Abstract
Engaging global key opinion leaders, the International Psoriasis Council (IPC) held a day-long roundtable discussion with the primary purpose to discuss the treatment goals of psoriasis patients and worldwide barriers to optimal care. Setting clear expectations might ultimately encourage undertreated psoriasis patients to seek care in an era in which great gains in therapeutic efficacy have been achieved. Here, we discuss the option for early treatment of all categories of psoriasis to alleviate disease impact while emphasizing the need for more focused attention for psoriasis patients with mild and moderate forms of this autoimmune disease. In addition, we encourage policy changes to keep pace with the innovative therapies and clinical science and highlight the demand for greater understanding of treatment barriers in resource-poor countries.
Similar content being viewed by others
Introduction
Psoriasis is an immune-mediated inflammatory skin disease with significant physical and psychosocial consequences. Visible skin disfigurement and the associated symptoms of itch, pain, scaling, bleeding, burning, and cracking have a significant impact on the patient’s quality of life. Additionally, psoriasis is a systemic disease with multiple comorbidities, which increase the disease burden to beyond the realm of the skin [1]. Despite the current large inventory of effective treatment choices, including innovative biologics and oral therapy, undertreatment and non-treatment of psoriasis is prevalent worldwide, including in Europe and the USA [2]. This situation is even worse in developing countries where psoriasis patients with moderate-to-severe disease have poor access to the novel and costlier therapies [2,3,4,5,6]. The “Clear about Psoriasis” global study involving 31 countries (Western and non-Western) identified that 57% of moderate-to-severe psoriasis patients surveyed did not achieve clear/almost clear skin on current therapy [7], which recapitulates earlier findings that a majority of psoriasis patients worldwide are undertreated.
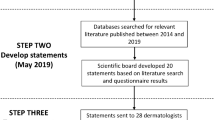
Key stakeholders agree that this global problem is driven by economics, market access, health policies, differences in the patient and physician perspectives on the disease, knowledge gaps, and the lack of established treatment goals. Councilors from the International Psoriasis Council (IPC) convened during a roundtable event, with the primary purpose to discuss clinical goals and specific barriers to optimal treatment and to highlight challenges for patients living in both Western and non-Western countries (Table 1). The event included dermatologists from ten different countries, and the intent was to reveal global perspectives and provide expert opinion.
This article does not contain any studies with human participants or animals performed by any of the authors.
Current State of Patient Satisfaction
In previous surveys psoriasis patients have reported treatment dissatisfaction [2] and failure to meet treatment goals with current therapy [3]. A recent review of 60 published studies/articles, which included 35,388 psoriasis patients, noted modest patient satisfaction, with those patients treated with biologics reporting higher satisfaction than those treated with oral therapies, phototherapy, or topicals [8]. How these data would differ today given the introduction of the newer biologic therapies, such as interleukin (IL) inhibitors (IL-17 and IL-23), which have excellent clinical efficacy but significant cost issues, is yet to be determined. Part of the problem is that the majority of recent innovation have been targeted to the moderate-to-severe patient population, with little new successful development for those psoriasis patients with mild and moderate disease.
Psoriasis severity is generally defined by clinicians using objective measures of body surface area (BSA), the Psoriasis Area Severity Index (PASI), or one of several Physician Global Assessment (PGA) measures [9]. Additionally, the impact of psoriasis on patients’ quality of life may be evaluated by the Dermatology Life Quality Index (DLQI), a self-reported questionnaire assessing the physical, psychological, and social well-being of patients [10]. Psoriasis patients and their physicians differ with regard to which psoriasis symptoms are most important. For example, some patients have found itch to be most bothersome, while dermatologists reported the location and size of the skin lesions as paramount [11]. Itch, affecting 60–96% of patients, is the primary source of discomfort, negatively impacting daily physical and mental well-being [12,13,14]. Clinical studies with ixekizumab [15, 16], tofacitinib [17], apremilast [18], etanercept [19], and secukinumab [20] have shown a significant association of improvement of itch with a correlative improvement of the quality of life for patients. Not surprisingly, the reduction of itch and pain is strongly correlated with skin clearance [21] [15]. In addition to physical symptoms of itch and pain, the visible aspect of the disease impacts many psychosocial domains. Anxiety and depression can lead to avoidance and reduction of social interactions [7, 22, 23]. In a recent global study, 84% of psoriasis patients surveyed reported humiliation, discrimination, difficulty in social/work situations, sleep disturbance, and mental health issues. In addition, both the physical symptoms plus psychiatric morbidity can negatively impact intimate relationships and sexual activity [24, 25]. These important factors, if recognized by the dermatologist, can be used to guide treatment decisions and provide educational health resources to the patient.
The reason for the discrepancy between patients and physician regarding the most bothersome symptoms of the disease is possibly due to the objective approach taken to determine disease severity by the physician versus the subjective manner by which patients experience and monitor their disease symptoms. Consequently, the physician’s use of the PASI could potentially miss the effect of a therapy on the specific symptoms, such as itch, burning, pain, and stinging, that commonly affect psoriasis patients. The DLQI captures the symptoms of itching, soreness, pain, and stinging using one question, but it does not evaluate each separately. This points to the potential value of utilizing psoriasis-specific patient-reported instruments that assess individual symptoms in conjunction with quality-of-life inquiries.
Disease-Specific Patient Reported Outcome Measures are Needed to Define Success and to Inform Clinical Decisions
Current outcome measures may not be helpful in distinguishing which psoriasis therapies are clinically meaningful unless they have established the minimal clinically important difference (MCID) for score change [26]. Certainly, the main goal of psoriasis treatment is to achieve skin clearance and to restore the patient’s normal daily activities to where this disabling disease has no impact on work, family life, social connections, and well-being of the patient [7, 26].
