Abstract
Introduction
To compare the anatomical and functional outcome and changes in the quality of life (QoL) over time of the lateral tarsal strip (LTS) versus the Quickert everting sutures (ES) for the repair of primary involutional lower eyelid entropion.
Methods
Forty-five patients (54 eyes) with primary involutional lower eyelid entropion were recruited in a prospective randomized clinical trial over 3-year period. Twenty-six eyes were randomized to the LTS technique and 28 to the ES procedure. Primary outcome was the anatomical correction of the eyelid at the final assessment in 1 year. Secondary outcomes were function and symptoms assessment with a QoL questionnaire at 6 months. Fisher’s exact test was used for the statistical analysis of success rate and gender study and Mann–Whitney U test and logistic regression analysis were used for age study. The Wilcoxon and Mann–Whitney U tests were used for the analysis of the National Eye Institute Visual Functioning Questionnaire-25 (NEI VFQ-25).
Results
At the 6-month follow-up, 25 eyes (96.2%) of the LTS group and 20 (71.4%) of the ES group had favorable outcome (P = 0.025). There were one and eight eyes, respectively, with early recurrence. At the final 12-month evaluation, 23 eyes (88.5%) in the LTS group and 16 eyes (57.1%) in the ES group were successful. Three (11.5%) and 12 (42.9%) eyes respectively showed postoperative recurrence. There was a statistically significant difference between the two groups (P = 0.015) for the primary outcome, whereas age and gender did not influence success. The NEI VFQ-25 showed statistically significant subjective improvement from baseline in most categories of the QoL. No significant difference between the two procedures was detected at 6 months.
Conclusion
This study suggests that the LTS procedure has a superior surgical success rate and reduction of symptoms compared with the ES for the repair of involutional lower eyelid entropion. Both procedures showed similar improvement of the postoperative QoL.
Trial registration
International Clinical Trials Registry Platform identifier: ACTRN12616000620426.
Similar content being viewed by others
Introduction
Entropion defines the inward turning of the eyelid margin and eyelashes against the eyeball. It is classified into the relatively rare congenital form, whereas acquired disease can be involutional, spastic or cicatricial. Involutional or senile entropion is the most frequently encountered lower lid malposition in the clinic [1, 2] with a reported prevalence of 2.1% in the elderly population (1.9% in men and 2.4% in women); it more frequently affects the lower eyelids, and there are no published details for the frequency of its surgical management [3].
Rubbing of the eyelashes against the ocular surface is a major cause for corneal epithelial abrasions which may evolve into ulceration and perforation with loss of vision in chronic cases [4].
The two key causative factors are reported to be the horizontal lid laxity mainly due to senile lateral canthal tendon elongation or dehiscence and the vertical laxity due to detachment of the inferior retractor from the tarsus. There is no published evidence on the relative contribution of each vector of lid laxity on the manifestation of involutional entropion.
There is an abundance of published surgical methods for the repair of involutional lower lid entropion, suggesting that there is incomplete understanding of the disease process and possibly low success rate of the available treatment modalities. The success and recurrence rates vary over time with longer follow-up revealing higher recurrence [5].
Literature data suggests that procedures combining horizontal and vertical eyelid tightening offer more favorable surgical outcome with long-lasting anatomical correction and high patient satisfaction [6, 7]. Even though combined procedures performed in specialist centers are the golden standard for entropion repair, the comparative efficacy of horizontal lid tightening versus retractor plication or stabilization for vertical tightening which can be performed by non-specialist ophthalmologists has not been systematically studied with all available data deriving from retrospective or case series reports [8].
The purpose of our study is to answer this clinical question by evaluating the comparative success rates of the everting sutures technique (Quickert everting sutures, ES) [9] for correcting vertical laxity with the lateral tarsal strip (LTS) technique [10] for horizontal eyelid tightening. The main advantage of the ES technique, in comparison to the LTS procedure or other therapeutic surgical options, is its simplicity. It is a low-cost method that can be easily performed more than once in older patients in the outpatient clinic, suitable for the general ophthalmologist, or even trained ophthalmic nurses.
