Abstract
Purpose
The purpose of the study is to assess the effect of probiotic supplementation on gut microbiota and insulin resistance in adolescents with severe obesity.
Methods
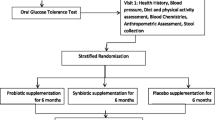
Through a randomized, double blind, placebo-controlled, 12-week pilot clinical trial, 15 adolescents with severe obesity received either an oral probiotic ‘Visbiome®’ (n = 8) or placebo (n = 7). Anthropometry, fasting glucose, insulin, hs-CRP and stool for microbiome and calprotectin were collected at baseline (week 0) and 12 weeks after intervention.
Results
Among completers (n = 4 in each of the two groups), mean change in fasting glucose was significantly lower in the probiotic group (0 ± 4 mg/dL) as compared to the placebo group (6.3 ± 1.7 mg/dL) (p = 0.028). Gut microbial Firmicutes to Bacteroidetes (F/B) ratio had a greater decline from week 0 to week 12 in the probiotic group (mean 17.7 ± 25.1 to 2.39 ± 2.0, respectively) but was not statistically significant (p = 0.06) as compared to in the placebo group (mean 12.8 ± 18.2 to 6.9 ± 5.61, respectively) (p = 0.89). Weight and BMI (mean ± SD) trended to remain stable in the treatment group (-1.07 ± 6.1 kg and -0.3 ± 2.2 kg/m2 respectively) as compared to the placebo group (3.9 ± 5.1 kg, 1.0 ± 1.6 kg/m2) but was not significant (p = 0.12 for weight and 0.38 for BMI). No significant change in the fasting insulin, HOMA-IR, or serum and stool inflammatory markers were noted between the two groups (p > 0.05). One participant in the treatment arm reported adverse effects of gastrointestinal intolerance.
Conclusion
Probiotic therapy with Visbiome® may improve the fasting glucose and possibly decrease the gut microbial F/B ratio as compared to placebo in adolescents with severe obesity. Future larger studies are required to confirm these findings.
U.S. Clinical Trial Registry number: NCT03109587





Similar content being viewed by others
Data availability
Data and materials are available upon request.
Code availability
Not applicable.
References
Dabelea D, Mayer-Davis EJ, Saydah S, Imperatore G, Linder B, Divers J, Bell R, Badaru A, Talton JW, Crume T, Liese AD, Merchant AT, Lawrence JM, Reynolds K, Dolan L, Liu LL, Hamman RF; Search for diabetes in youth study. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–86. https://doi.org/10.1001/jama.2014.3201.
RISE Consortium. Impact of insulin and metformin versus metformin alone on β-cell function in youth with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care. 2018;41(8):1717- 1725. https://doi.org/10.2337/dc18-0787.
Khan MT, Nieuwdorp M, Bäckhed F. Microbial modulation of insulin sensitivity. Cell Metab. 2014;20(5):753–60. https://doi.org/10.1016/j.cmet.2014.07.006.
Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto JM, Kennedy S, Leonard P, Li J, Burgdorf K, Grarup N, Jørgensen T, Brandslund I, Nielsen HB, Juncker AS, Bertalan M, Levenez F, Pons N, Rasmussen S, Sunagawa S, Tap J, Tims S, Zoetendal EG, Brunak S, Clément K, Doré J, Kleerebezem M, Kristiansen K, Renault P, Sicheritz-Ponten T, de Vos WM, Zucker JD, Raes J, Hansen T; MetaHIT consortium, Bork P, Wang J, Ehrlich SD, Pedersen O. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–6. https://doi.org/10.1038/nature12506.
Vallianou N, Stratigou T, Christodoulatos GS, Dalamaga M. Understanding the Role of the Gut Microbiome and Microbial Metabolites in Obesity and Obesity-Associated Metabolic Disorders: Current Evidence and Perspectives. Curr Obes Rep. 2019;8(3):317–32. https://doi.org/10.1007/s13679-019-00352-2.
Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444(7122):1022–3. https://doi.org/10.1038/4441022a.
Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, Sogin ML, Jones WJ, Roe BA, Affourtit JP, Egholm M, Henrissat B, Heath AC, Knight R, Gordon JI. A core gut microbiome in obese and lean twins. Nature. 2009;457(7228):480–4. https://doi.org/10.1038/nature07540.
