Abstract
Purpose of Review
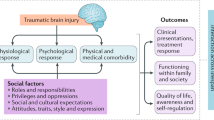
The goals of the report are to integrate recent and key foundational gender- and sex-related, post-traumatic brain injury (TBI) literature across several research domains, to highlight need for increased cross-field communication using an integrative biopsychosocial research model, and to provide recommendations for further research approaches and foci.
Recent Findings
Recent findings of TBI studies addressing gender and/or biological sex provide evidence of women’s unique risks for injury, significant differences in severity, type, and number of post-TBI symptoms reported by women vs. men, and complex, interactive molecular, genetic, psychosocial, and physiological factors that contribute differently to TBI outcomes for the sexes.
Summary
Brain injury researchers, following years of failed clinical trials and mixed findings, are adopting new methods for more precisely characterizing differing effects of sex on both responses to TBI and recovery trajectories as well as underlying causes of these differences. New approaches include analysis of large data sets, use of sophisticated statistical models, more consistent exploration of sex-specific effects of TBI in more TBI study domains, and use of more precise measures. Increased cross-field communication and collaboration, stratification by sex, and increased adoption of these approaches are recommended to help advance understanding of TBI and move us closer to treatment development.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Stein DG. What have we learned about treating brain injuries from the repeated failures of clinical trials. Featured Session, American Congress of Rehabilitation Annual Conference, October 28, 2017, Atlanta, GA. This paper provides an overview of Phase II and III TBI treatment trials and focuses on need to reevaluate and change methods in this gender and TBI study domain.
• Stein DG. Embracing failure; What the Phase III progesterone studies can teach about TBI clinical trials. Brain Inj. 2015;29(11):1259–72 This reference asks investigators to consider reasons for failed clinical trials and need to for new approaches to gender/TBI research.
Niemeier JP, Marwitz JH, Walker WC, Davis LC, Bushnik T, Ripley DL, et al. Are there cognitive and neurobehavioural correlates of hormonal neuroprotection for women after TBI? Nuropsychol Rehabil. 2013;23(3):363–82.
Davis DP, Douglas DJ, Smith W, Sise MJ, Vilke GM, Holbrook TL, et al. Traumatic brain injury outcomes in pre-and post-menopausal females versus age-matched males. J Neurotrauma. 2006;23:140–8.
Yeung JH, Mikocka-Walus AA, Cameron PA, Poon WS, Ho HF, Chang A, et al. Protection from traumatic brain injury in hormonally active women vs. men of a similar age: a retrospective international study. Arch Surg. 2011;146:436–42.
Stein DG. Brain damage, sex hormones and recovery: a new role for progesterone and estrogen? Trends Neurosci. 2001;24:386–91.
Stein DG, Wright DW. Progesterone in the clinical treatment of acute traumatic brain injury. Expert Opin Investig Drugs. 2010;19:847–57.
Stein DG, Wright DW, Kellermann AL. Does progesterone have neuroprotective properties? Ann Emerg Med. 2008;51:164–72.
Wagner AK, Willard LA, Kline AE, Wenger MK, Bolinger BD, Ren D, et al. Evaluation of estrous cycle stage and gender on behavioral outcome after experimental traumatic brain injury. Brain Res. 1998;2004:113–21.
Pettus EH, Wright DW, Stein DG, Hoffman SW. Progesterone treatment inhibits the inflammatory agents that accompany traumatic brain injury. Brain Res. 2005;1049:112–9.
Gibson CL, Gray IJ, Bath PM, Murphy SP. Progesterone for the treatment of experimental brain injury: a systematic review. Brain. 2008;131:318–28.
Kokiko ON, Murashov AK, Hoane MR. Administration of raloxifene reduces sensorimotor and working memory deficits following traumatic brain injury. Behav Brain Res. 2006;170:233–40.
Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, et al. Pro-TECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49:391–402 402e1-2.
Xiao G, Wei J, Yan W, Wang W, Lu. Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: A randomized controlled trial. Crit Care. 2009;12:R61.