Methods
This prospective randomized controlled trial (RCT) with identifier ACTRN12616000620426 was registered at ANZCTR following ethics committee approval by our local university investigational review board.
All procedures performed in studies involving human participants were in accordance with the Bioethics Committee of the Aristotle University Medical School and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Forty-five patients (54 eyes) with primary involutional lower eyelid entropion were recruited over a 3-year period, from May 2013 to February 2016, at the 1st Ophthalmology Department of Aristotle University of Thessaloniki and at the Ophthalmology Department of 424 General Military Hospital of Thessaloniki, Greece. Patients were recruited only after signing an informed consent for inclusion in the trial and were all operated on by the first author, a senior general ophthalmic surgeon. The mean age was 72.69 years (range 50–84 years). Baseline demographic characteristics of the comparative groups were similar with no statistically significant difference (Table 1).
Patients were randomized either to ES technique, or to the LTS procedure alone, irrespective of any degree of clinically apparent horizontal lid laxity. We did not use the preoperative data on horizontal laxity to stratify patients in the randomization process and allowed patients with a marked degree of laxity in the study pool. This helped to avoid selection bias in patient randomization and allowed a direct comparison of the two techniques alone in the general population. Patients were randomized with the use of a randomization table from a statistical book.
Exclusion criteria were cicatricial entropion or previous lower eyelid surgery for the same or other reason. Primary outcome was the anatomical correction of the eyelid at the final assessment in 1 year. Secondary outcomes were function and symptoms evaluation and changes in the quality of life (QoL) at 6 months.
Routine follow-up was scheduled within the first week and at 6 and 12 months after surgery.
In all cases, surgery was performed under local anesthesia. Topical anesthetic drops of tetracaine hydrochloride 0.5% were instilled in the lower conjunctival sac followed by subcutaneous infiltration of the lower eyelid with 2% lidocaine and 1:200 000 epinephrine anesthetic solution. In the LTS group, the lateral canthus and the lateral third of the upper eyelid were also infiltrated.
ES Technique
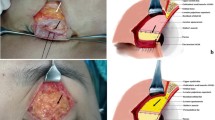
The ES technique consists of three (3) 6.0 double-armed polyglactin absorbable sutures (Vicryl, Ethicon, USA) placed obliquely, from the deep lower palpebral conjunctiva ideally engaging the capsulopalpebral fascia, forward through the eyelid exiting the skin 4–5 mm bellow the lash line. The 3 sutures were equally spaced within the lateral two-thirds of the lower eyelid, sparing the medial third to avoid punctum eversion. They were left in place to absorb spontaneously aiming at the formation of scar tissue to facilitate both adhesion of eyelid lamellae and inferior retractor stabilization close to the inferior tarsal plate [11].
LTS Procedure
The LTS procedure involves lateral canthotomy followed by cantholysis of the lateral palpebral ligament, preparation of an outer tarsal strip by dividing the anterior lamella (skin and orbicularis) from the lateral tarsus and removing the inferior and posterior conjunctiva and the lid margin tissue. Strip fixation to the inner periosteum of the lateral orbital rim at the corresponding area of Whitnall’s tubercule was performed with the use of a 5.0 double-armed braided polyester suture (Ethibond, Ethicon USA). The orbicularis muscle and skin were closed in layers with interrupted 6.0 polyglactin absorbable sutures (Vicryl, Ethicon USA) [12]. Skin sutures were removed in 1 week.
All patients were routinely prescribed a mixed gentamycin and dexamethasone ointment to use three times daily in the inferior conjunctival fornix and suture sites for 7 days. They were specifically instructed not to apply any traction to the lower eyelid for at least 3 weeks.