To this end, patient reported outcomes (PROs) complement and qualify objective (observer only) tools [26, 27] and move the focus from objective to subjective (patient-experienced) measures. The DLQI, a PRO that is not specific for psoriasis, is composed of content that includes important and relevant concepts from the perspective of psoriasis patients [28] and is the most widely accepted PRO currently available to clinicians. Psoriasis-specific PROs should capture corresponding elements of the DLQI that have been clinically validated, that are responsive to change, and which are determined as well understood by patients [28, 29] but which may need to be expanded to include other elements. A thorough assessment of psoriasis-specific PRO tools has been systematically reviewed elsewhere [30, 31].
The International Dermatology Outcome Measures Group (IDEOM) is one initiative which aims to establish validated and standardized outcome measures that satisfy the needs of all stakeholders for use in clinical trials and clinical practice [32,33,34]. The core domains that have been identified are skin manifestations (surface area of involvement, location, redness, induration, and scale), investigator global assessments, psoriasis and psoriatic arthritis symptoms, patient global assessment, treatment satisfaction, and health-related quality of life [35].
Ideally, an effective PRO with regard to measuring both disease severity and treatment effects could replace objective metrics such as the PASI or PGA. Furthermore, the discussion of PRO results has the potential to significantly enhance the physician–patient interaction and contribute to the formation of valid treatment goals.
Treatment Expectations and Clinical Goals
In the majority of cases, patient expectations are influenced by the clinician, but neither the patient nor the clinician may be fully aware of what the patient believes is most important. Dermatologists are generally calibrated to patient expectations that are highly related to factors such as age, gender, socioeconomic status, occupation, and geographic locale [36]. In a German registry, patients surveyed reported a wide range of highly valued treatment goals beyond skin clearance, which included improvement of itching, burning, and pain and normal life functioning [37]. In addition, many patients are unaware that there is a possibility of attaining 100% clearance over both the short term and long term, or of achieving substantial improvement or elimination of their most troublesome symptoms [7]. Treatment goal misalignment was reported in 67.9% of patient–physician pairs surveyed in a study conducted in Japan which examined skin clearance as a goal indicator [38]. The main reason for misalignment was that patients expressed a higher goal than physicians. This finding again highlights the importance of dermatologists recognizing patient expectations in order to reach clinical goals. It is likely that this disconnect also contributes to the finding that adherence to treatment falls well below that for other chronic conditions [39, 40]. In part, adherence is negatively affected by patient psychological barriers related to past failed treatments, whereby the patient becomes resigned to modest or limited outcomes (inadequate skin clearance and relief from symptoms) [41].
What Defines Treatment Success or Failure?
Treatment success in managing chronic disease has been defined as control of a target that is quantifiable to a specified value or range (e.g., for certain conditions, glycated hemoglobin levels, lipid profiles, blood pressure ranges, or virus burden). The identification and acceptance of treatment goals require the establishment of minimal disease criteria through literature review and a subsequent expert consensus building exercise, such as the Delphi process. Target goals should be defined for both the initiation and maintenance phases of treatment and should also be easy to implement in clinical practice and feasible to attain. Ideally, treatment goals should correlate with meaningful effects on systemic comorbidities, such that achieving these targets has positive effects on either morbidity or mortality. Such targets for psoriasis therapy are yet to be identified.
Once target goals have been established, a “treat to target” approach can be compared to standard care to identify the best approach for disease management. For example, in psoriatic arthritis, the Tight Control of Psoriatic Arthritis study (TICOPA) investigated an intensive and early treatment protocol versus standard care [42]. First, the target goals of minimal disease activity (MDA) criteria were validated through observation and investigational studies and then these goals were applied in the TICOPA study. The results of the study determined that intensive care (review every 4 weeks, with escalation of treatment to MDA targets) provided greater patient improvement in disease activity and reduction in joint damage than standard care (review at 12 weeks).
Treatment goals for psoriasis have been defined by European [43], American [44], Canadian [45], and Australian [46] consensus committees according to shared criteria that define treatment success. The recently published consensus from the US National Psoriasis Foundation posits that an acceptable response to treatment at 3 months after initiation is ≤ 3% BSA or a BSA improvement of ≥ 75% from baseline; the target treatment response at 3 months after initiation is ≤ 1% BSA; and the target response at each 6-month maintenance appointment is ≤ 1% BSA [44].
These targets, which have been established to improve patient outcomes in diverse clinical settings within Western countries, may need modification in non-Western countries due to safety concerns in vulnerable populations. For example, Brazil has adopted the European targets with a few modifications due to the high local prevalence of human T-lymphotropic virus (HTLV) and tuberculosis infection burden, which demands screening before initiating treatment with immunosuppressive therapies [47]. More information is needed to establish the burden of psoriasis within populations of Latin America and the Caribbean in order to gain a stronger understanding of patient perspectives and barriers to care [48].
The Malaysian Ministry of Health lists treatment goals as minimum targets within therapy categories (topicals, phototherapy, conventional therapies, or biologics) and highlights the need for target goals to be based on patient severity and patient preference [49].
Clinically Meaningful Targets
It appears to be relatively straightforward to provide treatment with the target of skin clearance based on BSA, PASI, or PGA (minimal disease criteria), but the degree that is clinically meaningful to the patient should be clarified. A recent study examined the impact of total skin clearance on quality of life from the patient’s perspective by investigating PSI and DLQI [26]. Patients that responded to treatment with total skin clearance (PASI 100 and PGA 0) demonstrated minimal or no impairment in dermatology-related quality of life factors or signs and did not experience symptoms of psoriasis. This outcome translates into a clinically meaningful treatment goal for patients. The study further revealed that even small areas of residual disease in patients that did not respond with complete clearance have a negative impact on patient quality of life and psoriasis symptoms.
Examination of other target goals below PASI100 might also be useful for determining the relationship between categories of PASI response levels. For example, data derived from clinical studies on secukinumab reveal that achieving a PASI response of 90 correlates with better quality of life (DLQI 0/1) at week 12 than achieving a PASI response of 75–89 [50]. When setting treatment goals, it should be understood that the concept of percentage PASI reduction as the only outcome measure might not be relevant for individual patients; rather, absolute change is usually more relevant. In this vein, the MCID score for absolute change of the metric being used should be better understood; for example, for the DLQI, the MCID is a score change of 4 [51].
