Abstract
Sleep dysfunction is highly prevalent across the spectrum of neurodegenerative conditions and is a key determinant of quality of life for both patients and their families. Mounting recent evidence also suggests that such dysfunction exacerbates cognitive and affective clinical features of neurodegeneration, as well as disease progression through acceleration of pathogenic processes. Effective assessment and treatment of sleep dysfunction in neurodegeneration is therefore of paramount importance; yet robust therapeutic guidelines are lacking, owing in part to a historical paucity of effective treatments and trials. Here, we review the common sleep abnormalities evident in neurodegenerative disease states and evaluate the latest evidence for traditional and emerging interventions, both pharmacological and nonpharmacological. Interventions considered include conservative measures, targeted treatments of specific clinical sleep pathologies, established sedating and alerting agents, melatonin, and orexin antagonists, as well as bright light therapy, behavioral measures, and slow-wave sleep augmentation techniques. We conclude by providing a suggested framework for treatment based on contemporary evidence and highlight areas that may emerge as major therapeutic advances in the near future.
Similar content being viewed by others
Introduction
Sleep dysfunction is prominent across the spectrum of neurodegenerative conditions, occurring in 40 to 90% of patients [1,2,3,4,5]. It is a key determinant of patients’ quality of life [6], falls risk [7], and progression to institutionalization [8,9,10,11], as well as caregiver burden and health [12,13,14]. It should therefore be a priority in the clinical care of patients with neurodegenerative disease but is currently typically overlooked.
Moreover, mounting recent evidence contends that sleep dysfunction contributes to the severity and progression of neurodegeneration [15]. On a symptomatic level, it is well-established that sleep deprivation and disruption leads to deficits in attention, executive function, and processing speed, as well as promoting impulsivity, emotional lability, and depression [16,17,18,19,20]. Sleep abnormalities therefore almost certainly contribute to the burden of such features common to neurodegenerative conditions. Importantly, however, exacerbation may also occur at the level of the underlying pathogenic processes. The discovery of the glymphatic pathway and its predominant activity during sleep [21,22,23], for example, has revealed the critical role of sleep in the clearance of extracellular neurotoxic waste linked to some forms of neurodegeneration. Clearance of both β-amyloid and tau has been shown to occur in this way [24, 25], and sleep deprivation has been shown to effect marked, rapid increases in these pathogenic protein species in both animal models [26, 27] and humans [28,29,30]. Likewise, sleep deprivation has been shown to promote tau propagation [27] and induce neuroinflammation [31], both of which have been implicated in neurodegenerative pathophysiology. Other recent studies have also revealed in detail the role of sleep in memory consolidation through synaptic modelling and the formation of cortical engrams [32,33,34]. Impairment of sleep is thus very likely to contribute to the synaptic dysfunction and memory impairment characterizing many neurodegenerative conditions.
Addressing sleep dysfunction in neurodegeneration is therefore of critical importance, offering potential to not only enhance quality of life for patients and their families, but also to mitigate disease burden and delay progression. Given the lack of therapies that currently achieve this for neurodegenerative conditions, this potential is of paramount significance.
Here, we review the latest evidence for traditional and emerging sleep therapies in neurodegeneration, both pharmacological and nonpharmacological. Reflecting the weight of available literature, considered evidence relates predominantly to Alzheimer’s and Parkinson’s disease, but, where available, is also discussed in relation to Huntington’s disease, Lewy body dementia, and vascular dementia.
Sleep Dysfunction in Neurodegenerative Conditions: Commonalities and Discriminators
Important commonalities are present among neurodegenerative conditions with regard to the nature of sleep dysfunction. Insomnia, in the form of delayed sleep onset, fragmentation, or early awakening difficulties, is a prevalent abnormality affecting around 50% of patients [4] and is convergent across the spectrum of neurodegenerative disease [4, 35, 36]. Circadian dysfunction is also common throughout, as evidenced by loss of robust rest–activity rhythms, abnormalities of melatonin concentration and rhythmicity, and loss of autonomic diurnal fluctuation [37, 38]. Likewise, where sleep architecture is analyzed via polysomnography, a characteristic pattern of abnormalities emerges; that of increased arousals/awakenings, loss of slow-wave and rapid eye movement (REM) sleep stages, increased latency to initiation of REM, and consequent gain in time spent in the lightest stages of sleep [35, 39,40,41]. It is also notable that, across the spectrum of neurodegenerative disease, sleep abnormalities frequently precede diagnostic clinical features: for example, sleep fragmentation precedes the onset of overt Alzheimer’s disease and manifest Huntington’s disease [42, 43] and REM behavior sleep disorder (RBD) often precedes the clinical onset of motor features of Parkinson’s, multiple system atrophy, or Lewy body dementia [44, 45].
Nevertheless, important discriminators are also evident. For example, obstructive sleep apnea (OSA) is notably prevalent in Alzheimer’s disease, affecting 40% of patients [46, 47], and is the predominant abnormality seen in vascular dementia [48]. By contrast, restless leg syndrome (RLS) and RBD are more prevalent in Parkinson’s disease, affecting 15 and 35 to 46% patients respectively [2, 5, 49], with rates of RBD in multiple system atrophy and Lewy body dementia being even higher [35]. While daytime sleepiness and sundowning are prominent in Alzheimer’s disease, true excessive daytime sleepiness and sleep attacks typify Parkinson’s disease [5, 50]. Periodic limb movement disorder, meanwhile, is seen more commonly in Huntington’s disease [51].
These parallels and discrepancies likely reflect the underlying pathology of neurodegeneration. Commonalities are likely driven by shared neurodegenerative patterns of hypothalamic involvement leading to circadian dysfunction, and generalized atrophy leading to an inability to gate and support sleep stages appropriately. By contrast, discriminators likely reflect relative patterns of disease burden, for example, a brainstem emphasis in Parkinson’s disease, versus basal forebrain dysfunction in Alzheimer’s [52].
Preliminary Therapeutic Considerations
It is vital that the process of addressing sleep dysfunction in a patient with neurodegeneration begins with a comprehensive assessment of the specific problems in question. For an excellent recent review of appropriate questions, validated scales, and objective investigations such as sleep studies and actigraphy to aid in this process, please see the recent review by Ooms and Ju [48]. This process will help ensure identification of specific clinical sleep pathologies where present and recognition of preliminary contributory factors to sleep dysfunction such as depression, pain, nocturia, medications, and caffeine/nicotine/alcohol use. It is imperative that such elements are addressed first, prior to consideration of other strategies.
Depression
Depression is highly prevalent in neurodegeneration [53], and while the relationship between depression and sleep dysfunction is bidirectional, it is well recognized that depression frequently leads to initiation and maintenance insomnia, as well as sleep architectural disturbance including a loss of slow-wave sleep [54]. Treating depression in Parkinson’s disease has been associated with improvements in sleep symptoms [55, 56]. Therefore, where depression and sleep dysfunction are concomitant and the severity of depression mandates treatment, it is prudent to consider such treatment prior to other sleep interventions. However, attention should be paid to the selection of antidepressant: selective serotonin reuptake inhibitors and venlafaxine can impair sleep quality, whereas agents such as trazodone and mirtazapine promote sleep [54], and antidepressants can exacerbate clinical sleep pathology (Table 1).
Pain
Contributory pain, for example due to comorbid osteoarthritis, should be addressed with analgesics. Discomfort due to rigidity/akinesia, dystonia, and impaired bed mobility in Parkinson’s disease are commonly thought to contribute to sleep dysfunction [60], such that dopaminergic therapy may be of benefit [61]. However, some studies effecting specific improvement in these features have failed to show concomitant improvement in sleep quality [62, 63].