Surgical success and recurrence rates were assessed by clinical evaluation alone. At baseline and each follow-up visit, the operated lower eyelid was examined in the primary, up- and down-gaze positions. Evidence of generalized horizontal lid laxity and canthal tendon laxity as well as inferior retractor dehiscence with loss of lower lid skin crease and inferior fornix shallowing was recorded.
To identify latent or intermittent recurrence of entropion, patients were asked to forcefully squeeze their eyelids closed while looking downwards to elicit possible inward turning (Figs. 1, 2).
The QoL was assessed with the National Eye Institute Visual Functioning Questionnaire-25 (NEI VFQ-25) developed by RAND and funded by NEI, which was translated and validated in Greek language according to the instructions of RAND. The VFQ-25 was completed at baseline before surgery and at the 6-month follow-up visit.
The Fisher’s exact test was used for the statistical analysis of success rate and gender study, and the Mann–Whitney U test and logistic regression analysis were used for age study. The Wilcoxon and the Mann–Whitney U tests were used for the analysis of the NEI VFQ-25.
In order to capture dependencies between categorical variables, the non-parametric Fisher’s exact test was used, which enables the detection of discrete data interaction relations in small samples. Also, to examine the differences of the mean values of numerical variables based on the two-level categorical variables, the non-parametric Mann–Whitney U statistic, which is a two-way equilibrium test between independent samples, was used.
A P value < 0.05 was regarded statistically significant.
Results
Twenty-six Eyelids were Treated with the LTS Technique and Twenty-eight with the ES Method
Surgical success was defined as complete anatomical restoration of the eyelid position and resolution of symptoms.
At 6- and 12-months follow-up, the overall recurrence rate was different. The eyes in the LTS group had a much lower recurrence rate than those in the ES group, at both follow-up visits. There was a statistically significant difference between the two groups (P = 0.025 and 0.015, respectively; Table 1).
The age of the patient was not proven to be a confounding factor for the outcome.
This was found after applying a Mann–Whitney U test in order to compare the differences of the mean age of the patients based on whether they had or not postoperative recurrence (P > 0.05, Table 2) and by using the method of logistic regressions for each follow-up period in order to detect the effect of age on the appearance of postoperative recurrence (P > 0.05, Table 3).
The gender of the patient was also not correlated to the recurrence rate (Table 4).
All eyelids in the ES group had no surgical complication. One patient in the LTS group developed an abscess in the lateral canthal area at 12 months, possibly due to granuloma from the polyethylene fixation suture. This complication was surgically addressed by drainage of the abscess and excision of the suture granuloma.
As far as it concerns the subscales of the QoL, there was a comparison between the preoperative and postoperative data, as well as between the postoperative results of the two groups (Tables 5, 6).
Discussion
Our study is the first prospective RCT comparing the ES technique with the LTS procedure alone for the repair of primary involutional lower eyelid entropion [13]. Our results suggest that the LTS procedure alone is more effective than the ES technique at 12-months follow up (P = 0.015).
Patients treated with the ES procedure had a very high recurrence rate at 12 months (42.9%), possibly because, following the study design, we did not exclude from the group eyelids with marked horizontal eyelid laxity. Jang et al. reported similar results with a recurrence rate of 49.3% within 2 years postoperatively [14]. In another RCT, Scheepers et al. found a lower recurrence rate (21%) for ES alone at 18 months follow-up, but patients with excessive horizontal eyelid laxity were excluded from this procedure. In other retrospective studies, the recurrence rate at 12 months was from 12–25.5% [15,16,17]. Meadows et al. reported a 22% recurrence rate, but highlighted dermatochalasis and orbital fat prolapse of the lower eyelids as possible causative factors for entropion [18]. Indeed, evidence suggests that progressive senile changes of the lower eyelid tissues in addition to the relative enophthalmos due to orbital fat atrophy or forward prolapse are the main causative factors of involutional entropion [3, 19, 20].