Overall, current evidence supports the conclusion that greater skin clearance correlates with greater improvement of patient quality of life. However, studies have also shown that skin lesion severity on the head and upper extremities had disproportionately large impacts on DLQI compared with BSA, particularly for younger women and men. The impact was significantly greater in women aged < 45 years (higher DLQI) [52]. In addition, genital psoriasis, which affects over 60% of psoriasis patients, imparts significant impairment on the quality of life, feelings of stigmatization, and impact on sexual health [25]. These findings again point to the importance of patient perspectives on treatment goals and expectations.
Finally, the impact of psoriasis extends beyond the patient. Disease burden on family members and partners has garnered little attention in the past and, due to this lack of consideration, is a hidden and often ignored important aspect of the disease. However, observational studies have captured the degree of impairment in the quality of life of persons living with psoriasis patients using family quality reported outcome instruments, such as Psoriasis Family Index (PFI), Family Dermatology Life Quality Index (FDLQI), and Family Reported Outcome Measure (FROM-16) [23, 53–56]. Family members are burdened with psychological pressures, disruption of social, holiday, and sports activities, and disturbance in daily activities [23].
Treat-to-Target: A Reality or Aspirational?
The treat-to-target approach may be difficult to implement in global clinical practices if the target goal is too ambitious and beyond the reach of the majority of patients. PASI100 should be considered to be an aspirational and important goal, as no current treatment can achieve it in more than 50% of patients. For example, in the UNCOVER-1 study, 35.3% of patients treated with ixekizumab reached PASI100 at week 12 [57]. PASI 90, on the other hand, is achievable in a larger percentage of patients treated with IL-17 inhibitors (ixekizumab 70.9% [57]; secukinumab 70.0% [58]; brodalumab 70.3% [59]) and IL-23p19 inhibitors (risankizumab 77% [60]; tildrakizumab 58% [61]; guselkumab 73.3% [62]). Other concerns regarding the treat-to-target approach include the possibility of inappropriate treatment if non-response or loss of response is not well understood, patient reluctance to undergo increased monitoring, dosing, or switching of therapies with a different mode of action, and potential increase in cost. Ultimately, therapy must be customized, as the definition of success will depend on the patient’s perspective [63].
In addition, goals should be set to encourage physicians to optimize treatments and maximize long-term quality of life—while reducing the risk of important comorbidities. However, setting an actual number value within formal treatment guidelines used by physicians and private healthcare insurers may negatively impact access. For example, if a target is not met despite the patient being satisfied, insurers might deny payment. In resource-poor countries, such as Brazil, where the government health agencies approve biologics but deny access to the public healthcare system due to economic reasons, physicians would be caught between the treat-to-target guidelines (and patient expectations) and divergent public healthcare policies [47].
Clearance and Longevity
With the current broad spectrum of available psoriasis therapies, sustained and consistent clearance of psoriasis is a definite possibility [26]. In large patient populations, greater clearance translates to greater satisfaction, as patients who achieve full clearance (when compared to those who are “almost clear”) more often report greater symptom resolution [64]. Importantly, psoriasis patients who are effectively treated may display a “reset” of the level of disease that can be tolerated. Treatment discontinuation after initial success results in a rebound dissatisfaction with returning disease (worsening of quality of life). Small recurrences of psoriasis therefore translate into disproportionately larger detrimental effects on quality of life reporting [65]. Reduction of drug dose after initial treatment success could result in a similar phenomenon [66].
These data would support the avoidance of unnecessary switching among therapies in order to increase the likelihood of long-term patient satisfaction. However, sustained efficacy is still a significant shortcoming with the biologic therapies, and corrective approaches to this problem are hindered by a lack of head-to-head studies between therapies and an understanding of the mechanisms by which therapies lose their effectiveness over time. Access to observational prospective registries has allowed some comparative assessments of long-term efficacy [67–69]. The use of concomitant immunomodulatory drugs, such as methotrexate, is inadequately studied, but it is well recognized from the rheumatology literature that this approach may lengthen treatment response [70, 71]. In this regard, it is important to realize that only monotherapy (including no potent topical steroids) is allowed in psoriasis clinical trials, whereas in rheumatology clinical studies, including those in psoriatic arthritis, more than 50% of patients in the clinical trials conducted to date are on concomitant systemic therapy (methotrexate, prednisone, etc.). In addition, because drug durability rates are possibly lower in the clinical setting than in controlled trials, more real-world studies [72] are needed to gauge the longevity of response of the novel biologics and oral therapies.
There is also a need for variable dosing in studies of the various drugs to better understand how long-term clearance might be sustained. Internationally, methotrexate is the most widely used systemic therapy due to its reasonable efficacy and low cost. A recent survey administered across 63 countries demonstrated significant differences on dosing, route of administration, and safety monitoring of methotrexate [73]. In fact, an intensified dosing schedule of subcutaneous methotrexate over 52 weeks was found to be effective and well tolerated in moderate to severe patients [74].
Clinical Inertia and Patient Barriers
Clinical inertia, a concept coined in early 2000s, is defined as the failure to initiate and/or to intensify care when treatment goals are not met [75]. Evidence for clinical inertia in the treatment of psoriasis has been established; for example, in the studies (described above) in which only 31% of patients report that the target goal of skin clearance is reached.
Recent observational evidence suggests that patients, on average, seek referral to a secondary care (specialist) 15 years after presentation [76]. The authors of this study report that this delay in seeking help can be attributed to several barriers, including familial experience of the disease (acceptance that many family members have psoriasis); previous failed therapies and thus a sense of hopelessness; lack of follow-up to assess treatment response after initiation; and difficulty in obtaining a secondary care referral. Strikingly, patient conception of psoriasis as being neither curable nor life-threatening, and thus unworthy of treatment, was also identified as a strong barrier to seeking effective treatment [76]. The barriers identified here are modifiable and have the potential to lead the patient to early treatment.