Indiani CMDSP, Rizzardi KF, Castelo PM, Ferraz LFC, Darrieux M, Parisotto TM. Childhood Obesity and Firmicutes/Bacteroidetes Ratio in the Gut Microbiota: A Systematic Review. Child Obes. 2018;14(8):501–9. https://doi.org/10.1089/chi.2018.0040.
Cox AJ, West NP, Cripps AW. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol. 2015;3(3):207–15. https://doi.org/10.1016/S2213-8587(14)70134-2.
Utzschneider KM, Kratz M, Damman CJ, Hullar M. Mechanisms linking the gut microbiome and glucose metabolism. J Clin Endocrinol Metab. 2016;101(4):1445–54. Epub 2016 Mar 3. Erratum in: J Clin Endocrinol Metab. 2016;101(6):2622. https://doi.org/10.1210/jc.2015-4251.
Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, Derrien M, Druesne A, Van HylckamaVlieg JE, Bloks VW, Groen AK, Heilig HG, Zoetendal EG, Stroes ES, de Vos WM, Hoekstra JB, Nieuwdorp M. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143(4):913-6.e7. https://doi.org/10.1053/j.gastro.2012.06.031.
Wang J, Tang H, Zhang C, Zhao Y, Derrien M, Rocher E, van-HylckamaVlieg J.E., Strissel K., Zhao L., Obin M., Shen J, . Modulation of gut microbiota during probiotic-mediated attenuation of metabolic syndrome in high fat diet-fed mice. ISME J. 2015;9:1. https://doi.org/10.1038/ismej.2014.99.
Bagarolli RA, Tobar N, Oliveira AG, Araújo TG, Carvalho BM, Rocha GZ, Vecina JF, Calisto K, Guadagnini D, Prada PO, Santos A, Saad STO, Saad MJA. Probiotics modulate gut microbiota and improve insulin sensitivity in DIO mice. J Nutr Biochem. 2017;50:16–25. https://doi.org/10.1016/j.jnutbio.2017.08.006.
Kassaian N, Feizi A, Aminorroaya A, Amini M. Probiotic and synbiotic supplementation could improve metabolic syndrome in prediabetic adults: A randomized controlled trial. Diabetes Metab Syndr. 2019;13(5):2991–6. https://doi.org/10.1016/j.dsx.2018.07.016.
Kassaian N, Feizi A, Aminorroaya A, Jafari P, Ebrahimi MT, Amini M. The effects of probiotics and synbiotic supplementation on glucose and insulin metabolism in adults with prediabetes: a double-blind randomized clinical trial. Acta Diabetol. 2018;55(10):1019–28. https://doi.org/10.1007/s00592-018-1175-2.
Kobyliak N, Falalyeyeva T, Mykhalchyshyn G, Kyriienko D, Komissarenko I. Effect of alive probiotic on insulin resistance in type 2 diabetes patients: Randomized clinical trial. Diabetes Metab Syndr. 2018;12(5):617–24. https://doi.org/10.1016/j.dsx.2018.04.015.DOI:10.1016/j.dsx.2018.04.015.
Nagata S, Chiba Y, Wang C, Yamashiro Y. The effects of the Lactobacillus casei strain on obesity in children: a pilot study. Benef Microbes. 2017;8(4):535–43. https://doi.org/10.3920/BM2016.0170.
Gøbel RJ, Larsen N, Jakobsen M, Mølgaard C, Michaelsen KF. Probiotics to adolescents with obesity: effects on inflammation and metabolic syndrome. J Pediatr Gastroenterol Nutr. 2012;55(6):673–8. https://doi.org/10.1097/MPG.0b013e318263066c.
Larsen N, Vogensen FK, Gøbel RJ, Michaelsen KF, Forssten SD, Lahtinen SJ, Jakobsen M. Effect of Lactobacillus salivarius Ls-33 on fecal microbiota in obese adolescents. Clin Nutr. 2013;32(6):935–40. https://doi.org/10.1016/j.clnu.2013.02.007.
Vajro P, Mandato C, Licenziati MR, Franzese A, Vitale DF, Lenta S, Caropreso M, Vallone G, Meli R. Effects of Lactobacillus rhamnosus strain GG in pediatric obesity-related liver disease. J Pediatr Gastroenterol Nutr. 2011;52(6):740–3. https://doi.org/10.1097/MPG.0b013e31821f9b85.
