Abstract
Background
Australia has a high proportion of migrants, with an increasing migration rate from India. Type 2 diabetes is a chronic condition common amongst the Indian population. The decision to initiate and continue medication therapy (conventional or ayurvedic medicine) is complex and is influenced by a wide range of factors.
Objective
To determine preferences for conventional vs. ayurvedic medicines in Indian migrants with diabetes, and to identify the factors that may influence their preferences.
Methods
A discrete choice experiment was conducted with participants in Australia who were migrants from India with type 2 diabetes (n=141). Each respondent evaluated eight choice tasks consisting of eight attributes describing medicines and outcomes of medication taking; and were asked to choose ‘conventional’, or ‘ayurvedic’ medicine. A mixed multinomial logit model was used to estimate preferences.
Results
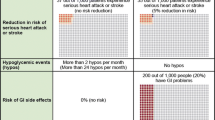
Overall, respondents’ preference to initiate a medicine was negative for both conventional (β=−2.33164, p<0.001) and ayurvedic medicines (β=−3.12181, p<0.001); however, significant heterogenicity was noted in participants’ preferences (SD: 2.33122, p<0.001). Six significant attributes were identified to influence preferences. In decreasing rank order: occurrence of hypoglycaemic events (relative importance, RI=24.33%), weight change (RI=20.00%), effectiveness of medicine (RI=17.91%), instructions to take with food (RI=17.05%), side effects (RI=13.20%) and formulation (RI=7.49%). Respondents preferred to initiate a medicine despite potential side effects.
Conclusions
There was a greater preference for conventional medicine, though neither were preferred. Medicine attributes and medication-taking outcomes influenced people’s preferences for an antidiabetic medicine. It is important to identify individual preferences during healthcare consultations to ensure optimal medication-taking.

Similar content being viewed by others
References
IDF Diabetes Atlas-8th edition. International Diabetes Federation. Available from http://www.diabetesatlas.org/. Accessed 26 Jan 2020.
Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besançon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: results from the International Diabetes Federation Diabetes Atlas. Diabet Res Clini Pract. 2020:108072. https://doi.org/10.1016/j.diabres.2020.108072.
Diabetes in Australia. Diabetes Australia, available from; https://www.diabetesaustralia.com.au/diabetes-in-australia. Accessed 26 Jan 2018.
Sainsbury E, Shi Y, Flack J, Colagiuri S. Burden of diabetes in Australia: it’s time for more action. Preliminary report. July 2018. Available from: https://www.sydney.edu.au/content/dam/corporate/documents/faculty-of-medicine-and-health/research/centres-institutes-groups/burden-of-diabetes-its-time-for-more-action-report.pdf. Accessed 16 Mar 2020.
Migration A. Australian Bureau of Statistics, Available from https://www.abs.gov.au/statistics/people/population/migration-australia/latest-release. Accessed 29 Sept 2020.
Centre for Epidemiology and Research. 2002–2005 Report on adult health by country of birth from the New South Wales population health survey. Sydney: New South Wales Department of Health; 2006.
New South Wales Health. The health of the People of New South Wales - Report of the Chief Health Officer 2008. Sydney: New South Wales Department of Health; Population Health Division; 2008.
Pandey MM, Rastogi S, Rawat AK. Indian traditional ayurvedic system of medicine and nutritional supplementation. Evid Based Complement Alternat Med. 2013;12. Article ID 376327. https://doi.org/10.1155/2013/376327.
Alfian SD, Sukandar H, Arisanti N, Abdulah R. Complementary and alternative medicine use decreases adherence to prescribed medication in diabetes patients. J Acupunct Meridian Stud. 2018;11(5):337. https://doi.org/10.1016/j.jams.2018.10.002.
Sridharan K. Mohan R, Ramaratnam S. Panneerselvam D. Ayurvedic treatments for diabetes mellitus. Cochrane Database Syst Rev. 2011;12:Art. No.: CD008288. https://doi.org/10.1002/14651858.CD008288.
Steyn M, Couchman L, Coombes G, Earle KA, Johnston A, Holt DW. A herbal treatment for type 2 diabetes adulterated with undisclosed drugs. Lancet. 2018;391(10138):2411. https://doi.org/10.1016/S0140-6736(18)31134-6.
Global Ayurveda S. 2018; Available from http://globalayurvedasummit.com/. Accessed 20 May 2020.
Porqueddu T. Herbal medicines for diabetes control among Indian and Pakistani migrants with diabetes. Anthropol Med. 2017;24(1):17–31. https://doi.org/10.1080/13648470.2016.1249338.
Lawton J, Ahmad N, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. BML. 2005;330(7502):1247. https://doi.org/10.1136/bmj.38460.642789.
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–35. https://doi.org/10.1161/CIRCULATIONAHA.108.768986.
Khan MU, Kohn M, Aslani P. The need for a paradigm shift in adherence research: the case of ADHD. Res Social Adm Pharm. 2019;15(3):318–20. https://doi.org/10.1016/j.sapharm.2018.04.033.