Access to expert care for patients with moderate to severe disease is affected by several factors. First among these is the inadequate supply of or limited access to dermatology practitioners in countries worldwide. Second, the framework in which patients receive care may not support the complexity needed for appropriate evaluation and management of psoriasis. Given the time constraints of the average dermatology clinic visit (5–15 min), arriving at effective treatment that maximizes both physician and patient outcomes and satisfaction may be challenging. Third, access to medications is frequently constrained. While psoriasis is a systemic disease associated with chronic inflammation and, in a number of patients, end-organ damage, it continues to be viewed by patients, physicians, and payors as a cosmetic or “itchy skin” problem and not of equal health significance as, for example, rheumatologic disorders. For example, US payers make decisions on physician and drug quality based on claims databases in community practices that do not assess either patient severity, associated comorbidities, or disease-specific outcomes [77]. Treatment regimens for psoriasis patients should be tailored to meet specific needs based on disease severity, impact on quality of life, response to previous therapies, and presence of comorbidities. With regard to comorbidities such as psoriatic arthritis, it is important to ensure that the appropriate agent not only improves the disease symptoms but also has the potential to inhibit the radiographic progression of disease [78]. In addition, since psoriasis is a chronic systemic and incurable disease that affects all age groups, special populations, such as pregnant women, pediatric patients, elderly patients, and those with chronic infections, must be considered [79].
Disparate treatment access for psoriasis patients is especially high for those who seek biologic treatment and new oral therapies in developing countries. In 2016, the World Health Organization issued a global report to emphasize that psoriasis is a serious, disfiguring, and disabling non-communicable disease and set forth actions to improve healthcare across all countries [6]. Communicable diseases still contribute significantly to disease burden in most developing countries, and a majority of the financial resources is dedicated to providing these treatments. However, recent studies have reported that the occurrence of non-communicable disease doubles the overall health burden [80, 81]. In some developing countries the economic burden of modern, highly effective therapies will drive the discussion. Unless pharmaceutical companies, payers, and regulators reach a consensus on how to adequately fit treat-to-target guidelines into the healthcare general budget, achieving excellent standard of care will be challenging. A better understanding of factors that influence disparity is critical to narrowing the healthcare gaps for patients.
Conclusions
Over 125 million people living with psoriasis depend on feasible approaches to attain treatment goals in order to reverse the current state of untreated and undertreated patient populations. Delivering comprehensive treatment information to the patient will help develop realistic expectations and lead to improved health outcomes [36, 43]. Further, patients and healthcare providers should appreciate that even though skin clearance is achieved in the short term, clearance must be maintained and a long-term strategy must be implemented in the form of a multidisciplinary approach that limits the comorbidities associated with psoriasis [11, 82, 83].
References
Boehncke WH, Boehncke S. More than skin-deep: the many dimensions of the psoriatic disease. Swiss Med Wkly. 2014;144:w13968. https://doi.org/10.4414/smw.2014.13968.
Armstrong AW, Robertson AD, Wu J, Schupp C, Lebwohl MG. Undertreatment, treatment trends, and treatment dissatisfaction among patients with psoriasis and psoriatic arthritis in the United States: findings from the National Psoriasis Foundation surveys, 2003–2011. JAMA Dermatol. 2013;149(10):1180–5. https://doi.org/10.1001/jamadermatol.2013.5264.
van de Kerkhof PC, Reich K, Kavanaugh A, et al. Physician perspectives in the management of psoriasis and psoriatic arthritis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis survey. J Eur Acad Dermatol Venereol. 2015;29(10):2002–10. https://doi.org/10.1111/jdv.13150.
Lebwohl MG, Kavanaugh A, Armstrong AW, Van Voorhees AS. US perspectives in the management of psoriasis and psoriatic arthritis: patient and physician results from the population-based multinational assessment of psoriasis and psoriatic arthritis (MAPP) survey. Am J Clin Dermatol. 2016;17(1):87–97. https://doi.org/10.1007/s40257-015-0169-x.
Armstrong AW, Koning JW, Rowse S, Tan H, Mamolo C, Kaur M. Under-treatment of patients with moderate to severe psoriasis in the United States: analysis of medication usage with health plan data. Dermatol Ther (Heidelb). 2016. https://doi.org/10.1007/s13555-016-0153-2.
World Health Organization. World Health Organization global report on psoriasis. Geneva: World Health Association; 2016.
Armstrong A, Jarvis S, Boehncke WH, et al. Patient perceptions of clear/almost clear skin in moderate-to-severe plaque psoriasis: results of the Clear About Psoriasis worldwide survey. J Eur Acad Dermatol Venereol. 2018;32(12):2200–2207. https://doi.org/10.1111/jdv.15065.
Florek AG, Wang CJ, Armstrong AW. Treatment preferences and treatment satisfaction among psoriasis patients: a systematic review. Arch Dermatol Res. 2018;310(4):271–319. https://doi.org/10.1007/s00403-018-1808-x.
Langley RG, Ellis CN. Evaluating psoriasis with psoriasis area and severity index, psoriasis global assessment, and lattice system physician’s global assessment. J Am Acad Dermatol. 2004;51(4):563–9. https://doi.org/10.1016/j.jaad.2004.04.012.
Finlay AY, Khan GK. Dermatology life quality index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6.
Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based multinational assessment of psoriasis and psoriatic arthritis survey. J Am Acad Dermatol. 2014;70(5):871–81. https://doi.org/10.1016/j.jaad.2013.12.018.
Ryan C, Menter A. Discordance between physician assessment of psoriasis and patient self-assessment: the importance of itch. Br J Dermatol. 2016;175(1):19–20. https://doi.org/10.1111/bjd.14672.
Globe D, Bayliss MS, Harrison DJ. The impact of itch symptoms in psoriasis: results from physician interviews and patient focus groups. Health Qual Life Outcomes. 2009;7:62. https://doi.org/10.1186/1477-7525-7-62.
Szepietowski JC, Reich A. Itch in psoriasis management. Curr Probl Dermatol. 2016;50:102–10. https://doi.org/10.1159/000446050.
Kimball AB, Luger T, Gottlieb A, et al. Impact of ixekizumab on psoriasis itch severity and other psoriasis symptoms: results from 3 phase III psoriasis clinical trials. J Am Acad Dermatol. 2016. https://doi.org/10.1016/j.jaad.2016.07.034.