Stein DG. A clinical/translational perspective: can a developmental hormone play a role in the treatment of traumatic brain injury? Horm Behav. 2013;63:291–300.
• Skolnick BE, Maas AI, Narayan RK, van der Hoop RG, MacAllister T, Ward JD, et al. SYNAPSE: Trial Investigators A clinical trial of progesterone for severe traumatic brain injury. N Engl J Med. 2014;371:2467–76 This paper describes results of a trial of progesterone for persons with severe TBI and the lack of evidence of efficacy.
• Wright DW, Yeatts SD, Silbergleit R, Palesch YY, Hertzberg VS, Frankel M, et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371:2457–66 The results of a failed trial of progesterone for acute TBI are described.
Berry C, Ley EJ, Tillou A, Cryer G, Margulies DR, Salim A. The effect of gender on patients with moderate to severe head injuries. J Trauma. 2009;67:950–3.
Leitgeb J, Mauritz W, Brazinova A, Janciak I, Majdan M, Wilbacher I, et al. Effects of gender on outcomes after traumatic brain injury. J Trauma. 2011;71:1620–6.
Bounds TA, Schopp L, Johnstone B, Under C, Goldman H. Gender differences in a sample of vocational rehabilitation clients with TBI. NeuroRehabil. 2003;18:189–96.
• Cuthbert JP, Pretz CR, Bushnik T, Fraser RT, Hart T, Kolakowsky-Hayner SA, et al. Ten-year employment patterns of working age individuals after moderate to severe traumatic brain injury: A National Institute on Disability and Rehabilitation Research Traumatic Brain Injury Model Systems Study. Arch Phys Med Rehabil. 2015;96:2128–36 This work provides large data set analyses and findings related to outcomes after TBI showing sex differences.
Farace E, Alves WM. Do women fare worse? A metanalysis of gender differences in outcome after traumatic brain injury. Neursurg Foc. 2000;8:e6.
Goranson TE, Graves RE, Allison D, Freniere RL. Community integration following multidisciplinary rehabilitation for traumatic brain injury. Brain Inj. 2003;17:759–74.
Graham JE, Radice-Neumann DM, Reistetter TA, Hammond FM, Dijkers M, Granger CV. Influence of sex and age on inpatient rehabilitation outcomes among older adults with traumatic brain injury. Arch Phys Med Rehabil. 2010;91:43–50.
• Howrey BT, Graham JE, Pappadis MR, Granger CV, Ottenbacher KJ. Trajectories of functional change after inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2017;98:1606–13 The paper reports findings showing sex and gender differences in recovery.
Liossi C, Wood R. Gender as a moderator of cognitive and affective outcome after traumatic brain injury. J Neuropsychiatr Clin Neurosci. 2009;21:43–51.
Moore DW, Ashman TA, Cantor JB, Krinick RJ, Spielman LA. Does gender influence cognitive outcome after traumatic brain injury? Neuropsychol Rehabil. 2010;20:340–54.
Niemeier JP, Marwitz JH, Lesher K, Walker WC, Bushnik T. Gender differences in executive functions following traumatic brain injury. Neuropsychol Rehabil. 2007;17:293–313.
Niemeier JP, Perrin PB, Holcomb MG, Rolston CD, Artman LK, Lu J, et al. Gender differences in awareness and outcomes during acute traumatic brain injury recovery. J Women's Health. 2014;23:573–80.
Ponsford JL, Myles PS, Cooper DJ, Medermott FT, Murray LJ, Laidlaw J, et al. Gender differences in outcome in patients with hypotension and severe traumatic brain injury. Brain Inj. 2008;39:67–76.
Drapeau A, Boyer R, Lesage A. The influence of social anchorage on the gender differences in the use of mental health service. J Behav Health Serv Res. 2009;36:372–84.
Munro CA, Winicki JM, Schretlen DF, Gower EW, Turano KA, Munoz B, et al. Sex differences in cognition in healthy elderly individuals. Neuropsychol Dev Cogn B Aging. 2012;19:739–68.