Nocturia
Nocturia is a prominent cause of sleep disruption in Parkinson’s disease, affecting around 35 to 66% of individuals [5, 49], but is also a contributory factor in many patients with other neurodegenerative conditions often secondary to age-related comorbid conditions such as benign prostatic hypertrophy or heart failure. Simple measures such as the optimization of timing of diuretics, reduction of water intake from late afternoon, or convene catheter systems can therefore be of significant benefit to many patients with disrupted sleep. In the setting of Parkinson’s, optimization of dopaminergic therapy may effect improvement in nocturia [64, 65], particularly the nocturnal use of rotigotine patches [66]. Anticholinergic interventions for nocturia, however, should be viewed with caution due to their well-documented deleterious cognitive side effects.
Influence of Medications for Comorbidities
The contribution of medications for comorbid conditions should also be considered. For example, α-blockers, β-blockers, corticosteroids, serotonin selective reuptake inhibitors, and angiotensin-converting enzyme inhibitors all have detrimental effects on sleep and should therefore be rationalized in the setting of sleep dysfunction.
Influence of Medications for Neurodegenerative Conditions
The contribution of medications administered for the neurodegenerative condition itself should also be considered, especially with respect to timing and dose. For example, donepezil and memantine administered for Alzheimer’s have been shown to improve sleep quality overall [67, 68] but donepezil may cause sleep disruption if taken late in the day [69]; modification of timing may therefore bring benefit. Likewise, dopamine agonists improve sleep quality and daytime functioning in Parkinson’s [70, 71] but carry a dose-related risk of excessive daytime somnolence and sleep attacks; therefore, dosing should be reviewed in the setting of sleep dysfunction.
Caffeine, Nicotine, and Alcohol Exposure
Exposure to caffeine, alcohol, or nicotine less than 4 h prior to going to bed is associated with poor sleep quality; patients’ use of such items should therefore also be reviewed and addressed. Particular effort should be made to probe alcohol use accurately, as 26% of elderly individuals with sleep problems have reported self-medicating with alcohol for sleep induction [72], and alcohol abuse is frequent in neurodegenerative conditions that promote addictive behaviors/impulse control disorders.
Treatment of Clinical Sleep Pathology
Alongside such considerations, clinical sleep pathology such as OSA, RLS, PLMD, or RBD should be addressed in a targeted way where present. This is vital, as such factors make a significant contribution to overall sleep dysfunction: for example, RLS frequently leads to sleep onset insomnia, and OSA and PLMD may contribute to sleep fragmentation and daytime sleepiness [73, 74]. This is also important as highly effective interventions are available: for example, continuous positive airway pressure (CPAP) for OSA has been shown not only to improve sleep quality, but also to enhance mood and cognition, and slow cognitive decline in Alzheimer’s disease [75,76,77,78]. The treatment of such pathology has been recently reviewed in detail elsewhere [49], but a framework of key strategies is provided in Table 1.
Where such interventions are unsuccessful in effecting sufficient improvement in sleep dysfunction, further pharmacological and nonpharmacological strategies should be considered. Herein we evaluate current evidence in these two domains.
Pharmacological Therapies
Sedating and Alerting Agents
A number of hypnotic agents, including benzodiazepines, Z-drugs, and sedating antidepressants and antihistamines, are frequently used to treat insomnia in healthy adults. However, such agents are almost exclusively only approved for short-term use and are recommended as a secondary measure to nonpharmacological approaches. This is because i) all such agents bear limited efficacy and salient risk of significant adverse effects and ii) there is insufficient evidence to balance benefits against such risks for long-term use in healthy adults [79]. There is even less scope to contend that benefits outweigh such risks in older individuals or patients with neurodegenerative disorders: as outlined below, robust randomized controlled trials are sparse, and extrapolation from observational studies suggests that risks are likely to be more prominent in such populations.
Benzodiazepines and Z-Drugs
Both benzodiazepines, such as temazepam, nitrazepam, and triazolam, and Z-drugs, such as zopiclone, zolpidem, and zaleplon, improve sleep quality by reducing sleep latency and awakenings via agonism of GABAA receptors, the main inhibitory neurotransmitter receptors in the brain. Adverse effects of benzodiazepines include tolerance, dependence, and withdrawal, as well as both acute [80, 81] and chronic [82] impairment of attention and psychomotor speed. Impairment of memory consolidation is also well supported, although refuted by some studies [83,84,85]. While risks of such adverse effects are lower with Z-drugs, they are not absent [86, 87]. Moreover, both benzodiazepines and Z-drugs have been found to reduce REM and/or slow-wave sleep [88,89,90], stages of sleep vital to memory consolidation [32,33,34] and glymphatic clearance of neurotoxic waste [21].
In line with these observations, among elderly populations, benzodiazepines and Z-drugs are consistently associated with an increased risk of hip fracture due to falls [91], and some evidence suggests an increased risk of cognitive impairment [92] and decline [93]. Likewise, in an observational study in a probable Alzheimer’s cohort adjusted for baseline cognitive function and confounding clinical features [94], use of benzodiazepines was associated with a higher risk of deterioration. In Parkinson’s disease, a small placebo-controlled study of eszopiclone identified improved subjective sleep measures without marked adverse events [55], but with a treatment period of only 6 weeks. High-quality evidence among neurodegeneration-specific cohorts is otherwise lacking.
Thus, it is highly likely that use of such agents in a neurodegenerative population will bring harm in excess of benefit and should therefore be viewed with caution.
Sedating Antihistamines and Antidepressants
Sedating antihistamines such as diphenhydramine and hydroxyzine are some of the most frequently used agents in individuals with insomnia, in part due to their availability in over-the-counter preparations. However, the mixed antihistamine/anticholinergic effect of such agents can cause prominent sedation, cognitive impairment, delirium, and increased daytime somnolence, such that avoidance is recommended in a neurodegenerative population [95,96,97].
Sedating antidepressants, such as amitryptiline, trazodone, mirtazapine, and doxepin, are also commonly used in the treatment of insomnia. Of note, trazodone has shown neuroprotective effects and rescue of memory deficits in preclinical models of neurodegeneration [98]. However, the majority of such antidepressants bear the same potential for deleterious outcomes as antihistamines, due to mixed anticholinergic and/or antihistamine effects. In line with this, observational studies in older individuals have identified the use of such agents as associated with increased risk of both hip fracture [99] and mortality [100]. A small blinded placebo-controlled trial of trazodone in an Alzheimer’s disease cohort found an improvement in total sleep time without prominent adverse events or cognitive impairment [101]. However, the treatment period was only 2 weeks, this finding has not been replicated in other studies, and, indeed, a number of other studies have identified trazodone as bearing prominent risks of cognitive impairment [102] and adverse outcomes [100]. Alongside this, a randomized controlled trial of mirtazapine in Alzheimer’s has found no benefit to sleep or cognitive outcomes, with an increase in daytime drowsiness [103]. It is therefore recommended that such agents are avoided for sleep therapy except where depression is concomitant and requires pharmacological intervention. Nevertheless, some more favorable evidence is present for doxepin: a 12-week double-blind controlled study in elderly individuals with chronic primary insomnia identified objective sleep benefit without prominent adverse effects [104], and an open-label study in a Parkinson’s cohort identified improved cognitive and subjective sleep outcomes without major adverse effect [105], although the treatment period was only 6 weeks. Again, however, these findings have yet to be replicated or trialled in larger cohorts, and as such this evidence has to be seen to be as inconclusive at this stage.
Antipsychotics
Antipsychotics represent a further class of agents that have been used in the treatment of sleep dysfunction in neurodegeneration, typically capitalizing upon their hypnotic effect when administered for behavioral and psychological symptoms of dementia (BPSD). Short-term randomized studies have supported their ability to significantly increase total sleep time in patients with dementia [106], and a 5-year observational study in Alzheimer’s disease comparing outcomes from risperidone versus zolpidem, melatonin, or no treatment found superior outcomes within the risperidone subgroup [107]. However, this is contradicted by the appropriately adjusted observational study conducted by Ellul et al. [94], in which antipsychotics were associated with greater deterioration in patients with Alzheimer’s, and is at odds with a weight of evidence suggesting that antipsychotics carry an increased risk of hip fracture [99], cognitive decline, cerebrovascular accident, and death [99, 108,109,110] among patients with dementia. It is therefore not recommended that such agents are used to address sleep dysfunction, unless they already mandated for concomitant BPSD. Where this is needed, there is some evidence to suggest that quetiapine carries a lower risk of adverse effects than other antipsychotics, but this is tempered by concurrent lower efficacy for treating BPSD [111].