Leonardi CL, Blauvelt A, Sofen HL, et al. Rapid improvements in health-related quality of life and itch with ixekizumab treatment in randomized phase 3 trials: results from UNCOVER-2 and UNCOVER-3. J Eur Acad Dermatol Venereol. 2017. https://doi.org/10.1111/jdv.14211.
Feldman SR, Thaci D, Gooderham M, et al. Tofacitinib improves pruritus and health-related quality of life up to 52 weeks: results from 2 randomized phase III trials in patients with moderate to severe plaque psoriasis. J Am Acad Dermatol. 2016. https://doi.org/10.1016/j.jaad.2016.07.040.
Sobell JM, Foley P, Toth D, et al. Effects of apremilast on pruritus and skin discomfort/pain correlate with improvements in quality of life in patients with moderate to severe plaque psoriasis. Acta Derm Venereol. 2016;96(4):514–20. https://doi.org/10.2340/00015555-2360.
Mrowietz U, Chouela EN, Mallbris L, et al. Pruritus and quality of life in moderate-to-severe plaque psoriasis: post hoc explorative analysis from the PRISTINE study. J Eur Acad Dermatol Venereol. 2015;29(6):1114–20. https://doi.org/10.1111/jdv.12761.
Stull C, Grossman S, Yosipovitch G. Current and emerging therapies for itch management in psoriasis. Am J Clin Dermatol. 2016;17(6):617–24. https://doi.org/10.1007/s40257-016-0213-5.
Viswanathan HN, Chau D, Milmont CE, et al. Total skin clearance results in improvements in health-related quality of life and reduced symptom severity among patients with moderate to severe psoriasis. J Dermatolog Treat. 2015;26(3):235–9. https://doi.org/10.3109/09546634.2014.943687.
Anstey A, McAteer H, Kamath N, Percival F. Extending psychosocial assessment of patients with psoriasis in the UK, using a self-rateds, web-based survey. Clin Exp Dermatol. 2012;37(7):735–40. https://doi.org/10.1111/j.1365-2230.2012.04457.x.
Eghlileb AM, Davies EE, Finlay AY. Psoriasis has a major secondary impact on the lives of family members and partners. Br J Dermatol. 2007;156(6):1245–50. https://doi.org/10.1111/j.1365-2133.2007.07881.x.
Sampogna F, Abeni D, Gieler U, et al. Impairment of sexual life in 3,485 dermatological outpatients from a multicentre study in 13 European countries. Acta Derm Venereol. 2017;97(4):478–82. https://doi.org/10.2340/00015555-2561.
Ryan C, Sadlier M, De Vol E, et al. Genital psoriasis is associated with significant impairment in quality of life and sexual functioning. J Am Acad Dermatol. 2015;72(6):978–83. https://doi.org/10.1016/j.jaad.2015.02.1127.
Strober B, Papp KA, Lebwohl M, et al. Clinical meaningfulness of complete skin clearance in psoriasis. J Am Acad Dermatol. 2016. https://doi.org/10.1016/j.jaad.2016.03.026.
Lebwohl M, Swensen AR, Nyirady J, Kim E, Gwaltney CJ, Strober BE. The Psoriasis Symptom Diary: development and content validity of a novel patient-reported outcome instrument. Int J Dermatol. 2014;53(6):714–22. https://doi.org/10.1111/j.1365-4632.2012.05798.x.
Safikhani S, Sundaram M, Bao Y, Mulani P, Revicki DA. Qualitative assessment of the content validity of the dermatology life quality index in patients with moderate to severe psoriasis. J Dermatol Treat. 2013;24(1):50–9. https://doi.org/10.3109/09546634.2011.631980.
Loo WJ, Diba V, Chawla M, Finlay AY. Dermatology Life Quality Index: influence of an illustrated version. Br J Dermatol. 2003;148(2):279–84.
Kitchen H, Cordingley L, Young H, Griffiths CE, Bundy C. Patient-reported outcome measures in psoriasis: the good, the bad and the missing! Br J Dermatol. 2015;172(5):1210–21. https://doi.org/10.1111/bjd.13691.
Ali FM, Cueva AC, Vyas J, et al. A systematic review of the use of quality-of-life instruments in randomized controlled trials for psoriasis. Br J Dermatol. 2017;176(3):577–93. https://doi.org/10.1111/bjd.14788.
Greb JE, Merola J, Garg A, et al. The psoriatic disease payer advisory panel. J Drugs Dermatol. 2016;15(5):641–4.
Merola JF, Armstrong AW, Saraiya A, et al. International dermatology outcome measures initiative as applied to psoriatic disease outcomes: an update. J Rheumatol. 2016;43(5):959–60. https://doi.org/10.3899/jrheum.160114.
Callis Duffin KMJ, Christensen R, Latella J, Garg A, Gottlieb AB, Armstrong AW. Identifying a core domain set to assess psoriasis in clinical trials: a combined delphi consensus survey from the international dermatology outcome measures initiative. JAMA Dermatol.2018;154(10):1137–44. https://doi.org/10.1001/jamadermatol.2018.1165
Perez-Chada LM Singh S, Callis-Duffin K, et al.. International Dermatology Outcome Measures (IDEOM) group 2016 New York meeting: meeting summary and data from the Psoriasis Working Group. J Drugs Dermatol. 2017;16(8):770–77.
Strohal R, Prinz JC, Girolomoni G, Nast A. A patient-centred approach to biological treatment decision making for psoriasis: an expert consensus. J Eur Acad Dermatol Venereol. 2015;29(12):2390–8. https://doi.org/10.1111/jdv.13248.
Blome C, Gosau R, Radtke MA, Reich K, Rustenbach SJ, Spehr C, et al. Patient-relevant treatment goals in psoriasis. Arch Dermatol Res. 2016;308(2):69–78. https://doi.org/10.1007/s00403-015-1613-8.