Murre JM, Janssen SM, Rouw R, Meeter M. The rise and fall of immediate and delayed memory for verbal and visuospatial information from late childhood to late adulthood. Acta Psychol. 2013;142:96–107.
Redpath S, Williams W, Hanna D, Linden M, Yates P, Harris A. Healthcare professionals; attitudes towards traumatic brain injury (TBI): the influence of profession, experience, etiology and blame on prejudice towards survivors of brain injury. Brain Inj. 2010;24:802–11.
Engel de Abreu PM, Puglisi JL, Crus-Santos A, Befi-Lopes DM, Martin R. Effects of impoverished environmental conditions on working memory performance. Memory. 2014;22:323–31.
• Flanagan SR. Invited commentary on ‘Centers for Disease Control and Prevention Report to Congress: Traumatic brain injury in the United Stated: Epidemiology and Rehabilitation.’. Arch Phys Med Rehabil. 2015;96:1753–5 This paper summarizes the conclusions of a Congressional committee of experts that showed critical continued need to find treatments and address gaps in care for people with TBI and their families.
• Davanzo JR, Sieg EP, Timmons SD. Management of traumatic brain injury. Surg Clin North Am. 2017;97:1237–53 This work provides an overview of heterogeneity of TBI and barriers to finding treatments.
Saban KL, Hogan NS, Hogan TP, Pape TL. He looks normal but…challenges of family caregivers of veterans diagnosed with a traumatic brain injury. Rehabil Nurs. 2015;40:277–85.
• Wade DR, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. 2017;31:995–1004 This editorial covers the need to apply the biopsychosocial model to healthcare management to improve outcomes.
Wagner AK. TBI Rehabilomics research: An Exemplar of a biomarker-based approach to precision care for populations with disability. Curr Neurol Neurosci Rep. 2017;17:84.
Xiong C, Martin T, Sravanapudi M, Colantonio A, Mollayeva T. Factors associated with return to work in men and women with work-related traumatic brain injury. Disabil Health J. 2016;9:439–48.
• Richardson C, McKay A, Ponsford JL. The trajectory of awareness across the first year after traumatic brain injury; the role of biopsychosocial factors. Brain Inj. 2014;28:1711–20 This study illustrates the value of applying a biopsychosocial model to understand brain injury complexities and for identification of gender and biological sex differences that could impact treatment.
Colantonio A. Sex, gender, and traumatic brain injury: a commentary. Arch Phys Med Rehabil. 2016;97:51–4.
National Institute of Women’s Health, National Institutes of Health. https://orwh.od.nih.gov/sex-gender/ retrieved October 30, 2018.
Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research? JAMA. 2016;316:1863–4.
•• National Institutes of Health. https://www.ncbi.nlm.nih.gov/books/NBK19934/ retrieved October 21 2018. This is the announcement of NIH guidance on investigator and grant applicant attention to sex as a biological variable in research.
• Amoroso T, Iverson KM. Acknowledging the risk for traumatic brain injury in women Veterans. J Nerv Ment Dis. 2017;205:318–23 This paper brings attention to epidemiology of TBI and women veterans as well as describes unique risks for TBI and challenges of women Veterans with TBI.
• Iverson KM, Sayer NA, Meterko M, Stolzmann K, Suri P, Gormley K, et al. Intimate partner violence among female OEF/OIF/OND veterans who were evaluated for traumatic brain injury in the Veterans Health Administration: A preliminary investigation. J Interpers Violence. 2017;1:8862605. https://doi.org/10.1177/088626051770491This article importantly draws attention to unique risks for women veterans for sustaining a TBI from intimate partner violence.
• Lippa SM, Brickell TA, Bailie JM, French LM, Kennedy JE, Lange RT. Postconcussion symptom reporting after mild traumatic brain injury in female service members: Impact of gender, posttraumatic stress disorder, severity of injury, and associated bodily injuries. J Head Trauma Rehabil. 2018;33:101–12 The paper shows differential effects of sex on concussion/mTBI for service members.