Sodium Oxybate
Sodium oxybate, an agent used in the treatment of narcolepsy and thought to act via GABAergic mechanisms, is attracting growing interest as a possible alternative pharmacological agent for the treatment of sleep dysfunction in neurodegeneration. Not only has it been found to enhance slow-wave activity and counteract the cognitive effects of sleep deprivation in healthy adults [112], it has also shown promising effects on toxic proteinopathies, neuroprotection, and neuroinflammation in animal models of neurodegeneration [113]. Moreover, in Parkinson’s disease, both open-label [114] and small randomized controlled trials [115] have identified both subjective and objective sleep improvement following its use. Nonetheless, de novo sleep apnea or parasomnia was induced in 3/12 participants [115], long-term use in a neurodegenerative cohort has yet to be assessed, and its proposed GABAergic mode of action raises the potential that this agent will have similar problems to those seen with benzodiazepines and Z-drugs.
Modafinil
Some studies have considered the converse approach to addressing sleep dysfunction in neurodegeneration, by administering the alerting agent modafinil during waking hours. However, evidence to date has not supported its use: modafinil has failed to show consistent benefit for fatigue [116] or daytime somnolence [114, 117, 118] in Parkinson’s disease or for apathy in Alzheimer’s disease [119]. A small randomized controlled acute single-dose trial in Huntington’s disease identified some improvement in alertness, but with no improvement to mood, and deleterious cognitive effects [120].
Melatonin
Melatonin, the hormone that helps orchestrate circadian sleep–wake function, has received considerable research interest as a further alternative pharmacological agent for the treatment of sleep dysfunction in neurodegeneration. Exogenous melatonin administration can influence both circadian rhythm and sleep quality [121], and the reduction in release of endogenous melatonin across the spectrum of neurodegeneration [37] would suggest that administration may have a beneficial normalizing effect. Moreover, preclinical studies have suggested that melatonin could have an independent antioxidant, anti-inflammatory, and neuroprotective role [122], and one of promoting glymphatic clearance [123] of neurotoxic waste.
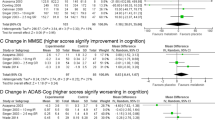
However, while a number of studies have suggested a benefit of melatonin therapy in Alzheimer’s disease, the great majority of these are open-label studies and based on subjective outcomes [124,125,126,127]. Of the five robust randomized controlled trials in Alzheimer’s disease employing objective outcomes based on actigraphic sleep variables, the evidence is inconclusive. Three have failed to show benefit to any sleep variable [128,129,130], while two have demonstrated mixed benefit: Asayama et al. [131] reported a significant increase in total sleep time (mean, 103 min) with decreased nocturnal activity, while Dowling at al. [132] reported improved rest–activity rhythm, but only through improvements in wake activity rather than sleep, and only when administered in conjunction with light therapy. This lack of consensus may relate to the wide range of melatonin doses employed in these studies. The cognitive benefit of melatonin therapy in Alzheimer’s disease has been reported in two studies [131, 133] but the extent of this is of questionable clinical significance: a change of 1.5 out of a total of 30 points on the Mini-Mental State Examination (MMSE) and 3.5 to 4.3 out of a scale of 70 points on the Alzheimer’s Disease Cognitive Assessment Scale (ADAS-Cog).
Only one robust study of melatonin therapy has been undertaken in mild cognitive impairment. This double-blind placebo cross-over study [134] suggested improvement in both sleep quality and rest–activity rhythms as reported by actigraphy outcomes, as well as benefits to depression and cognition, but to our knowledge this finding has not been reproduced in any other study to date.
Very limited high-quality data is available as to the value of melatonin therapy in Parkinson’s disease. Of studies available in English, there has been one placebo-controlled trial with actigraphic outcomes [135] which demonstrated no benefit other than a gain of just 10 min of total sleep time, while a randomized double-blind placebo-controlled trial showed no benefit on objective polysomnographic outcomes and no benefit to motor symptoms [136]. However, a recent evidence-based review [137] has found melatonin to be “possibly useful” in the treatment of insomnia in Parkinson’s, on the basis of i) positive studies employing subjective sleep outcomes and ii) melatonin’s low side effect profile.
Overall, meta-analyses evaluating the effect of melatonin on Alzheimer’s, Parkinson’s, or mixed dementia have found no benefit to any sleep or cognitive variable [138, 139], other than two reporting a modest, likely clinically insignificant increase in total sleep time: 24 min [140] and 33 min [141].
However, these findings should not be conflated with those pertaining to RBD, where there is a strong evidence base for the efficacy of melatonin: open-label prospective [57, 59], retrospective [58], and double-blind placebo-controlled [142] studies have all suggested significant scope for melatonin therapy to reduce RBD episodes, as confirmed by polysomnographic outcomes.
Orexin Antagonists
Orexin, also known as hypocretin, is a key hypothalamic neuropeptide regulating sleep by promoting wakefulness and arousal. The recent development of pharmacological orexin antagonists for clinical use therefore represents an emerging avenue of sleep therapy bearing potential in neurodegeneration [52, 143]. In addition, preclinical studies in mice have suggested that orexin antagonism can also suppress β-amyloid accumulation [144].
Two phase 3 trials of orexin antagonists [145, 146] have produced moderately promising results in the treatment of primary insomnia, increasing total sleep time (55 min treatment group vs 19 min placebo group) and reducing wake time after sleep onset (48 min treatment group vs 25 min placebo) by reducing the duration of wakeful periods. Moreover, head to head trials of orexin antagonists versus zolpidem have suggested superiority with respect to latency to persistent sleep and sleep maintenance [147] and also to cognitive outcomes [148]. Levels of somnolence appear comparable [149] and, if present, are mild–moderate and rarely require drug withdrawal [145, 146]. Sleep architecture also appears largely unaffected [145].
Encouragingly, studies involving older healthy participants have not demonstrated significantly different efficacy or safety outcomes [145, 150], and the sole trial in a neurodegenerative cohort that has been published to date has suggested strikingly similar outcomes to those in healthy cohorts. In this randomized controlled trial undertaken in patients with insomnia and mild–moderate Alzheimer’s [151], orexin antagonism was superior to placebo with respect to improvements in total sleep time (73 min vs 45 min) and wake time after sleep onset (− 45 min vs – 29 min), with no major effect on sleep architecture. Moreover, limited cognitive assessment through the Mini Mental State Examination and Symbol Digit Task did not suggest deleterious cognitive outcomes, somnolence was not prominent or severe, and while there were more falls in the treatment group (2.1% vs 0%), these were not judged to be drug related.
Nonetheless, the efficacy and safety of orexin antagonists in neurodegeneration remains to be tested robustly. Indeed, the fact that orexin levels are reduced in many neurodegenerative conditions [152, 153] may predict poor outcomes, and the central activity of orexin antagonists raises the potential for adverse events in such populations. In particular, the phase 3 studies were undertaken in cohorts that excluded depression. Given the high rates of coincidence of depression and sleep dysfunction in neurodegenerative conditions, assumptions cannot yet be extrapolated regarding safety for affective outcomes. It is also of note that, to date, orexin antagonists are only approved for clinical use in Japan, Australia, and the USA.
Nonpharmacological Interventions
Nonpharmacological sleep therapies, most notably bright light therapy and behavioral interventions, also merit consideration.
Bright Light Therapy
Light is the most powerful zeitgeber of the human circadian system [154], and bright light therapy delivered by light emitters (e.g., lightboxes) is known to affect both circadian rhythm [155, 156] and sleep quality [157] in healthy individuals. There is also a strong evidence base for its efficacy in depression [158]. The potential for bright light therapy to treat sleep dysfunction and its corollaries in neurodegeneration has therefore received considerable research attention.