Alisi A, Bedogni G, Baviera G, Giorgio V, Porro E, Paris C, Giammaria P, Reali L, Anania F, Nobili V. Randomised clinical trial: The beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2014;39(11):1276–85. https://doi.org/10.1111/apt.12758.
Famouri F, Shariat Z, Hashemipour M, Keikha M, Kelishadi R. Effects of Probiotics on Nonalcoholic Fatty Liver Disease in Obese Children and Adolescents. J Pediatr Gastroenterol Nutr. 2017;64(3):413–7. https://doi.org/10.1097/MPG.0000000000001422.
Ipar N, Aydogdu SD, Yildirim GK, Inal M, Gies I, Vandenplas Y, Dinleyici EC. Effects of synbiotic on anthropometry, lipid profile and oxidative stress in obese children. Benef Microbes. 2015;6(6):775–82. https://doi.org/10.3920/BM2015.0011.
Safavi M, Farajian S, Kelishadi R, Mirlohi M, Hashemipour M. The effects of synbiotic supplementation on some cardio-metabolic risk factors in overweight and obese children: a randomized triple-masked controlled trial. Int J Food Sci Nutr. 2013;64(6):687–93. https://doi.org/10.3109/09637486.2013.775224.
Stefanaki C, Michos A, Mastorakos G, Mantzou A, Landis G, Zosi P, Bacopoulou F. Probiotics in Adolescent Prediabetes: A Pilot RCT on Glycemic Control and Intestinal Bacteriome. J Clin Med. 2019;8(10):1743. https://doi.org/10.3390/jcm8101743.
Jones RB, Alderete TL, Martin AA, Geary BA, Hwang DH, Palmer SL, Goran MI. Probiotic supplementation increases obesity with no detectable effects on liver fat or gut microbiota in obese Hispanic adolescents: a 16-week, randomized, placebo-controlled trial. Pediatr Obes. 2018;13(11):705–14. https://doi.org/10.1111/ijpo.12273.
Honda K, Moto M, Uchida N, He F, Hashizume N. Anti-diabetic effects of lactic acid bacteria in normal and type 2 diabetic mice. J Clin Biochem Nutr. 2012;51:96. https://doi.org/10.3164/jcbn.11-07.
Tabuchi M, Ozaki M, Tamura A, Tabuchi M, Ozaki M, Tamura A, Yamada N, Ishida T, Hosoda M, Hosono A. Antidiabetic effect of Lactobacillus GG in streptozotocin-induced diabetic rats. Biosci Biotechnol Biochem. 2003;67:1421. https://doi.org/10.1271/bbb.67.1421.
Falony G, Vlachou A, Verbrugghe K, De Vuyst L. Cross-feeding between Bifidobacterium longum BB536 and acetate-converting, butyrate-producing colon bacteria during growth on oligofructose. Appl Environ Microbiol. 2006;72:7835. https://doi.org/10.1128/AEM.01296-06.
Walker AW, Duncan SH, McWilliam Leitch EC, Walker AW, Duncan SH, McWilliam Leitch EC, Child MW, Flint HJ. pH and peptide supply can radically alter bacterial populations and short-chain fatty acid ratios within microbial communities from the human colon. Appl Environ Microbiol. 2005;71:3692. https://doi.org/10.1128/AEM.71.7.3692-3700.2005.
Yadav H, Lee JH, Lloyd J, Walter P, Rane SG. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem. 2013;288(35):25088–97. https://doi.org/10.1074/jbc.M113.452516.
Jafarnejad S, Saremi S, Jafarnejad F, Arab A. Effects of a Multispecies probiotic mixture on glycemic control and inflammatory status in women with gestational diabetes: A randomized controlled clinical trial. J Nutr Metab. 2016;2016:5190846. https://doi.org/10.1155/2016/5190846.
Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999-2016 [published correction appears in Pediatrics. 2018 Sep;142(3)]. Pediatrics. 2018;141(3):e20173459. https://doi.org/10.1542/peds.2017-3459.
Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–712. https://doi.org/10.1161/CIR.0b013e3182a5cfb3.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190.