Brickell TA, Lippa SM, French LM, Kennedy JE, Bailie JM, Lange RT. Female service members and symptom reporting after combat and non-combat-related mild traumatic brain injury. J Neurotrauma. 2017;34:300–12.
• Black AM, Sergio LE, Macpherson AK. The epidemiology of concussions: Number and nature of concussions and time to recovery among female and male Canadian varsity athletes 2008 to 2011. Clin J Sport Med. 2017;27:52–6 This paper reports higher frequency of concussions and association with sport played for Canadian women compared to Canadian men athletes.
•• Zuckerman SL, Kerr ZY, Yengo-Kahn A, Wasserman E, Covassin T, Solomon GS, et al. Epidemiology of sports-related concussion in NCAA athletes from 2009–2010 to 2013–2014: incidence, recurrence, and mechanisms. Am J Sports Med. 2016;44:NP5 This work identifies U.S. sex differences in rate of concussion as well as sports activities most likely to result in concussion.
• Sandel K, Schatz P, Goldberg KB, Lazar M. Sex-based differences in cognitive deficits and symptom reporting among acutely concussed adolescent lacrosse and soccer players. Am J Sports Med. 2017;45:937–44 This paper identifies sex differences in post-concussion deficits and symptoms for U.S. athletes.
• Sufrinko AM, Mucha A, Covassin T, Marchetti G, Elbin RJ, Collins MW, et al. Sex differences in vestibular/ocular and neurocognitive outcomes after sport-related concussion. Clin J Sport Med. 2017;27:190–4 Sex differences are reported in cognitive/neurocognitive outcomes after concussion.
• Zuckerman SL, Apple RP, Odom MJ, Lee YM, Solomon GS, Sills AK. Effect of sex on symptoms and return to baseline in sport-related concussion. J Neurosurg Pediatr. 2014;13:72–81 The work reports sex-dependent symptoms and recovery trajectories for sports-related concussions.
van der Horm HJ, Spikman JM, Jacobs B, van der Naalt J. Postconcussive complaints, anxiety, and depression with vocational outcome in patients with traumatic brain injury (TBI) of various severities and to assess sex differences. Arch Phys Med Rehabil. 2013;94:867–74.
•• Yilmaz T, Roks G, de Koning M, Scheenen M, van der Horn H, Plas G, et al. Risk factors and outcomes associated with post-traumatic headache after mild traumatic brain injury. Emerg Med J. 2017;34:800–5 The study found that women are more likely to have headache after mTBI.
• Gauvin-Lepage J, Friedman D, Grilli L, Gagnon I. Effect of sex on recovery from persistent postconcussion symptoms in children and adolescents participating in an active rehabilitation intervention. J Head Trauma Rehabil. 2018. https://doi.org/10.10897/HTR.0000000000000402The paper discusses findings that girls in concussion recovery have more symptoms, longer, than boys.
• Thomas DJ, Coxe K, Li H, Pommering TL, Young JA, Smith GA, et al. Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clin J Sport Med. 2018;28:56–63 This recent publication report recovery lengths are longer for women athletes after concussion.
• Lin CY, Casey E, Herman DC, Katz N, Tenforde AS. Sex differences in common sports injuries. PMR. 2018;10:1073–82 The paper states that more women athletes have concussions.
• Brooks BL, Silverberg N, Maxwell B, Mannix R, Zafonte R, Berkner PD, et al. Investigating effects of sex differences and prior concussions on symptom reporting and cognition among adolescent soccer players. Am J Sports Med. 2018;46:961–8 The authors report that women soccer players have different and longer lasting symptoms than men.
• Oyegbile TO, Delasobera BE, Zecavati N. Gender differences in sleep symptoms after repeat concussions. Sleep Med. 2017;40:110–5 This paper reports sex-specific differences in post-concussion symptoms in 8 to 17-year-old athletes showing girls have worse and long-lasting sleep difficulties than men after concussion.
Barnes BC, Cooper L, Kirkendall DT, McDermott TP, Jordan BD, Garrett WE. Concussion history in elite male and female soccer players. Am J Sports Med. 1998;26:433–8.