Okubo Y, Tsuruta D, Tang AC, et al. Analysis of treatment goal alignment between Japanese psoriasis patients and their paired treating physicians. J Eur Acad Dermatol Venereol. 2018;32(4):606–14. https://doi.org/10.1111/jdv.14630.
Ahn CS, Culp L, Huang WW, Davis SA, Feldman SR. Adherence in dermatology. J Dermatolog Treat. 2016. https://doi.org/10.1080/09546634.2016.1181256.
Belinchon I, Rivera R, Blanch C, Comellas M, Lizan L. Adherence, satisfaction and preferences for treatment in patients with psoriasis in the European Union: a systematic review of the literature. Patient Prefer Adherence. 2016;10:2357–67. https://doi.org/10.2147/PPA.S117006.
Thorneloe RJ, Bundy C, Griffiths CE, Ashcroft DM, Cordingley L. Nonadherence to psoriasis medication as an outcome of limited coping resources and conflicting goals: findings from a qualitative interview study with people with psoriasis. Br J Dermatol. 2017;176(3):667–76. https://doi.org/10.1111/bjd.15086.
Coates LC, Moverley AR, McParland L, et al. Effect of tight control of inflammation in early psoriatic arthritis (TICOPA): a UK multicentre, open-label, randomised controlled trial. Lancet. 2015;386(10012):2489–98. https://doi.org/10.1016/S0140-6736(15)00347-5.
Mrowietz U, Kragballe K, Reich K, et al. Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch Dermatol Res. 2011;303(1):1–10. https://doi.org/10.1007/s00403-010-1080-1.
Armstrong AW, Siegel MP, Bagel J, et al. From the medical board of the national psoriasis foundation: treatment targets for plaque psoriasis. J Am Acad Dermatol. 2016. https://doi.org/10.1016/j.jaad.2016.10.017.
Gulliver W, Lynde C, Dutz JP, et al. Think beyond the skin: 2014 Canadian expert opinion paper on treating to target in plaque psoriasis. J Cutan Med Surg. 2015;19(1):22–7. https://doi.org/10.2310/7750.2014.13151.
Baker C, Mack A, Cooper A, et al. Treatment goals for moderate to severe psoriasis: an Australian consensus. Australas J Dermatol. 2013;54(2):148–54. https://doi.org/10.1111/ajd.12014.
Duarte GV, Porto-Silva L. de Oliveira MD (2015) Epidemiology and treatment of psoriasis: a Brazilian perspective. Psoriasis (Auckl). 2015;5:55–64.
Hernandez-Vasquez A, Molinari L, Larrea N, Ciapponi A. Psoriasis in Latin America and the Caribbean: a systematic review. J Eur Acad Dermatol Venereol. 2017;31(12):1991–8. https://doi.org/10.1111/jdv.14393.
Ministry of Health Malaysia. Clinical practice guidelines: management of Psoriasis vulgaris. Putrajaya: Malaysia Health Technology Assessment Section, Ministry of Health Malaysia; 2013.
Elewski BE, Puig L, Mordin M, et al. Psoriasis patients with psoriasis Area and Severity Index (PASI) 90 response achieve greater health-related quality-of-life improvements than those with PASI 75-89 response: results from two phase 3 studies of secukinumab. J Dermatolog Treat. 2017;28(6):492–99. https://doi.org/10.1080/09546634.2017.1294727.
Basra MK, Salek MS, Camilleri L, Sturkey R, Finlay AY. Determining the minimal clinically important difference and responsiveness of the dermatology life quality index (DLQI): further data. Dermatology. 2015;230(1):27–33. https://doi.org/10.1159/000365390.
Kimball A, Sundaram M, Mulani PM, Bao Y. Quality of life effects of psoriasis skin symptoms affecting different body regions. J Am Acad Dermatol; 2012;66(4)[Suppl 1]:AB202.
Basra MK, Sue-Ho R, Finlay AY. The family dermatology life quality index: measuring the secondary impact of skin disease. Br J Dermatol. 2007;156(3):528–38. https://doi.org/10.1111/j.1365-2133.2006.07617.x.
Basra MK, Zammit AM, Kamudoni P, Eghlileb AM, Finlay AY, Salek MS. PFI-14(c): a rasch analysis refinement of the psoriasis family index. Dermatology. 2015;231(1):15–23. https://doi.org/10.1159/000379748.
Martinez-Garcia E, Arias-Santiago S, Valenzuela-Salas I, Garrido-Colmenero C, Garcia-Mellado V, Buendia-Eisman A. Quality of life in persons living with psoriasis patients. J Am Acad Dermatol. 2014;71(2):302–7. https://doi.org/10.1016/j.jaad.2014.03.039.
Golics CJ, Basra MK, Finlay AY, Salek S. The development and validation of the Family Reported Outcome Measure (FROM-16)(c) to assess the impact of disease on the partner or family member. Qual Life Res. 2014;23(1):317–26. https://doi.org/10.1007/s11136-013-0457-y.
Gordon KB, Colombel JF, Hardin DS. Phase 3 trials of ixekizumab in moderate-to-severe plaque psoriasis. N Engl J Med. 2016;375(21):2102. https://doi.org/10.1056/NEJMc1610828.
Thaci D, Blauvelt A, Reich K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015;73(3):400–9. https://doi.org/10.1016/j.jaad.2015.05.013.
Papp KA, Reich K, Paul C, et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2016;175(2):273–86. https://doi.org/10.1111/bjd.14493.
Papp KA, Blauvelt A, Bukhalo M, et al. Risankizumab versus Ustekinumab for moderate-to-severe plaque psoriasis. N Engl J Med. 2017;376(16):1551–60. https://doi.org/10.1056/NEJMoa1607017.
Papp K, Thaci D, Reich K, et al. Tildrakizumab (MK-3222), an anti-interleukin-23p19 monoclonal antibody, improves psoriasis in a phase IIb randomized placebo-controlled trial. Br J Dermatol. 2015;173(4):930–9. https://doi.org/10.1111/bjd.13932.
Blauvelt A, Papp KA, Griffiths CE, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. J Am Acad Dermatol. 2017;76(3):405–17. https://doi.org/10.1016/j.jaad.2016.11.041.