Krapek K, King K, Warren SS, George KG, Caputo DA, Mihelich K, Holst EM, Nichol MB, Shi SG, Livengood KB, Walden S. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. 2004;38(9):1357–62. https://doi.org/10.1345/aph.1D612.
Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299–307. https://doi.org/10.2147/PPA.S106821.
Arifulla M, John LJ, Sreedharan J, Muttappallymyalil J, Basha SA. Patients’ adherence to anti-diabetic medications in a Hospital at Ajman, UAE. Malaysian J Med Sci. 2014;21(1):44–9.
Abebaw M, Messele A, Hailu M, Zewdu F. Adherence and associated factors towards antidiabetic medication among type II diabetic patients on follow-up at University of Gondar Hospital, Northwest Ethiopia. Adv Nurs. 2016;8579157:2016. https://doi.org/10.1155/2016/8579157.
Bagonza J, Rutebemberwa E, Bazeyo W. Adherence to anti diabetic medication among patients with diabetes in eastern Uganda; a cross sectional study. BMC Health Serv Res. 2015;15:168. https://doi.org/10.1186/s12913-015-0820-5.
Huber CA, Reich O. Medication adherence in patients with diabetes mellitus: does physician drug dispensing enhance quality of care? Evidence from a large health claims database in Switzerland. Patient Prefer Adherence. 2016;10:1803–9. https://doi.org/10.2147/PPA.S115425.
Rwegerera GM, Moshomo T, Gaenamong M, Oyewo TA, Gollakota S, Mhimbira FA, et al. Antidiabetic medication adherence and associated factors among patients in Botswana; implications for the future. Alex J Med. 2018;54(2):103–9. https://doi.org/10.1016/j.ajme.2017.01.005.
Basu S, Garg S, Sharma N, Singh MM, Garg S. Adherence to self-care practices, glycemic status and influencing factors in diabetes patients in a tertiary care hospital in Delhi. World J Diabetes. 2018;9(5):72–9. https://doi.org/10.4239/wjd.v9.i5.72.
Dhippayom T, Krass I. Medication-taking behaviour in New South Wales Patients with Type 2 Diabetes: an observational study. Aust J Prim Health. 2015;21(4):429–37. https://doi.org/10.1071/PY14062.
Feher MD, Brazier J, Schaper N, Vega-Hernandez G, Nikolajsen A, Bøgelund M. Patients’ with type 2 diabetes willingness to pay for insulin therapy and clinical outcomes. BMJ Open Diabetes Res Care. 2016;4(1). https://doi.org/10.1136/bmjdrc-2016-000192.
Peyrot M, Barnett AH, Meneghini LF, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29:682–9. https://doi.org/10.1111/j.1464-5491.2012.03605.x.
Seston EM, Ashcroft DM, Griffiths CE. Balancing the benefits and risks of drug treatment: a stated-preference, discrete choice experiment with patients with psoriasis. Arch Dermatol. 2007;143(9):1175–9. https://doi.org/10.1001/archderm.143.9.1175.
Sinclair AJ, Alexander CM, Davies MJ, Zhao C, Mavros P. Factors associated with initiation of antihyperglycaemic medication in UK patients with newly diagnosed type 2 diabetes. BMC Endocr Disord. 2012;12(1):1–7. https://doi.org/10.1186/1472-6823-12-1.
Spoelstra JA, Stolk RP, Klungel OH, Erkens JA, Rutten GE, Leufkens HG. Initiation of glucose-lowering therapy in Type 2 diabetes mellitus patients in general practice. Diabet Med. 2004;21:896–900. https://doi.org/10.1111/j.1464-5491.2004.01273.x.
Mansfield C, Sikirica MV, Pugh A, Poulos CM, Unmuessig V, Morano R, Martin AA. Patient preferences for attributes of Type 2 Diabetes Mellitus medications in Germany and Spain: an online discrete-choice experiment survey. Diabetes Ther. 2017;8(6):1365–78. https://doi.org/10.1007/s13300-017-0326-8.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–9. https://doi.org/10.2337/dc14-2441.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2016 Executive Summary. Endocr Pract. 2016;22(1):84–113. https://doi.org/10.4158/EP151126.CS.
Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902. https://doi.org/10.1007/s40273-014-0170-x.
Toroski M, Kebriaeezadeh A, Esteghamati A, Karyani AK, Abbasian H, Nikfar S. Patient and physician preferences for type 2 diabetes medications: a systematic review. J Diabetes Metab Disord. 2019;18(2):643–56. https://doi.org/10.1007/s40200-019-00449-4.
Johnson FR, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, Bresnahan BW, Kanninen B, Bridges JF. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health. 2013;16(1):3–13. https://doi.org/10.1016/j.jval.2012.08.2223.
Hair JF, Black WC, Babin BJ, et al. Multivariate Data Analysis: International Edition. 6th ed. New Jersey: Pearson Prentice Hall; 2006.
ChoiceMetrics. Ngene 1.2.1 User Manual & Reference Guide, Australia. 2018.
