103/0971-9784.173020.
Anastasiadis K, Antonitsis P, Vranis K, Kleontas A, Asteriou C, Grosomanidis V, et al. Effectiveness of prophylactic levosimendan in patients with impaired left ventricular function undergoing coronary artery bypass grafting: a randomized pilot study. Interact Cardiovasc Thorac Surg. 2016;23(5):740–7. https://doi.org/10.1093/icvts/ivw213.
Landoni G, Lomivorotov VV, Alvaro G, Lobreglio R, Pisano A, Guarracino F, et al. Levosimendan for hemodynamic support after cardiac surgery. N Engl J Med. 2017;376(21):2021–31. https://doi.org/10.1056/NEJMoa1616325.
Baysal A, Yanartas M, Dogukan M, Gundogus N, Kocak T, Koksal C. Levosimendan improves renal outcome in cardiac surgery: a randomized trial. J Cardiothorac Vasc Anesth. 2014;28(3):586–94. https://doi.org/10.1053/j.jvca.2013.09.004.
Tritapepe L, De Santis V, Vitale D, Guarracino F, Pellegrini F, Pietropaoli P, et al. Levosimendan pre-treatment improves outcomes in patients undergoing coronary artery bypass graft surgery. Br J Anaesth. 2009;102(2):198–204. https://doi.org/10.1093/bja/aen367.
Lomivorotov VV, Boboshko VA, Efremov SM, Kornilov IA, Chernyavskiy AM, Lomivorotov VN, et al. Levosimendan versus an intra-aortic balloon pump in high-risk cardiac patients. J Cardiothorac Vasc Anesth. 2012;26(4):596–603. https://doi.org/10.1053/j.jvca.2011.09.006.
Malik V, Subramanian A, Hote M, Kiran U. Effect of levosimendan on diastolic function in patients undergoing coronary artery bypass grafting: a comparative study. J Cardiovasc Pharmacol. 2015;66(2):141–7. https://doi.org/10.1097/fjc.0000000000000256.
Kaptan K, Erinc K, Ifran A, Yildirim V, Uzun M, Beyan C, et al. Levosimendan has an inhibitory effect on platelet function. Am J Hematol. 2008;83(1):46–9.
Ambrus N, Szolnoky JA, Pollesello P, Kun A, Varró A, Papp JG, et al. Prolonged antispasmodic effect in isolated radial artery graft and pronounced platelet inhibition induced by the inodilator drug, levosimendan. Basic Clin Pharmacol Toxicol. 2012;110(3):269–74. https://doi.org/10.1111/j.1742-7843.2011.00801.x.
Plaschke K, Bent F, Rosenhagen C, Wagner S, Hofer S, Kopitz J. The inhibitory in vitro effect of high-dose levosimendan on platelet function may be mediated through its action as a phosphodiesterase inhibitor. Coron Artery Dis. 2012;23(3):215–20. https://doi.org/10.1097/MCA.0b013e32835167cc.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Executive summary: heart disease and stroke statistics–2016 Update: a report from the American Heart Association. Circulation. 2016;133(4):447–54. https://doi.org/10.1161/CIR.0000000000000366.
Emeklibas N, Kammerer I, Bach J, Sack F-U, Hellstern P. Preoperative hemostasis and its association with bleeding and blood component transfusion requirements in cardiopulmonary bypass surgery. Transfusion. 2013;53(6):1226–34. https://doi.org/10.1111/j.1537-2995.2012.03885.x.
Desborough M, Sandu R, Brunskill SJ, Doree C, Trivella M, Montedori A, et al. Fresh frozen plasma for cardiovascular surgery. Cochrane Database Syst Rev. 2015;7:cd007614. https://doi.org/10.1002/14651858.cd007614.pub2.
Koch CG, Li L, Duncan AI, Mihaljevic T, Loop FD, Starr NJ, et al. Transfusion in coronary artery bypass grafting is associated with reduced long-term survival. Ann Thorac Surg. 2006;81(5):1650–7.
Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;358(12):1229–39. https://doi.org/10.1056/NEJMoa070403.