The majority of studies with objective actigraphic sleep outcomes have been undertaken in mixed dementia cohorts in residential settings. Most have demonstrated a degree of benefit; many in the absence of a control arm raising the possibility of placebo effects [159,160,161], but gains have also extended to controlled studies [162,163,164]. The most common benefit has been of strengthened circadian rhythm [159, 160, 164, 165], but some studies have also demonstrated enhanced total sleep time and sleep efficiency [159, 161] and reduced wake after sleep onset [161]. Five studies have also analyzed cognitive outcomes [166,167,168,169,170]. Each demonstrated minor benefit, but outcomes were limited to Mini-Mental State Examination (MMSE) only and may have been consequent to the alerting influence of bright light rather than via changes in sleep quality. Evidence regarding the effect on behavioral features of neurodegeneration is mixed: while some studies have reported improvements in both depression and agitation alongside sleep benefit [159, 166], others have demonstrated exacerbated agitation [171].
With respect to studies in specific dementia subtypes, studies of bright light therapy in Alzheimer’s-only cohorts have demonstrated similar benefits to those in mixed dementia studies [163], while a head-to-head study of vascular dementia versus Alzheimer’s disease favored a greater benefit in vascular dementia [162]. Uncontrolled, unblinded studies in Parkinson’s disease have suggested benefit of bright light therapy to mood, motor outcomes, and subjective markers of sleep [172, 173]. However, controlled studies have found frequent parallel sleep outcomes between active and control conditions [174, 175], raising the possibility of a placebo effect.
Despite this overall positive potential, meta-analyses of bright light therapy in neurodegeneration have largely failed to recommend its use overall. While the benefits seen in most studies are acknowledged, these have been insufficient to contend significant efficacy overall [176,177,178]. One meta-analysis has advocated its use [179], but estimates a weak effect size (Hedges g = 0.3). This outcome likely relates to the same factors that limit the practical suitability of bright light therapy for patients with neurodegenerative conditions: to be both effective and comparable between studies, bright light therapy requires consistent daily use, at a consistent time tailored to the patient’s circadian rhythm, at a consistent sedentary distance to achieve uniform lux exposure, and in a season/setting where effects are not outweighed by environmental light exposure [166]. This is clearly not always feasible for patients with dementia; indeed, studies incorporating adherence analysis have reported noncompliance to be as high as 25% (155; Lazar personal communication). The development of blue light glasses [180] may circumvent some of these barriers, but have yet to be tested robustly.
Behavioral Measures
Behavioral measures, collectively known as cognitive behavioral therapy for insomnia (CBT-I) and summarized in Table 2, have a strong evidence base in improving sleep quality in healthy individuals [181].
Studies of the use of such measures in neurodegeneration have been encouraging. As for bright light therapy, the majority of evidence comes from mixed dementia cohorts, most using multicomponent techniques focusing on sleep hygiene. Almost all studies have suggested benefit, many in enhanced daytime wakefulness [182, 183], but also in reduced wake time at night [184] and sleep duration [185], confirmed both by actigraphy [182,183,184,185] and polysomnography [186, 187]. Some studies have also reported associated cognitive benefit [186] and a reduction in agitation [185, 188].
Moreover, such findings extend to Alzheimer’s specific cohorts, where both sleep hygiene alone [189] and in combination with light therapy [190, 191] have been shown to benefit sleep quality. Similarly, CBT-I has been shown to benefit sleep quality and executive function in mild cognitive impairment [192]. Akin to bright light therapy, there is a relative paucity of high-quality studies in Parkinson’s specific cohorts, with most studies employing subjective outcomes suggesting benefit [193,194,195], whereas objective measures have tended to be negative [105, 196]. Nonetheless, daytime physical exercise has been found to improve nocturnal actigraphy [197] and polysomnographic outcomes [198] in Parkinson’s.
As with bright light therapy, the application of such measures is clearly contingent upon an individual patient and/or carer’s ability to implement/engage with them consistently, which may be impractical for many patients. Adherence is key to efficacy [191], and attrition rates have been as high as 40% in community studies [199]. Furthermore, in the main, carers have been found to need tailored and patient-specific advice rather than generic guidance [200], which may limit feasibility.
A combined recent meta-analysis [176] of bright light therapy and behavioral measures in the treatment of sleep dysfunction in neurodegeneration has reported benefit to sleep efficiency, but only when used in combination. However, no overall benefit was found for cognition, agitation, depression, or functional outcomes.
Slow-Wave Sleep Augmentation
Slow-wave sleep (SWS) represents the central electrophysiological element of the sleep-dependent recovery process, as well as being implicated in sleep-dependent memory consolidation [32], age-related changes in cognition [201], and glymphatic clearance of neurotoxic waste [23, 202]. It is consistently impaired across the spectrum of neurodegeneration [35]. As a result, the development of neurophysiological stimulation techniques that augment SWS, most notably transcranial direct-current stimulation (TDCS) and acoustic stimulation applied during sleep, is a further important emerging frontier in the field of sleep therapies in neurodegeneration.
The ability of such techniques to augment the slow oscillations (SOs) underpinning SWS has been demonstrated consistently and robustly in numerous blinded cross-over sham/stim paradigm studies [203]. While it may seem improbable that pulses of sound alone would have such an effect, it is possible and thought to be mediated by an interaction between the nonlemniscal acoustic pathway and diffuse thalamocortical projections during sleep, wherein acoustic stimuli evoke a widespread synchronous response, akin to a transient SO, in order to mediate arousal to threat. Where the stimulus is at threshold, it is able to induce SO activity without arousal [204].
Transcranial Direct-Current Stimulation
Augmentation of slow oscillation activity by TDCS has demonstrated benefit to declarative memory in both young [205,206,207] and older [208, 209] healthy participants, and in both nocturnal [206] and nap [205, 207, 208] protocols. In Cellini et al. [207], this was accompanied by an overall increase in time spent in slow-wave sleep, and cognitive benefits persisted at 48 h.
There have, however, been a number of negative studies using this approach [210,211,212]. This discrepancy may relate to the variability of the stimulation protocols applied, as well as the timing and frequency of TDCS—all of which appears to be critical to efficacy. For example, Marshall et al. [213] found that theta-TDCS reduces slow oscillation activity and impairs declarative memory while the stimulation protocol used in the negative study by Eggert et al. [212] in fact induced a reduction in slow-wave sleep and increased wake time. By contrast, Cellini et al. [207] found that stimulation during asynchronous slow-wave sleep was more efficacious than that applied during endogenous SO activity, and positive findings may have related to the incorporation of such stimulation in their study. Incongruent findings may also relate to the study population: Koo et al. [214], for example, found that any cognitive benefits of TDCS were only apparent when participants were stratified according to higher baseline memory function.
Of note, two studies also evaluated the effect of sleep–TDCS on mood, demonstrating a positive effect in both healthy participants [205] and those with schizophrenia [215].
To date, only one study of TDCS in sleep has been conducted in a neurodegenerative cohort. This study [216], undertaken during a nap protocol in sixteen participants with mild cognitive impairment, demonstrated benefit to visual but not verbal or visuospatial declarative memory at 30 min post awakening.
Acoustic Stimulation
Slow-wave augmentation by acoustic stimulation has likewise demonstrated cognitive benefit in young [217,218,219], middle-aged [220], and older healthy adults [221], in both nap [217] and nocturnal [218,219,220,221] protocols, with benefits seen in executive function [220] as well as declarative memory [217,218,219, 221]. In most cases, this was mediated through tones of pink noise delivered by headphones, but more recently, bone conduction via a mastoid application has also been implemented successfully [222].