Ponsford JL, Myles PS, Cooper DJ, Mcdermott FT, Murray LJ, Laidlaw J, et al. Gender differences in outcome in patients with hypotension and severe traumatic brain injury. Injury. 2008;39:67–76.
Ley EJ, Short SS, Liou DZ, Singer MB, Mirocha J, Melo N, et al. Gender impacts mortality after traumatic brain injury in teenagers. J Trauma Acute Care Surg. 2013;75:682–6.
• Herrera-Melero MC, Egea-Guerrero JJL, Vilches-Arenas A, Rincon-Ferrari MD, Flores-Cordero JM, Leon-Carrion J, et al. Acute predictors for mortality after severe TBI in Spain: Gender differences and clinical data. Brain Inj. 2015;29:1439–44 The study showed that women have greater risk of mortality early on in recovery due to complications than men do after severe TBI.
Brooks JC, Strauss DJ, Shavelle RM, Paculdo DR, Hammond FM, Harrison-Felix CL. Long-term disability and survival in traumatic brain injury: results from the National Institute on Disability and Rehabilitation Research model systems. Arch Phys Med Rehabil. 2013;94:2203–9.
• Brooks JC, Shavelle RM, Strauss DJ, Hammond FM, Harrison-Felix CL. Long-term survival after traumatic brain injury Part II: Life expectancy. Arch Phys Med Rehabil. 2015;96:1000–5 The paper reports sex differences in life expectancy after TBI.
• Chan Y, Mollayeva T, Ottenbacher KJ, Colantonio A. Clinical profile and comorbidity of traumatic brain injury among younger and older men and women: a brief research note. BMC Res Notes. 2017;10:371 The study found that women and men have differing comorbidities that impact recovery.
Corrigan JD, Lineberry LA, Komaroff E, Langlois JA, Selassie AW, Wood KD. Employment after traumatic brain injury: differences between men and women. Arch Phys Med Rehabil. 2007;88:1400–9.
Stergiou-Kita M, Mansfield E, Sokoloff S, Colantonio A. Gender influences on return to work after mild traumatic brain injury. Arch Phys Med Rehabil. 2016;97:S40–5.
Arciniegas D, Adler L, Topkoff J, Cawthra E, Filley CM, Reite M. Attention and memory dysfunction after traumatic brain injury: cholinergic mechanisms, sensory gating, and a hypothesis for further investigation. Brain Inj. 1999;13:1–13.
Donders J, Hoffman NM. Gender differences in learning and memory after pediatric traumatic brain injury. Neuropsychol. 2002;16:491–9.
Russell KC, Arenth PM, Scanlon JM, Kessler L, Ricker JH. Hemispheric and executive influences on low-level language processing after traumatic brain injury. Brain Inj. 2012;26:984–95.
Ratcliff JJ, Greenspan AL, Goldstein FC, Stringer AY, Bushnik T, Hammond FM, et al. Gender and traumatic brain injury: Dr. the sexes fare differently? Brain Inj. 2007;21:1023–30.
Weintraub S, Dikmen SS, Heaton RK, Tulsky DS, Zelaxo PD, Slotkin J, et al. The cognition battery of the NIH toolbox for assessment of neurological and behavioral function: validation in an adult sample. J Int Neuropsychol Soc. 2014;20:567–78.
• Mollayeva T, Cassidy JD, Shapiro CM, Mollayeva S, Colantonio A. Concussion/mild traumatic brain injury related to chronic pain in males and females: A diagnostic modelling study. Medicine (Baltimore). 2017;96:e5917 The study analyses revealed sex-specific differences in how men and women experience pain after TBI.
Weiss PS. President Obama announces the BRAIN initiative. ACS Nano. 2013;7:2873–4.
Wagner AK, McCullough EH, Nivonkuru C, Ozawa H, Loucks TL, Dobos JA, et al. Acute serum hormone levels: characterization and prognosis after severe traumatic brain injury. J Neurotrauma. 2011;28:871–88.