Gordon KB, Armstrong AW, Menter MA, Wu JJ. Treating to target—a realistic goal in psoriasis? Semin Cutan Med Surg. 2018;37(2S):S44–7. https://doi.org/10.12788/j.sder.2018.010.
Feldman SR, Bushnell DM, Klekotka PA, et al. Differences in psoriasis signs and symptom severity between patients with clear and almost clear skin in clinical practice. J Dermatol Treat. 2016;27(3):224–7. https://doi.org/10.3109/09546634.2015.1093589.
Papp K, Menter A, Poulin Y, Gu Y, Sasso EH. Long-term outcomes of interruption and retreatment vs. continuous therapy with adalimumab for psoriasis: subanalysis of REVEAL and the open-label extension study. J Eur Acad Dermatol Venereol. 2013;27(5):634–42. https://doi.org/10.1111/j.1468-3083.2012.04515.x.
Poulin YOM, Sheth P, Gu Y. Psoriasis patients required to discontinue adalimumab therapy have worsening in their quality of life out of proportion to worsening in the objective signs of disease: Subanalysis of REVEAL. J Am Acad Dermatol. 2012;66(4)[Suppl 1]:AB201. https://doi.org/10.1016/j.jaad.2011.11.841
Warren RB, Smith CH, Yiu ZZ, et al. Differential drug survival of biologic therapies for the treatment of psoriasis: a prospective observational cohort study from the british association of dermatologists biologic interventions register (BADBIR). J Invest Dermatol. 2015;135(11):2632–40. https://doi.org/10.1038/jid.2015.208.
Davila-Seijo P, Dauden E, Carretero G, et al. Survival of classic and biological systemic drugs in psoriasis: results of the BIOBADADERM registry and critical analysis. J Eur Acad Dermatol Venereol. 2016;30(11):1942–50. https://doi.org/10.1111/jdv.13682.
Menter A, Papp KA, Gooderham M, et al. Drug survival of biologic therapy in a large, disease-based registry of patients with psoriasis: results from the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Eur Acad Dermatol Venereol. 2016. https://doi.org/10.1111/jdv.13611.
Schaeverbeke T, Truchetet ME, Kostine M, Barnetche T, Bannwarth B, Richez C. Immunogenicity of biologic agents in rheumatoid arthritis patients: lessons for clinical practice. Rheumatology (Oxford). 2016;55(2):210–20. https://doi.org/10.1093/rheumatology/kev277.
Jani M, Barton A, Warren RB, Griffiths CE, Chinoy H. The role of DMARDs in reducing the immunogenicity of TNF inhibitors in chronic inflammatory diseases. Rheumatology (Oxford). 2014;53(2):213–22. https://doi.org/10.1093/rheumatology/ket260.
Gniadecki R, Bang B, Bryld LE, Iversen L, Lasthein S, Skov L. Comparison of long-term drug survival and safety of biologic agents in patients with psoriasis vulgaris. Br J Dermatol. 2015;172(1):244–52. https://doi.org/10.1111/bjd.13343.
Gyulai R, Bagot M, Griffiths CE, et al. Current practice of methotrexate use for psoriasis: results of a worldwide survey among dermatologists. J Eur Acad Dermatol Venereol. 2015;29(2):224–31. https://doi.org/10.1111/jdv.12495.
Warren RB, Mrowietz U, von Kiedrowski R, et al. An intensified dosing schedule of subcutaneous methotrexate in patients with moderate to severe plaque-type psoriasis (METOP): a 52 week, multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10068):528–37. https://doi.org/10.1016/S0140-6736(16)32127-4.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–34.
Simpson JK, Wilson M, Ahmed AA, Mizara A, Clarke A, McBride SR. An exploratory study to investigate health-seeking behaviour in patients with psoriasis using framework analysis. Br J Dermatol. 2017. https://doi.org/10.1111/bjd.15307.
Gottlieb AB, Greb JE, Goldminz AM. Psoriasis trends and practice gaps. Dermatol Clin. 2016;34(3):235–42. https://doi.org/10.1016/j.det.2016.03.004.
Kaushik SB, Lebwohl MG. CME part I psoriasis: which therapy for which patient psoriasis comorbidities and preferred systemic agents. J Am Acad Dermatol. 2018. https://doi.org/10.1016/j.jaad.2018.06.057.
Kaushik SB, Lebwohl MG. CME part II psoriasis: which therapy for which patient focus on special populations and chronic infections. J Am Acad Dermatol. 2018. https://doi.org/10.1016/j.jaad.2018.06.056.
Boutayeb A, Boutayeb S. The burden of non communicable diseases in developing countries. Int J Equity Health. 2005;4(1):2. https://doi.org/10.1186/1475-9276-4-2.
Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191–9. https://doi.org/10.1016/j.trstmh.2005.07.021.
DeCoster E, Alves de Medeiros A, et al. A multileveled approach in psoriasis assessment and follow-up: a proposal for a tailored guide for the dermatological practice. J Dermatolog Treat. 2016;27(4):298–310. https://doi.org/10.3109/09546634.2015.1117566.
Hoffman MB, Hill D, Feldman SR. Current challenges and emerging drug delivery strategies for the treatment of psoriasis. Expert Opin Drug Deliv. 2016;13(10):1461–73. https://doi.org/10.1080/17425247.2016.1188801.