Compellingly, the degree of cognitive enhancement correlated with the degree of slow-wave augmentation elicited in a number of these studies [218, 220, 221]. Response rates appear variable, however, and in some studies, benefit was only seen when nonresponders were excluded (35% participants) [220]. As with TDCS, there are studies failing to demonstrate cognitive benefit within the literature, but these have typically also failed to show an overall increase in slow-wave activity following the intervention [223, 224]. The precise stimulation protocol again appears critical, but in comparison with TDCS, efficacy to boost slow-wave activity and benefit to cognition appears greatest when stimulation is phase-locked to the upstate of endogenous SOs [218, 225, 226]: so-called closed loop stimulation.
There has to date been only one study of acoustic augmentation of SWS in a neurodegenerative cohort [227]. Conducted in 2019, this nocturnal pilot study in nine patients with amnestic mild cognitive impairment demonstrated highly variable increases in slow-wave activity (1-30%), but promisingly, improvement in declarative memory was demonstrated in five of nine participants, and the degree of improvement correlated with that of slow-wave activity augmentation.
The ease of delivery in a domiciliary setting, and its low side effect profile, places acoustic stimulation at a significant practical advantage over TDCS. Notably, a number of companies have now developed headband devices delivering closed loop acoustic stimulation, designed for use during sleep in the home setting (e.g., Dreem2 headband, Phillips SmartSleep Deep Sleep Headband), in some cases combined with delivery of personalized behavioral measures guidance. It is worth noting, however, that the cumulative effects of the long-term application of acoustic stimulation on cognition are not known: all studies evaluating cognitive outcomes have, as yet, incorporated single-night and immediate postsleep testing protocols only.
Concluding Remarks
Sleep dysfunction in neurodegenerative conditions merits prioritization in clinical care: not only because it has the potential to significantly improve quality of life for patients and their families, but also because there is mounting evidence to suggest that it may also mitigate cognitive and affective symptoms and slow disease progression. Given the lack of therapies that currently achieve this in neurodegeneration, this potential should not be discounted.
In all cases, it is important that the approach to treating sleep dysfunction in a patient with a neurodegenerative condition begins with a comprehensive assessment of this aspect of their condition, via targeted questions, objective scales, and investigations, in order to identify preliminary contributory factors (depression, pain, nocturia, medications, and caffeine/nicotine/alcohol use) and specific clinical sleep pathology (OSA, RLS, RBD, PLMD) where present. These should be addressed with conservative measures and specific treatments as outlined.
Only in the event of such measures failing to bring adequate benefit should other interventions be considered. Of available secondary measures, current evidence is most in favor of behavioral measures alongside bright light therapy, although it is clearly imperative that the practicality of such measures for an individual’s circumstance is taken into account. Currently, the landscape of pharmacological options is largely unfavorable, with deleterious effects likely to outweigh benefit for sedating agents including antidepressants, antihistamines, and antipsychotics, and a lack of cogent evidence suggesting significant benefit from modafinil or melatonin. We would advocate that sedating agents are only used where already mandated for concomitant affective or behavioral symptoms, or in the event of failure of all other measures. The overriding message is therefore that, as clinicians, we should resist the engrained temptation to treat sleep dysfunction in neurodegeneration by add-on prescription and instead take time to implement conservative measures and nonpharmacological interventions that are more likely to bring benefit. Nonetheless, the landscape of pharmacological options is evolving, with both sodium oxybate and orexin antagonists showing promise. Finally, the development of domiciliary devices providing slow-wave sleep augmentation provides further hope of efficacious intervention emerging in the near future.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Change history
18 December 2020
A Correction to this paper has been published: https://doi.org/10.1007/s13311-020-00980-w
References
Carpenter BD, Strauss M, Patterson MB. Sleep Disturbances in Community-Dwelling Patients with Alzheimer’s Disease. Clin Gerontol 1996;16:35–49.
Barone P, Antonini A, Colosimo C, et al. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord 2009;24:1641–1649.
Tandberg E, Larsen JP, Karlsen K. A community-based study of sleep disorders in patients with Parkinson’s disease. Mov Disord 1998;13:895–899.
Guarnieri B, Adorni F, Musicco M, et al. Prevalence of sleep disturbances in mild cognitive impairment and dementing disorders: A multicenter Italian clinical cross-sectional study on 431 patients. Dement Geriatr Cogn Disord 2012;33:50–58.
Chahine LM, Amara AW, Videnovic A. A systematic review of the literature on disorders of sleep and wakefulness in Parkinson’s disease from 2005 to 2015. Sleep Med Rev 2017;35:33–50.
Shafazand S, Wallace DM, Arheart KL, et al. Insomnia, sleep quality, and quality of life in mild to moderate parkinson’s disease. Ann Am Thorac Soc 2017;14:412–419.
Stone KL, Ensrud KE, Ancoli-Israel S. Sleep, insomnia and falls in elderly patients. Sleep Med 2008;9(SUPPL. 1):S18-S22.
Pollak CP, Perlick D, Linsner JP, Wenston J, Hsieh F. Sleep problems in the community elderly as predictors of death and nursing home placement. J Community Health 1990;15:123–135.
Pollak CP, Perlick D. Sleep Problems and Institutionalization of the Elderly. Top.Geriatr. 1991;4:204–210.
Hope T, Keene J, Gedling K, Fairburn CG, Jacoby R. Predictors of institutionalization for people with dementia living at home with a carer. Int J Geriatr Psychiatry 1998;13:682–690.
Bianchetti A, Scuratti A, Zanetti O, et al. Predictors of mortality and institutionalization in Alzheimer disease patients 1 year after discharge from an Alzheimer dementia unit. Dement Geriatr Cogn Disord 1995;6:108–112.
Gehrman P, Gooneratne NS, Brewster GS, Richards KC, Karlawish J. Impact of Alzheimer disease patients’ sleep disturbances on their caregivers. Geriatr Nurs (Minneap) 2018;39:60–65.
Spira AP, Friedman L, Beaudreau SA, et al. Sleep and physical functioning in family caregivers of older adults with memory impairment. Int Psychogeriatr 2010;22:306–311.
McCurry SM, Logsdon RG, Teri L, Vitiello M V. Sleep disturbances in caregivers of persons with dementia: Contributing factors and treatment implications. Sleep Med Rev 2007;11:143–153.
Pillai JA, Leverenz JB. Sleep and Neurodegeneration: A Critical Appraisal. Chest. 2017;151:1375–1386.
Alhola P, Polo-Kantola P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis Treat 2007;3:553–567.
Aidman E, Jackson SA, Kleitman S. Effects of sleep deprivation on executive functioning, cognitive abilities, metacognitive confidence, and decision making. Appl Cogn Psychol 2019;33:188–200.
Lo JC, Ong JL, Leong RLF, Gooley JJ, Chee MWL. Cognitive Performance, Sleepiness, and Mood in Partially Sleep Deprived Adolescents: The Need for Sleep Study. Sleep. 2016;39:687–698.
Chua EC-P, Yeo S-C, Lee IT-G, et al. Sustained Attention Performance during Sleep Deprivation Associates with Instability in Behavior and Physiologic Measures at Baseline. Sleep. 2014;37:27–39.
Beattie L, Kyle SD, Espie CA, Biello SM. Social interactions, emotion and sleep: A systematic review and research agenda. Sleep Med Rev 2015;24:83–100.
Rasmussen MK, Mestre H, Nedergaard M. The glymphatic pathway in neurological disorders. Lancet Neurol 2018;17:1016–1024.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–377.
Fultz NE, Bonmassar G, Setsompop K, et al. Coupled electrophysiological, hemodynamic, and cerebrospinal fluid oscillations in human sleep. Science. 2019;366:628–631.
Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med 2012;4:147.
Iliff JJ, Chen MJ, Plog BA, et al. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci 2014;34:16180–16193.
Rothman SM, Herdener N, Frankola KA, Mughal MR, Mattson MP. Chronic mild sleep restriction accentuates contextual memory impairments, and accumulations of cortical Aβ and pTau in a mouse model of Alzheimer’s disease. Brain Res 2013;1529:200–208.
Holth JK, Fritschi SK, Wang C, et al. The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Science. 2019;363:80–884.