The LTS group showed a recurrence rate of 11.5% at 12 months, higher than the recurrence rate of the combined procedure (ES + LTS) which was 0% at 18 months in the study by Scheepers et al. [21] and 9.4% at 24 months in the study by Ho et al. [22]. Published data shows that the recurrence rate of the LTS procedure alone varies from 14–22% while López-García et al. reported a rate of 4% for a modified LTS technique [23,24,25].
The ES procedure, which indirectly tightens the lower lid retractors, hence addressing vertical eyelid laxity, has a high recurrence rate (42.9%), especially if it is applied in cases with significant horizontal eyelid laxity. Despite this, it remains a simple and easily repeatable technique requiring basic surgical skills. The LTS procedure tightens the lid laterally, thus correcting the component of horizontal laxity. It is related to a much more favorable outcome (88.5%), but it requires a steeper learning curve.
Our study design deliberately did not stratify patient according to the degree of horizontal lid laxity as this would have been a selection bias for randomly comparing the two techniques and the corresponding causative factors for entropion. It is conceivable that in the daily clinical setting, assessment of horizontal laxity is of paramount importance for the selection of the appropriate surgical correction, as transcutaneous everting sutures may not function at all when there is significant horizontal laxity present [17]. Along those lines, our results clearly suggest that the horizontal component of lid laxity is more important than the vertical component for the correction of involutional lower lid entropion. This confirms the findings of previous trials suggesting that horizontal lid tightening in the form of a LTS is the far most important component of entropion repair, even when there is no clinically noticeable horizontal laxity present [24, 26, 27]. Direct retractor plication in the form of the Jones procedure is more effective than indirect retractor stabilization in the form of the Wies procedure or the less invasive Quickert transcutaneous sutures [26, 28].
Our results support the ample published evidence suggesting that the combined procedure addressing both horizontal and vertical lid laxity offers the best success rate with anatomical correction and very late, if any, recurrences achieving highest patient satisfaction [28,29,30]. This principle also applies in Asian eyelids with slightly different anatomy than the Caucasian eyelids [30].
Analysis of the VFQ-25 showed statistically significant improvement for most of the subscales at 6-months follow-up following surgical correction. We anticipated no effect and therefore no statistically significant difference for the distance activities, the color and the peripheral vision since lower lid entropion doesn’t affect these parameters. Similarly, comparing the two techniques postoperatively showed no statistically significant differences (P > 0.05) between the mean scores of the ocular pain (subjective symptoms) and the other VFQ-25 subscales.
The NEI VFQ-25 was developed at the National Eye Institute in Maryland, USA. It is a shorter version of the 51-item NEI VFQ, containing 25 items for the assessment of QoL [31].
The reason for the selection of the NEI VFQ-25 in our study was the available validated translation in Greek language and its widespread use over time for the evaluation of vision-related QoL in patients with various ocular diseases, such as age-related macular degeneration, cataract surgery, dry eye [32], glaucoma and uveitis. It is valid [33], reliable and highly repeatable with internal consistency [34]. It has been used extensively in clinical trials of ophthalmic research [35, 36].
The Glasgow Benefit Inventory (GBI) is a subjective post-interventional questionnaire, originally developed for otorhinolaryngological interventions that has also been used in oculoplastic surgery. It is simpler both for the examiner and patient since it is applied only once for assessment of the QoL changes after surgery. A draw-back of the GBI is that it doesn’t consider the preoperative condition of the patient, resulting in non-comparative scores [37].
The main limitations of our RCT are the lack of horizontal lower lid laxity measurement, the relatively small sample size and the medium-term follow-up of 12 months. However, our study contributes valuable documentation in the field of involutional lower eyelid entropion repair, since there is a clear need for more randomized studies in the field [13]. The use of the NEI VFQ-25 in this trial has its own limitations since it was developed in order to estimate the impact of visual impairment on QoL. It has a lower sensitivity for ocular pain assessment and the correlation between sub-scores and the eyelid malposition [31].