Dorneles CDC, Bodanese LC, Guaragna JCVDC, Macagnan FE, Coelho JC, Borges AP, et al. The impact of blood transfusion on morbidity and mortality after cardiac surgery. Rev Bras Cirurg Cardiovasc. 2011;26(2):222–9.
Biancari F, Mikkola R, Heikkinen J, Lahtinen J, Airaksinen KE, Juvonen T. Estimating the risk of complications related to re-exploration for bleeding after adult cardiac surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg. 2012;41(1):50–5. https://doi.org/10.1016/j.ejcts.2011.04.023.
Kristensen KL, Rauer LJ, Mortensen PE, Kjeldsen BJ. Reoperation for bleeding in cardiac surgery. Interact Cardiovasc Thorac Surg. 2012;14(6):709–13. https://doi.org/10.1093/icvts/ivs050.
Frojd V, Jeppsson A. Reexploration for bleeding and its association with mortality after cardiac surgery. Ann Thorac Surg. 2016;102(1):109–17. https://doi.org/10.1016/j.athoracsur.
Ruel M, Chan V, Boodhwani M, McDonald B, Ni X, Gill G, et al. How detrimental is reexploration for bleeding after cardiac surgery? J Thorac Cardiovasc Surg. 2017;154(3):927–35. https://doi.org/10.1016/j.jtcvs.2016.04.097.
Salis S, Mazzanti VV, Merli G, Salvi L, Tedesco CC, Veglia F, et al. Cardiopulmonary bypass duration is an independent predictor of morbidity and mortality after cardiac surgery. J Cardiothorac Vasc Anesth. 2008;22(6):814–22. https://doi.org/10.1053/j.jvca.2008.08.004.
Iino K, Miyata H, Motomura N, Watanabe G, Tomita S, Takemura H, et al. prolonged cross-clamping during aortic valve replacement is an independent predictor of postoperative morbidity and mortality: analysis of the Japan Cardiovascular Surgery Database. Ann Thorac Surg. 2017;103(2):602–9. https://doi.org/10.1016/j.athoracsur.2016.06.060.
Haithcock BE, Shepard AD, Raman SB, Conrad MF, Pandurangi K, Fanous NH. Activation of fibrinolytic pathways is associated with duration of supraceliac aortic cross-clamping. J Vasc Surg. 2004;40(2):325–33. https://doi.org/10.1016/j.jvs.2004.04.015.
Zangrillo A, Biondi-Zoccai G, Mizzi A, Bruno G, Bignami E, Gerli C, et al. Levosimendan reduces cardiac troponin release after cardiac surgery: a meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth. 2009;23(4):474–8. https://doi.org/10.1053/j.jvca.2008.11.013.
Kivikko M, Kuoppamäki M, Soinne L, Sundberg S, Pohjanjousi P, Ellmen J, et al. Oral levosimendan increases cerebral blood flow velocities in patients with a history of stroke or transient ischemic attack: a pilot safety study. Curr Therap Res. 2015;77:46–51. https://doi.org/10.1016/j.curtheres.2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Integrated Thinking Research Fund of Cardiology (CIMF-Z-2016-23-1823), the National Natural Science Foundation of China (81873534, 81702194, 81600633, 81670411, 81570400, 81470560, 81471036), the key research and development program of Shandong Province (2018GSF118002, 2018GSF118017, 2017GSF18156), and the Natural Science Foundation of Shandong Province (ZR2017BH023).
Conflict of interest
Sen-bo Yan, Xiao-yan Wang, Guo-kai Shang, Zhi-hao Wang, Qi-ming Deng, Jia-wen Song, Wen-wen Sai, Ming Song, Ming Zhong and Wei Zhang declare that they have no potential conflicts of interest that might be relevant to the contents of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yan, Sb., Wang, Xy., Shang, Gk. et al. Impact of Perioperative Levosimendan Administration on Risk of Bleeding After Cardiac Surgery: A Meta-analysis of Randomized Controlled Trials. Am J Cardiovasc Drugs 20, 149–160 (2020). https://doi.org/10.1007/s40256-019-00372-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-019-00372-2