Lucey BP, Hicks TJ, McLeland JS, et al. Effect of sleep on overnight cerebrospinal fluid amyloid β kinetics. Ann Neurol 2018;83:197–204.
Shokri-Kojori E, Wang GJ, Wiers CE, et al. β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proc Natl Acad Sci U S A 2018;115:4483–4488.
Benedict C, Blennow K, Zetterberg H, Cedernaes J. Effects of acute sleep loss on diurnal plasma dynamics of CNS health biomarkers in young men. Randomized Controlled Trial 2020;94:e1181-e11189.
Manchanda S, Singh H, Kaur T, Kaur G. Low-grade neuroinflammation due to chronic sleep deprivation results in anxiety and learning and memory impairments. Mol Cell Biochem 2018;449:63–72.
Rasch B, Born J. About sleep’s role in memory. Physiol Rev 2013;93:681–766.
Todorova R, Zugaro M. Isolated cortical computations during delta waves support memory consolidation. Science. 2019;366:377–381.
Norimoto H, Makino K, Gao M, et al. Hippocampal ripples down-regulate synapses. Science. 2018;359:1524–1527.
Malhotra RK. Neurodegenerative Disorders and Sleep. Sleep Med Clin 2018;13:63–70.
Ratti PL, Nègre-Pagès L, Pérez-Lloret S, et al. Subjective sleep dysfunction and insomnia symptoms in Parkinson’s disease: Insights from a cross-sectional evaluation of the French CoPark cohort. Parkinsonism Relat Disord 2015;21:1323–1329.
Videnovic A, Lazar AS, Barker RA, Overeem S. ‘The clocks that time us’ - Circadian rhythms in neurodegenerative disorders. Nat Rev Neurol 2014; 10:683–693.
Videnovic A, Golombek D. Circadian dysregulation in Parkinson’s disease. Neurobio Sleep and Circadian Rhythms 2017; 2:53–58.
Bliwise DL. Sleep in normal aging and dementia. Sleep. 1993; 16:40–81.
Zhang Y, Ren R, Yang L, et al. Sleep in Huntington’s disease: a systematic review and meta-analysis of polysomongraphic findings. Sleep. 2019;42:10.
Thorpy MJ, Adler CH. Parkinson’s Disease and Sleep. Neurol Clin 2005;23:1187–1208.
Lim ASP, Kowgier M, Yu L, Buchman AS, Bennett DA. Sleep Fragmentation and the Risk of Incident Alzheimer’s Disease and Cognitive Decline in Older Persons. Sleep. 2013;36:1027–32.
Lazar AS, Panin F, Goodman AOG, et al. Sleep deficits but no metabolic deficits in premanifest Huntington’s disease. Ann Neurol 2015;78:630–648.
Mahowald MW, Schenck CH. REM sleep behaviour disorder: A marker of synucleinopathy. Lancet Neurol 2013; 12:417–9.
Högl B, Stefani A, Videnovic A. Idiopathic REM sleep behaviour disorder and neurodegeneration - An update. Nat Rev Neurol 2018.; 14:40–56.
Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O. Sleep-disordered breathing in community-dwelling elderly. Sleep. 1991;14:486–495.
Reynolds CF 3rd, Kupfer DJ, Taska LS et al. Sleep apnea in Alzheimer’s dementia: Correlation with mental deterioration. J Clin Psychiatry 1985;46:257-261.
Ooms S, El-Ju Y. Treatment of Sleep Disorders in Dementia. Curr Treat Options Neurol. 2016; 18:40.
Loddo G, Calandra-Buonaura G, Sambati L, et al. The treatment of sleep disorders in Parkinson’s disease: From research to clinical practice. Front Neurol 2017; 8:42.
Hobson DE, Lang AE, Wayne Martin WR, Razmy A, Rivest J, Fleming J. Excessive daytime sleepiness and sudden-onset sleep in Parkinson disease: A survey by the Canadian Movement Disorders Group. J Am Med Assoc 2002;287:455–463.
Arnulf I, Nielsen J, Lohmann E, et al. Rapid eye movement sleep disturbances in Huntington disease. Arch Neurol 2008;65:482–488.
Musiek ES, Holtzman DM. Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science. 2016; 354: 004–008.
Baquero M. Depressive symptoms in neurodegenerative diseases. World J Clin Cases 2015;3:682.
Nutt DJ, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci 2008;10:329–336.
Menza M, Dobkin RD, Marin H, et al. Treatment of insomnia in Parkinson’s disease: A controlled trial of eszopiclone and placebo. Mov Disord 2010;25:1708–1714.
Dobkin RD, Menza M, Bienfait KL, et al. Depression in Parkinson’s disease: Symptom improvement and residual symptoms after acute pharmacologic management. Am J Geriatr Psychiatry 2011;19:222–229.
Kunz D, Bes F. Melatonin as a therapy in REM sleep behavior disorder patients: An open-labeled pilot study on the possible influence of melatonin on REM-sleep regulation. Mov Disord 1999;14:507–511.
Boeve BF, Silber MH, Ferman TJ. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: Results in 14 patients. Sleep Med 2003;4:281–284.
Takeuchi N, Uchimura N, Hashizume Y, et al. Melatonin therapy for REM sleep behavior disorder. In: Psychiatry and Clinical Neurosciences 2001;55:267–269.
Louter M, van Sloun RJG, Pevernagie DAA, et al. Subjectively impaired bed mobility in Parkinson disease affects sleep efficiency. Sleep Med 2013;14:668–674.
Ray Chaudhuri K, Martinez-Martin P, Rolfe KA, et al. Improvements in nocturnal symptoms with ropinirole prolonged release in patients with advanced Parkinson’s disease. Eur J Neurol 2012;19:105–113.
Stocchi F, Barbato L, Nordera G, Berardelli A, Ruggieri S. Sleep disorders in Parkinson’s disease. J Neurol 1998;245:S15–S18.
Wailke S, Herzog J, Witt K, Deuschl G, Volkmann J. Effect of controlled-release levodopa on the microstructure of sleep in Parkinson’s disease. Eur J Neurol 2011;18:590–596.
Brusa L, Musco S, Bernardi G, et al. Rasagiline effect on bladder disturbances in early mild Parkinson’s disease patients. Parkinsonism Relat Disord 2014; 20:931–932.
Aranda B, Cramer P. Effects of apomorphine and L-dopa on the parkinsonian bladder. Neurourol Urodyn 1993;12:203–209.
Calandra-Buonaura G, Guaraldi P, Doria A, et al. Rotigotine Objectively Improves Sleep in Parkinson’s Disease: An Open-Label Pilot Study with Actigraphic Recording. Parkinsons Dis 2016;2016: 3724148.
Kazui H, Adachi H, Kanemoto H, et al. Effects of donepezil on sleep disturbances in patients with dementia with Lewy bodies: An open-label study with actigraphy. Psychiatry Res 2017;251:312–318.
Ishikawa I, Shinno H, Ando N, Mori T, Nakamura Y. The effect of memantine on sleep architecture and psychiatric symptoms in patients with Alzheimer’s disease. Acta Neuropsychiatr 2016;28:157–164.
Agboton C, Mahdavian S, Singh A, Ghazvini P, Hill A, Sweet R. Impact of nighttime donepezil administration on sleep in the older adult population: A retrospective study. Ment Heal Clin 2014;4(5):257–259.
Trenkwalder C, Kies B, Rudzinska M, Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: A double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord 2011;26:90–99.
Pierantozzi M, Placidi F, Liguori C, et al. Rotigotine may improve sleep architecture in Parkinson’s disease: A double-blind, Randomized, Placebo-controlled polysomnographic study. Sleep Med 2016;21:140–144.
Aira M, Hartikainen S, Sulkava R. Drinking alcohol for medicinal purposes by people aged over 75: A community-based interview study. Fam Pract 2008;25:445–449.
Hornyak M, Feige B, Riemann D, Voderholzer U. Periodic leg movements in sleep and periodic limb movement disorder: Prevalence, clinical significance and treatment. Sleep Med Rev 2006;10:169–177.