•• Wunderle K, Hoeger KM, Wasserman E, Bazarian JJ. Menstrual phase as predictor of outcome after mild traumatic brain injury in women. J Head Trauma Rehabil. 2014;29:e1–8 The paper reports effects of endogenous sex hormones and oral contraceptives on response to TBI.
• Ranganathan P, Kumar RG, Davis K, McCullough EH, Berga SL, Wagner AK. Longitudinal sex and stress hormone profiles among reproductive age and post-menopausal women after severe TBI: A case series analysis. Brain Inj. 2016;30:452–61 This paper looks at complexities of sex hormones and TBI. This paper looks at complexities of sex hormones and TBI.
• Santarsieri M, Niyonkuru C, McCullough EH, Dobos JA, Dixon CE, Berga SL, et al. Cerebrospinal fluid cortisol and progesterone profiles and outcomes prognostication after severe traumatic brain injury. J Neurotrauma. 2014;31:699–712 The study finds associations between stress and sex hormone CSF levels and outcomes after severe TBI.
• Juengst SB, Arenth PM, Wagner A. Inflammation and apathy associations in the first year after traumatic brain injury. Arch Phys Med Rehabil. 2015;96:e98–9 This work links inflammation due to TBI with apathy during the first post-injury year.
• Juengst SB, Kumar RG, Failla MD, Goyal A, Wagner A. Acute inflammatory biomarker profiles predict depression risk following moderate to severe traumatic brain injury. J Head Trauma Rehabil. 2015;30:207–18 This work links inflammatory biomarkers of TBI with post-injury depression risk.
• Gallagher V, Kramer N, Abbott K, Alexander J, Breiter H, Herrold A, et al. The effects of sex differences and hormonal contraception on outcomes after collegiate sports-related concussion. J Neurotrauma. 2018;35:1242–7 Another paper (Wunderle) that similarly finds an association between outcomes and sex hormones/contraceptive use after concussion.
Russell AL, Richardson MR, Bauman BM, Hernandez IM, Saperstein S, Handa RJ, et al. Differential response of the HPA Axis to mild blast traumatic brain injury in male and female rats. Endocrinology. 2018;159:2363–75.
• Wirth P, Yu VV, Kimball AL, Liao J, Berkner P, Glenn MJ. New method to induce mild traumatic brain injury in rodents produces differential outcomes in female and male Sprague Dawley rats. J Neurosci Methods. 2017;290:133–44 Animal research study showing sex differences in outcomes from mTBI.
Semple BD, Dixit S, Shultz SR, Boon WC, O’Brien TJ. Sex-dependent changes in neuronal morphology and psychosocial behaviors after pediatric brain injury. Brain Inj. 2017;319:48–62.
• Wright DK, O’Brien TJ, Shultz SR, Mychasiuk R. Sex matters: repetitive mild traumatic brain injury in adolescent rats. Ann Clin Transl Neurol. 2017;4:640–65 Recent study showing sex differences in effects of repetitive mTBI.
• Thompson HJ, Vavilala MS, Rivara FP. Chapter 1 Common Data Elements and Federal Interagency Traumatic Brain Injury Research Informatics System for TBI Research. Annu Rev Nurs Res. 2015;33:1–11 The FITBUR informatics system is described.
Lamberty GJ, Nakase-Richardson R, Farrell-Carnahan L, McGarity S, Bidelspach D, Harrison-Felix C, et al. Development of a traumatic brain injury model system within the Department of Veterans Affairs Polytrauma System of care. J Head Trauma Rehabil. 2014;29:E1–7.
Traumatic Brain Injury Interagency Conference. https://interagencyconferencetbi.org/about/ Retrieved December 31, 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Janet Niemeier declares no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Injury Medicine and Rehabilitation
Rights and permissions
About this article
Cite this article
Niemeier, J.P. Biological Sex/Gender and Biopsychosocial Determinants of Traumatic Brain Injury Recovery Trajectories. Curr Phys Med Rehabil Rep 7, 297–304 (2019). https://doi.org/10.1007/s40141-019-00238-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-019-00238-3