Rose JM, Bliemer MCJ. Sample size requirements for stated choice experiments. Transportation. 2013;40:1021–41. https://doi.org/10.1007/s11116-013-9451-z.
Hensher DA, Greene WH. The mixed logit model: the state of practice. Transportation. 2003;30(2):133–76.
Khan MU. Factors influencing medication adherence in people with attention-deficit hyperactivity disorder and their parents/carers (Doctoral dissertation, University of Sydney). 2020.
Orme B. Interpreting the results of conjoint analysis. Getting Started with Conjoint Analyis: Strategies for Product Design and Pricing Research. 2010;2:77–88.
Greene WH. 1951- NLOGIT Reference Guide: Version 3.0. Plainview. NY: Econometric Software, Inc., 2002.
Mühlbacher A, Bethge S. What matters in type 2 diabetes mellitus oral treatment? A discrete choice experiment to evaluate patient preferences. Eur J Health Econom. 2016;17(9):1125–40. https://doi.org/10.1007/s10198-015-0750-5.
Aristides M, Weston AR, FitzGerald P, Reun CL, Maniadakis N. Patient preference and willingness-to-pay for Humalog mix 25 relative to humulin 30/70: a multicountry application of a discrete choice experiment. Value Health. 2004;7(4):442–54. https://doi.org/10.1111/j.1524-4733.2004.74007.x.
Gelhorn H, Stringer S, Brooks A, Thompson C, Monz B, Boye K, et al. Preferences for medication attributes among patients with type 2 diabetes mellitus in the UK. Diabetes Obes Metab. 2013;15(9):802–9. https://doi.org/10.1111/dom.12091.
Janssen EM, Longo DR, Bardsley JK, Bridges JFP. Education and patient preferences for treating type 2 diabetes: a stratified discrete-choice experiment. Patient Prefer Adherence. 2017;11:1729–36. https://doi.org/10.2147/PPA.S139471.
Fifer S, Rose J, Hamrosi KK, Swain D. Valuing injection frequency and other attributes of type 2 diabetes treatments in Australia: a discrete choice experiment. BMC Health Serv Res. 2018;18(1):1–1. https://doi.org/10.1186/s12913-018-3484-0.
Mohamed A, Zhang J, Johnson F, Malvoti E, Ostgren C, Parhofer K. The avoidance of weight gain is important for oral type 2 diabetes treatments in Sweden and Germany: a patient preference study. Value Health. 2013;39(5):397–403. https://doi.org/10.1016/j.diabet.2013.06.001.
Hauber AB, Mohamed AF, Johnson FR, Falvey H. Treatment preferences and medication adherence of people with Type 2 diabetes using oral glucose-lowering agents. Diabetic Med. 2009;26(4):416–24. https://doi.org/10.1111/j.1464-5491.2009.02696.x.
Polster M, Zanutto E, McDonald S, Conner C, Hammer M. A comparison of preferences for two GLP-1 products liraglutide and exenatide for the treatment of type 2 diabetes. J Med Econ. 2010;13(4):655–61. https://doi.org/10.3111/13696998.2010.529377.
American Diabetes Association. Glycemic targets. Diabetes Care. 2016;39(Suppl 1):39–46.
Bundesa¨rztekammer, Bundesvereinigung K: Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften, et al, editors: Nationale Versorgungsleitlinie: Therapie des Typ-2-Diabetes. Kurzfassung. Berlin. 2013.
Ahmad A. Medication-taking behaviour and treatment preferences of Indian migrants with type 2 diabetes in Australia. Doctoral dissertation, The University of Sydney; 2021.
Ranade M, Mudgalkar N. A simple dietary addition of fenugreek seed leads to the reduction in blood glucose levels: A parallel group, randomized single-blind trial. Ayu. 2017;38(1-2):24. https://doi.org/10.4103/ayu.AYU_20915.
Fenugreek, Diabetes, Diabetes UK. Available from, https://www.diabetes.co.uk/natural-therapies/fenugreek.html. Accessed 18 Dec 2020.
García-Pérez LE, Alvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4(2):175–94. https://doi.org/10.1007/s13300-013-0034-y.
Acknowledgements
Sincere gratitude to all participants and Indian associations/organizations/new papers for their assistance in data collection throughout this project.
Author information
Authors and Affiliations
Contributions
AA and PA designed the research study. AA analysed all the data and wrote the first draft of the manuscript. MUK and PA contributed significantly to all drafts of the manuscript and its final version. All authors have read and agreed with the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval to conduct the research project was received from the Human Research Ethics Committee of university on 8 July 2020 (Project No.:2020/321). The survey was performed in compliance with the approved research protocol. Participation in the study was completely voluntary. As an online questionnaire was used, the respondents were in control of completing and submitting the questionnaire. The completion of the online survey was taken as evidence of consent to participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmad, A., Khan, M.U. & Aslani, P. Patient preferences for the treatment of type 2 diabetes in Australia: a discrete choice experiment. J Diabetes Metab Disord 21, 229–240 (2022). https://doi.org/10.1007/s40200-021-00962-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00962-5