Slater G, Steier J. Excessive daytime sleepiness in sleep disorders. Journal of Thoracic Disease 2012; 4:608–616.
Chong MS, Ayalon L, Marler M, et al. Continuous Positive Airway Pressure Reduces Subjective Daytime Sleepiness in Patients with Mild to Moderate Alzheimer’s Disease with Sleep Disordered Breathing. J Am Geriatr Soc 2006;54:777–781.
Troussière A-C, Charley CM, Salleron J, et al. Treatment of sleep apnoea syndrome decreases cognitive decline in patients with Alzheimer’s disease. J Neurol Neurosurg Psychiatry 2014;85:1405-1408.
Ancoli-Israel S, Palmer BW, Cooke JR, et al. Cognitive effects of treating obstructive sleep apnea in Alzheimer’s disease: A randomized controlled study. J Am Geriatr Soc 2008;56:2076–2081.
Cooke JR, Ayalon L, Palmer BW, et al. Sustained use of CPAP slows deterioration of cognition, sleep, and mood in patients with Alzheimer’s disease and obstructive sleep apnea: A preliminary study. J Clin Sleep Med 2009;5:305–309.
Qaseem A, Kansagara D, Forciea MA, et al. Management of chronic insomnia disorder in adults: A clinical practice guideline from the American college of physicians. Ann Intern Med 2016;165:125–133.
Curran HV, Birch B. Differentiating the sedative, psychomotor and amnesic effects of benzodiazepines: a study with midazolam and the benzodiazepine antagonist, flumazenil. Psychopharmacology 1991;103:519–523.
Leufkens TRM, Lund JS, Vermeeren A. Highway driving performance and cognitive functioning the morning after bedtime and middle-of-the-night use of gaboxadol, zopiclone and zolpidem. J Sleep Res 2009;18:387–396.
Barker MJ, Greenwood KM, Jackson M, Crowe SF. Cognitive Effects of Long-Term Benzodiazepine Use: A Meta-Analysis. CNS Drugs 2004;18:37–48.
Meléndez J, Galli I, Boric K, et al. Zolpidem and triazolam do not affect the nocturnal sleep-induced memory improvement. Psychopharmacology (Berl). 2005;181:21–26.
Mednick SC, McDevitt EA, Walsh JK, et al. The critical role of sleep spindles in hippocampal-dependent memory: A pharmacology study. J Neurosci 2013;33:4494–4504.
Zhang J, Yetton B, Whitehurst LN, Naji M, Mednick SC. The effect of zolpidem on memory consolidation over a night of sleep. Sleep. 2020.
Otmani S, Demazières A, Staner C, et al. Effects of prolonged-release melatonin, zolpidem, and their combination on psychomotor functions, memory recall, and driving skills in healthy middle aged and elderly volunteers. Hum Psychopharmacol 2008;23:693–705.
Hall-Porter JM, Schweitzer PK, Eisenstein RD, Ahmed HAH, Walsh JK. The effect of two benzodiazepine receptor agonist hypnotics on sleep-dependent memory consolidation. J Clin Sleep Med 2014;10:27–34.
Vermeeren A, Coenen AML. Effects of the use of hypnotics on cognition. Prog Brain Res 2011;190:89–103.
Arbon EL, Knurowska M, Dijk DJ. Randomised clinical trial of the effects of prolonged-release melatonin, temazepam and zolpidem on slow-wave activity during sleep in healthy people. J Psychopharmacol 2015;29:764–776.
Brunner DP, Dijk DJ, Münch M, Borbély AA. Effect of zolpidem on sleep and sleep EEG spectra in healthy young men. Psychopharmacology 1991;104:1–5.
Cummings SR, Nevitt MC, Browner WS, et al. Risk Factors for Hip Fracture in White Women. N Engl J Med 1995;332:767–773.
Closser MH. Benzodiazepines and the elderly a review of potential problems. J Subst Abus Treat 1991;8:35–41.
Paterniti S, Dufouil C, Alpérovitch A. Long-term benzodiazepine use and cognitive decline in the elderly: The epidemiology of vascular aging study. J Clin Psychopharmacol 2002;22:285–293.
Ellul J, Archer N, Foy CML, et al. The effects of commonly prescribed drugs in patients with Alzheimer’s disease on the rate or deterioration. J Neurol Neurosurg Psychiatry 2007;78:233–239.
Van Ruitenbeek P, Vermeeren A, Riedel WJ. Cognitive domains affected by histamine H1-antagonism in humans: A literature review. Brain Res Rev 2010;64:263–282.
Campbell N, Boustani M, Limbil T, et al. The cognitive impact of anticholinergics: a clinical review. Clin Interv Aging 2009; 4:225–233.
Samuel MJ. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2015;63:2227–2246.
Halliday M, Radford H, Zents KAM, et al. Repurposed drugs targeting eIF2α-P-mediated translational repression prevent neurodegeneration in mice. Brain. 2017;140:1768–1783.
Oderda LH, Young JR, Asche C V., Pepper GA. Psychotropic related hip fractures: meta-analysis of first generation and second generation antidepressant and antipsychotic drugs. Ann Pharmacother 2012;46:917–928.
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J. Antidepressant use and risk of adverse outcomes in older people: Population based cohort study. BMJ. 2011;343:d4551.
Camargos EF, Louzada LL, Quintas JL, Naves JOS, Louzada FM, Nóbrega OT. Trazodone improves sleep parameters in Alzheimer disease patients: A randomized, double-blind, and placebo-controlled study. Am J Geriatr Psychiatry 2014;22:1565–1574.
Roth AJ, McCall WV, Liguori A. Cognitive, psychomotor and polysomnographic effects of trazodone in primary insomniacs. J Sleep Res 2011;20:552–558.
Scoralick FM, Louzada LL, Quintas JL, Naves JOS, Camargos EF, Nóbrega OT. Mirtazapine does not improve sleep disorders in Alzheimer’s disease: results from a double-blind, placebo-controlled pilot study. Psychogeriatrics. 2017;17:89–96.
Krystal AD, Durrence HH, Scharf M, et al. Efficacy and safety of doxepin 1 mg and 3 mg in a 12-week sleep laboratory and outpatient trial of elderly subjects with chronic primary insomnia. Sleep. 2010;33:1553–1561.
Rios Romenets S, Creti L, Fichten C, et al. Doxepin and cognitive behavioural therapy for insomnia in patients with Parkinson’s disease - A randomized study. Parkinsonism Relat Disord 2013;19:670–675.
Meguro K, Meguro M, Tanaka Y, Akanuma K, Yamaguchi K, Itoh M. Risperidone is effective for wandering and disturbed sleep/wake patterns in Alzheimer’s disease. J Geriatr Psychiatry Neurol 2004;17:61–67.
Yin Y, Liu Y, Zhuang J, et al. Low-Dose Atypical Antipsychotic Risperidone Improves the 5-Year Outcome in Alzheimer’s Disease Patients with Sleep Disturbances. Pharmacology. 2015;96:155–162.
Mittal V, Kurup L, Williamson D, Muralee S, Tampi RR. Risk of cerebrovascular adverse events and death in elderly patients with dementia when treated with antipsychotic medications: A literature review of evidence. Am J Alzheimers Dis Other Dement 2011;26:10–28.
Ballard C, Hanney ML, Theodoulou M, et al. The dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trial. Lancet Neurol 2009;8:151–157.
Chiu Y, Bero L, Hessol NA, Lexchin J, Harrington C. A literature review of clinical outcomes associated with antipsychotic medication use in North American nursing home residents. Health Policy 2015;119:802–813.
Masopust J, Protopopová D, Vališ M, Pavelek Z, Klímová B. Treatment of behavioral and psychological symptoms of dementias with psychopharmaceuticals: A review. Neuropsychiatr Dis Treat 2018;14:1211–1220.