Conclusions
In conclusion, our results suggest that the LTS procedure is more effective than the ES technique for the repair or primary involutional lower eyelid entropion. As the patients were not stratified for horizontal lid laxity, we can theorize that this element of lid malposition is more important than vertical laxity in the development of entropion. However, the combined procedure addressing both horizontal and vertical lid laxity offers the optimum success rate with the best anatomical correction and very late recurrences, achieving high patient satisfaction. Τhe NEI VFQ-25 is a satisfactory QoL questionnaire for entropion repair.
References
Levine MR, Enlow MK, Terman S. Spastic entropion after cataract surgery. Ann Ophthalmol. 1992;24:195–8.
Pereira MG, Rodrigues MA, Rodrigues SA. Eyelid entropion. Semin Ophthalmol. 2010;25:52–8.
Damasceno RW, Osaki MH, Dantas PE, Belfort R Jr. Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthal Plast Reconstr Surg. 2011;27:317–20.
Musch DC, Sugar A, Meyer RF. Demographic and predisposing factors in corneal ulceration. Arch Ophthalmol. 1983;101:1545–8.
Marcet MM, Phelps PO, Lai JS. Involutional entropion: risk factors and surgical remedies. Curr Opin Ophthalmol. 2015;26:416–21.
Lai AFNNJ, Paridaens D, van den Bosch WA. Surgical correction of involutional lower lid entropion with lateral canthal eyelid block excision and imbrication of the capsulopalpebral ligament using non-buried non-resorbable imbricating sutures versus buried resorbable imbricating sutures. Orbit. 2018;38:1–6.
McVeigh KA, Harrison R, Ford R. Entropion and ectropion repair: a snapshot of surgical practice in the United Kingdom. Orbit. 2018;37:105–9.
Boboridis K, Bunce C. Interventions for involutional lower lid entropion. Cochrane Database Syst Rev 2002;1:CD002221.
Quickert MH, Rathbun E. Suture repair of entropion. Arch Ophthalmol. 1971;85:304–5.
Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol. 1979;97:2192–6.
Wright M, Bell D, Scott C, Leatherbarrow B. Everting suture correction of lower lid involutional entropion. Br J Ophthalmol. 1999;83:1060–3.
Vahdani K, Ford R, Garrott H, Thaller VT. Lateral tarsal strip versus Bick’s procedure in correction of eyelid malposition. Eye (Lond). 2018;32:1117–22.
Boboridis KG, Bunce C. Interventions for involutional lower lid entropion. Cochrane Database Syst Rev 2011;12:CD002221.
Jang SY, Choi SR, Jang JW, Kim SJ, Choi HS. Long-term surgical outcomes of Quickert sutures for involutional lower eyelid entropion. J Craniomaxillofac Surg. 2014;42:1629–31.
Baek JS, Choi SC, Jang SY, Lee JH, Choi HS. Comparison of surgical outcome between Quickert suture and Quickert suture with modified lateral tarsal strip in involutional lower eyelid entropion. J Craniofac Surg. 2016;27:198–200.
Mohammed BR, Ford R. Success rate of nurse-led everting sutures for involutional lower lid entropion. Eye (Lond). 2017;31:732–5.
Tsang S, Yau GS, Lee JW, Chu AT, Yuen CY. Surgical outcome of involutional lower eyelid entropion correction using transcutaneous everting sutures in Chinese patients. Int Ophthalmol. 2014;34:865–8.
Meadows AE, Reck AC, Gaston H, Tyers AG. Everting sutures in involutional entropion. Orbit. 1999;18:177–81.
Bashour M, Harvey J. Causes of involutional ectropion and entropion—age-related tarsal changes are the key. Ophthal Plast Reconstr Surg. 2000;16:131–41.
Damasceno RW, Heindl LM, Hofmann-Rummelt C, et al. Pathogenesis of involutional ectropion and entropion: the involvement of matrix metalloproteinases in elastic fiber degradation. Orbit. 2011;30:132–9.
Scheepers MA, Singh R, Ng J, et al. A randomized controlled trial comparing everting sutures with everting sutures and a lateral tarsal strip for involutional entropion. Ophthalmology. 2010;117:352–5.