Acknowledgements
Funding
Celgene, Novartis, Eli Lilly, and AbbVie provided corporate sponsorship to the International Psoriasis Council for the round table event. These sponsors had no influence on the content and viewpoints in this manuscript. Article processing charges were funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
BE Strober received honoraria for serving as a consultant, advisory board member, and/or speaker for AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol-Myers-Squibb, Celgene, Dermavant, Dermira, Janssen, Leo, Eli Lilly, Leo, Medac, Meiji Seika Pharma, Sebela Pharmaceuticals, Menlo Therapeutics, Novartis, Pfizer, GlaxoSmithKline, UCB Pharma, Sirtris, Sun Pharma, Ortho Dermatologics/Valeant, Regeneron, and Sanofi-Genzyme. Investigator funding (no direct payments made to BE Strober) received from: AbbVie, Celgene, Eli Lilly, Janssen, Merck, Boehringer Ingelheim, GlaxoSmithKline, Pfizer, Galderma, Sienna Bio Scientific Director (consulting fee); CORRONA Psoriasis Registry. Grant support to the University of Connecticut for Fellowship Program (payments to the University of Connecticut, not BE Strober): AbbVie, Janssen, National Psoriasis Foundation. JM van der Walt has no disclosures to declare. AW Armstrong acted as consultant to AbbVie, Amgen, Janssen, Merck, Eli Lilly, Novartis, Pfizer, Celgene; received grants from AbbVie, Janssen, and Eli Lilly, and received honorarium from AbbVie and Eli Lilly. M Bourcier acted as consultant, speaker, or principal investigator for Abbie, Amgen, Eli Lilly, Janssen, Leo, Merck, Novartis, Pfizer, and Valeant. AVE Carvalho acted as advisory Board member for Novartis, Jansen, and Eli Lilly and as a speaker for Novartis, Jansen, Eli Lilly, and Pfizer. E Chouela acted as consultant, speaker, and principal investigator for Pfizer, Abbie, Novartis, Lilly, and Galderma. AD Cohen received research grants from Janssen, Novartis, AbbVie, and Sanofi; served as a consultant, advisor, or speaker to AbbVie, Amgen, Boehringer Ingelheim, Dexcel Pharma, Janssen, Kamedis, Lilly, Neopharm, Novartis, Perrigo, Pfizer, Rafa, Sanofi, Sirba, and Taro. C de la Cruz served as speaker and principal investigator to Lilly, Pfizer, Abbvie, Janssen, Novartis, and Amgen. CN Ellis has served as a consultant for AbbVie, Celgene, Gilead, GlaxoSmithKline, Johnson & Johnson, Eli Lilly, and Novartis. AY Finlay is joint copyright owner of the DLQI, PDI, PFI, FDLQI, and FROM-16. Cardiff University and AY Finlay receive royalties. AY Finlay has contributed to Novartis, Sanofi, Napp, and Galderma advisory boards. AB Gottlieb has Current Consulting/Advisory Board Agreements with Janssen Inc., Celgene Corp., Bristol Myers Squibb Co., Beiersdorf, Inc., Abbvie, UCB, Novartis, Incyte, Lilly, Reddy Labs, Valeant, Dermira, Allergan, and Sun Pharmaceutical Industries, and Research/Educational Grants from Janssen Incyte. J Gudjonsson received research support from SunPharma, Amgen, Novartis, Pfizer, and AbbVie and contributed to Novartis advisory board. L Iversen served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Admiral, Amgen, Celgene, Centocor, Eli Lilly, Janssen Cilag, Leo Pharma, MSD, Novartis, Pfizer, UCB, BMS, and Boehringer Ingelheim. CE Kleyn received research funding from Pfizer, Janssen, and Johnson & Johnson and honoraria from AbbVie, Amgen, Galderma, Janssen, Leo Pharma, Stiefel/GSK, and Eli Lilly. She is a consultant for Eli Lilly. CL Leonardi is a Consultant/Advisory Board Member for Abbvie, Amgen, Boehringer-Ingelheim, Dermira, Eli Lilly, Janssen, Leo, Pfizer, Sandoz, UCB, and Vitae; investigator for Actavis, Abbvie, Amgen, Boehringer-Ingelheim, Celgene, Coherus, Cellceutix, Corrona, Dermira, Eli Lilly, Galderma, Glenmark, Janssen, Leo Pharma, Merck, Novartis, Novella, Pfizer, Sandoz, Stiefel, and Wyeth; speaker bureau for Abbvie, Celgene, Novartis, and Eli Lilly. CW Lynde received honoraria or research grants from Allergan, Amgen, AbbVie, Astellas, Celgene, Eli Lilly, Galderma, Janssen, Leo Pharma, Pfizer Merck, Stiefel/GSK, and Novartis. C Ryan has received honoraria for her role as a consultant or speaker for AbbVie, Boehringer Ingelheim, Dermira, Dr. Reddy’s Laboratories, Janssen, Leo, Lilly, Medimetriks, Novartis, Regeneron/Sanofi, and UCB Pharma. CT Theng has no conflicts of interest to declare. F Valenzuela acted as a principal investigator, member of a scientific advisory board and/or speaker for AbbVie, Amgen, Eli Lilly, Janssen, Merck, Novartis, and Pfizer Inc. R Vender has received grants/research support from Abbvie, Amgen, Centocor, Dermira, Galderma, GSK, Leo, Lilly, Takeda, Novartis, Merck, Pfizer, Regeneron; honoraria from Abbvie, Amgen, Janssen, Galderma, GSK, Leo, Lilly. Novartis, Pfizer, Valeant, Actelion, Celgene, Cipher, Palladin; consulting fees from Abbvie, Amgen, Janssen, Galderma, GSK, Leo, Lilly, Novartis, Pfizer, Valeant, Actelion, Celgene, Cipher, and Palladin. JJ Wu is an investigator for AbbVie, Amgen, Eli Lilly, Janssen, Novartis, and Regeneron. HS Young acted as a consultant or speaker or had research funding to/from Abbott/Abbvie, Almirall, Amgen, Janssen, Leo-Pharma, Lilly, MEDA, Novartis, Stiefel, and UCB Pharma. AB Kimball is a consultant for Novartis, Abbvie, Dermira, UCB, Lilly, and Janssen and has received fellowship funding from Janssen and Abbvie.
Compliance with Ethics Guidelines
This article does not contain any studies with human participants or animals performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7436702.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Strober, B.E., van der Walt, J.M., Armstrong, A.W. et al. Clinical Goals and Barriers to Effective Psoriasis Care. Dermatol Ther (Heidelb) 9, 5–18 (2019). https://doi.org/10.1007/s13555-018-0279-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-018-0279-5