Poretsky R, Rodriguez-R LM, Luo C, Tsementzi D, Konstantinidis KT. Strengths and limitations of 16S rRNA gene amplicon sequencing in revealing temporal microbial community dynamics. PLoS ONE. 2014;9: e93827. https://doi.org/10.1371/journal.pone.0093827.
Paulson JN, Stine OC, Bravo HC, Pop M. Differential abundance analysis for microbial marker-gene surveys. Nat Methods. 2013;10(12):1200–2. https://doi.org/10.1038/nmeth.2658.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9. https://doi.org/10.1007/BF00280883.
Suau A, Bonnet R, Sutren M, Godon JJ, Gibson GR, Collins MD, Doré J. Direct analysis of genes encoding 16S rRNA from complex communities reveals many novel molecular species within the human gut. Appl Environ Microbiol. 1999;65(11):4799–807. https://doi.org/10.1128/AEM.65.11.4799-4807.1999.
Wang X, Heazlewood SP, Krause DO, Florin TH. Molecular characterization of the microbial species that colonize human ileal and colonic mucosa by using 16S rDNA sequence analysis. J Appl Microbiol. 2003;95(3):508–20. https://doi.org/10.1046/j.1365-2672.2003.02005.x.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. https://doi.org/10.1038/nature05414.
Graessler J, Qin Y, Zhong H, Zhang J, Licinio J, Wong ML, Xu A, Chavakis T, Bornstein AB, Ehrhart-Bornstein M, Lamounier-Zepter V, Lohmann T, Wolf T, Bornstein SR. Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J. 2013;13(6):514–22. https://doi.org/10.1038/tpj.2012.43.
Schwiertz A, Taras D, Schäfer K, Beijer S, Bos NA, Donus C, Hardt PD. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring). 2010;18(1):190–5. https://doi.org/10.1038/oby.2009.167.
Collins CE, Warren J, Neve M, McCoy P, Stokes BJ. Measuring effectiveness of dietetic interventions in child obesity: A systematic review of randomized trials. Arch Pediatr Adolesc Med. 2006;160:906–22. https://doi.org/10.1001/archpedi.160.9.906.
Shoemaker A, Cheng P, Gal RL, Kollman C, Tamborlane WV, Klingensmith GJ, Clements MA, Hannon TS, Heptulla R, Less J, Wood J; for the Pediatric Diabetes Consortium. Predictors of Loss to Follow-Up among Children with Type 2 Diabetes. Horm Res Paediatr. 2017;87(6):377–384. https://doi.org/10.1159/000475595.
Acknowledgements
We acknowledge the efforts of Cordelia Franklin and Sue Kearns in helping participants schedule for study visits.
Funding
This research was funded by the Office of Research Central, University of Washington (grant A118785 Royalty Research Fund, Pilot Study of Synbiotics in Pre-diabetic Adolescents).
Author information
Authors and Affiliations
Contributions
Conceptualization, Christian L. Roth, Christiane Hampe and William R. DePaolo; Data curation, Arushi Verma and Maria T. Nelson; Formal analysis, Arushi Verma, Maria T. Nelson and Christian L. Roth; Funding acquisition, Arushi Verma, William R. DePaolo, Christiane Hampe and Christian L. Roth; Investigation, Arushi Verma, William R. DePaolo and Christian L. Roth; Methodology, Arushi Verma and Christian L. Roth; Project administration, Arushi Verma and Christian L. Roth; Resources, William R. DePaolo, Christiane Hampe and Christian L. Roth; Software, Maria T. Nelson; Supervision, Christian L. Roth; Validation, William R. DePaolo and Christian L. Roth; Visualization, Arushi Verma, William R. DePaolo and Christian L. Roth; Writing – original draft, Arushi Verma; Writing – review & editing, Arushi Verma, Maria T. Nelson, William R. DePaolo and Christian L. Roth.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional IRB (Seattle Children’s IRB).
Consent to participate
Informed consent and assent was obtained by all participants of the study.
Consent for publication
All authors consent for publication.
Conflict of interest/Competing interest
The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Verma, A., Nelson, M.T., DePaolo, W.R. et al. A randomized double-blind placebo controlled pilot study of probiotics in adolescents with severe obesity. J Diabetes Metab Disord 20, 1289–1300 (2021). https://doi.org/10.1007/s40200-021-00855-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00855-7