Ho SF, Pherwani A, Elsherbiny SM, Reuser T. Lateral tarsal strip and Quickert sutures for lower eyelid entropion. Ophthalmic Plast Reconstr Surg. 2005;21:345–8.
Lopez-Garcia JS, Garcia-Lozano I, Gimenez-Vallejo C, Jimenez B, Sanchez A, de Juan IE. Modified lateral tarsal strip for involutional entropion and ectropion surgery. Graefes Arch Clin Exp Ophthalmol. 2017;255:619–25.
Olver JM, Barnes JA. Effective small-incision surgery for involutional lower eyelid entropion. Ophthalmology. 2000;107:1982–8.
Rougraff PM, Tse DT, Johnson TE, Feuer W. Involutional entropion repair with fornix sutures and lateral tarsal strip procedure. Ophthalmic Plast Reconstr Surg. 2001;17:281–7.
Boboridis KG, Mikropoulos DG, Ziakas NG. Entropion. Ophthalmology. 2011;118:225–6 (author reply 6).
Danks JJ, Rose GE. Involutional lower lid entropion: to shorten or not to shorten? Ophthalmology. 1998;105:2065–7.
Boboridis K, Bunce C, Rose GE. A comparative study of two procedures for repair of involutional lower lid entropion. Ophthalmology. 2000;107:959–61.
Lee H, Takahashi Y, Ichinose A, Kakizaki H. Comparison of surgical outcomes between simple posterior layer advancement of lower eyelid retractors and combination with a lateral tarsal strip procedure for involutional entropion in a Japanese population. Br J Ophthalmol. 2014;98:1579–82.
Serin D, Buttanri IB, Karslioglu S, Sevim MS, Buttanri B, Akbaba M. The efficacy of the combined procedure in involutional entropion surgery: a comparative study. Korean J Ophthalmol. 2013;27:405–8.
Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item national eye institute visual function Questionnaire. Arch Ophthalmol. 2001;119:1050–8.
Li XM, Hu L, Hu J, Wang W. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26:S16–20.
Marella M, Pesudovs K, Keeffe JE, O’Connor PM, Rees G, Lamoureux EL. The psychometric validity of the NEI VFQ-25 for use in a low-vision population. Invest Ophthalmol Vis Sci. 2010;51:2878–84.
Sivaprasad S, Tschosik E, Kapre A, et al. Reliability and construct validity of the NEI VFQ-25 in a subset of patients with geographic atrophy from the phase 2 mahalo study. Am J Ophthalmol. 2018;190:1–8.
Piper RJ, Kalyvas AV, Young AM, Hughes MA, Jamjoom AA, Fouyas IP. Interventions for idiopathic intracranial hypertension. Cochrane Database Syst Rev 2015;8:CD003434.
Squires H, Poku E, Bermejo I, et al. A systematic review and economic evaluation of adalimumab and dexamethasone for treating non-infectious intermediate uveitis, posterior uveitis or panuveitis in adults. Health Technol Assess. 2017;21:1–170.
Smith HB, Jyothi SB, Mahroo OA, et al. Patient-reported benefit from oculoplastic surgery. Eye (Lond). 2012;26:1418–23.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Elias A. Nakos, Konstadinos G. Boboridis, Angeliki A. Kakavouti–Doudou, Diamantis D. Almaliotis, Christos E. Sioulis and Vasileios E. Karampatakis have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the Bioethics Committee of the Aristotle University Medical School and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article, go to https://doi.org/10.6084/m9.figshare.8124122.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nakos, E.A., Boboridis, K.G., Kakavouti-Doudou, A.A. et al. Randomized Controlled Trial Comparing Everting Sutures with a Lateral Tarsal Strip for Involutional Lower Eyelid Entropion. Ophthalmol Ther 8, 397–406 (2019). https://doi.org/10.1007/s40123-019-0189-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-019-0189-3