Walsh JK, Hall-Porter JM, Griffin KS, et al. Enhancing slow wave sleep with sodium oxybate reduces the behavioral and physiological impact of sleep loss. Sleep. 2010;33:1217–1225.
Maitre M, Klein C, Mensah-Nyagan AG. A proposed preventive role for Gamma-hydroxybutyrate (XyremR) in Alzheimer’s disease. Alzheimer’s Research and Therapy 2016;8:37.
Ondo WG, Perkins T, Swick T, et al. Sodium oxybate for excessive daytime sleepiness in Parkinson disease: An open-label polysomnographic study. Arch Neurol 2008;65:1337–1340.
Büchele F, Hackius M, Schreglmann SR, et al. Sodium oxybate for excessive daytime sleepiness and sleep disturbance in Parkinson disease: A randomized clinical trial. JAMA Neurol 2018;75:114–118.
Lou JS, Dimitrova DM, Park BS, et al. Using modafinil to treat fatigue in parkinson disease: A double-blind, placebo-controlled pilot study. Clin Neuropharmacol 2009;32:305–310.
Ondo WG, Fayle R, Atassi F, Jankovic J. Modafinil for daytime somnolence in Parkinson’s disease: Double blind, placebo controlled parallel trial. J Neurol Neurosurg Psychiatry 2005;76:1636–1639.
Högl B, Saletu M, Brandauer E, et al. Modafinil for the treatment of daytime sleepiness in Parkinson’s disease: A double-blind, randomized, crossover, placebo-controlled polygraphic trial. Sleep. 2002;25:905–909.
Frakey LL, Salloway S, Buelow M, Malloy P. A randomized, double-blind, placebo-controlled trial of modafinil for the treatment of apathy in individuals with mild-to-moderate Alzheimer’s disease. J Clin Psychiatry 2012;73:796–801.
Blackwell AD, Paterson NS, Barker RA, Robbins TW, Sahakian BJ. The effects of modafinil on mood and cognition in Huntington’s disease. Psychopharmacology 2008;199:29–36.
Zakharov A, Khivintseva E. Clinical Use of Melatonin in the Treatment of Sleep Disorders. In: Melatonin - The Hormone of Darkness and its Therapeutic Potential and Perspectives. IntechOpen; 2020.
Cardinali DP. Melatonin: Clinical perspectives in neurodegeneration. Front Endocrinol 2019;10:480.
Pappolla MA, Matsubara E, Vidal R, et al. Melatonin Treatment Enhances Aβ Lymphatic Clearance in a Transgenic Mouse Model of Amyloidosis. Curr Alzheimer Res 2018;15(7):637-642.
Fainstein I, Bonetto AJ, Brusco LI, Cardinali DP. Effects of melatonin in elderly patients with sleep disturbance: A pilot study. Curr Ther Res - Clin Exp 1997;58:990–1000.
Cohen-Mansfield J, Garfinkel D, Lipson S. Melatonin for treatment of sundowning in elderly persons with dementia - A preliminary study. Arch Gerontol Geriatr 2000;31:65–76.
Mishima K, Okawa M, Hozumi S, Hishikawa Y. Supplementary administration of artificial bright light and melatonin as potent treatment for disorganized circadian rest-activity and dysfunctional autonomic and neuroendocrine systems in institutionalized demented elderly persons. Chronobiol Int 2000; 17:419–432.
Cardinali DP, Brusco LI, Liberczuk C, Furio AM. The use of melatonin in Alzheimer’s disease. Neuroendocrinol Lett 2002; 23:20–23.
Serfaty M, Kennell-Webb S, Warner J, Blizard R, Raven P. Double blind randodmised placebo controlled trial of low dose melatonin for sleep disorders in dementia. Int J Geriatr Psychiatry 2002;17:1120–1127.
Gehrman PR, Connor DJ, Martin JL, Shochat T, Corey-Bloom J, Ancoli-Israel S. Melatonin fails to improve sleep or agitation in double-blind randomized placebo-controlled trial of institutionalized patients with alzheimer disease. Am J Geriatr Psychiatry 2009;17:166–169.
Singer C, Tractenberg RE, Kaye J, et al. A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep. 2003;26:893–901.
Asayama K, Yamadera H, Ito T, Suzuki H, Kudo Y, Endo S. Double blind study of melatonin effects on the sleep-wake rhythm, cognitive and non-cognitive functions in Alzheimer type dementia. J Nippon Med Sch 2003;70:334–341.
Dowling GA, Burr RL, Van Someren EJW, et al. Melatonin and bright-light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. J Am Geriatr Soc 2008;56:239–46.
Wade AG, Farmer M, Harari G, et al. Add-on prolonged-release melatonin for cognitive function and sleep in mild to moderate Alzheimer’s disease: A 6-month, randomized, placebo-controlled, multicenter trial. Clin Interv Aging 2014;9:947–961.
Jean-Louis G, Gizycki H, Zizi F. Melatonin effects on sleep, mood, and cognition in elderly with mild cognitive impairment. J Pineal Res 1998;25:177–83.
Dowling GA, Mastick J, Colling E, Carter JH, Singer CM, Aminoff MJ. Melatonin for sleep disturbances in Parkinson’s disease. Sleep Med 2005;6:459–466.
Medeiros CAM, Carvalhedo De Bruin PF, Lopes LA, Magalhães MC, De Lourdes Seabra M, Sales De Bruin VM. Effect of exogenous melatonin on sleep and motor dysfunction in Parkinson’s disease: A randomized, double blind, placebo-controlled study. J Neurol. 2007;254:459–464.
Seppi K, Ray Chaudhuri K, Coelho M, Fox SH, Katzenschlager R, Perez Lloret S, et al. Update on treatments for nonmotor symptoms of Parkinson’s disease—an evidence-based medicine review. Mov Disord 2019;34:180–198.
Zhang W, Chen X Yan, Su S Wen, et al. Exogenous melatonin for sleep disorders in neurodegenerative diseases: a meta-analysis of randomized clinical trials. Neurol Sci. 2016;37:57–65.
Mccleery J, Cohen DA, Sharpley AL. Pharmacotherapies for sleep disturbances in dementia. Vol. 2016, Cochrane Database of Systematic Reviews. 2016; 11:CD009178
Xu J, Wang LL, Dammer EB, et al. Melatonin for Sleep Disorders and Cognition in Dementia: A Meta-Analysis of Randomized Controlled Trials. Am J Alzheimers Dis Other Dement 2015;30: 439–447.
Wang YY, Zheng W, Ng CH, Ungvari GS, Wei W, Xiang YT. Meta-analysis of randomized, double-blind, placebo-controlled trials of melatonin in Alzheimer’s disease. International Journal of Geriatric Psychiatry 2017; 32:50–57.
Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res 2010;19:591–596.
Cedernaes J, Osorio RS, Varga AW, Kam K, Schiöth HB, Benedict C. Candidate mechanisms underlying the association between sleep-wake disruptions and Alzheimer’s disease. Sleep Med Rev 2017;31:102–111.
Kang JE, Lim MM, Bateman RJ, Lee JJ, Smyth LP, Cirrito JR, et al. Amyloid-β dynamics are regulated by orexin and the sleep-wake cycle. Science. 2009;326(5955):1005–1007.
Herring WJ, Connor KM, Snyder E, et al. Suvorexant in patients with insomnia: Pooled analyses of three-month data from phase-3 randomized controlled clinical trials. J Clin Sleep Med 2016;12:1215–1225.
Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: A phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–471.
Rosenberg R, Murphy P, Zammit G, et al. Comparison of Lemborexant With Placebo and Zolpidem Tartrate Extended Release for the Treatment of Older Adults With Insomnia Disorder: A Phase 3 Randomized Clinical Trial. JAMA Netw Open 2019;2:e1918254.
Neylan TC, Richards A, Metzler TJ, et al. Acute cognitive effects of the hypocretin receptor antagonist almorexant relative to zolpidem and placebo: a randomized clinical trial. Sleep. 2020.
Black J, Pillar G, Hedner J, et al. Efficacy and safety of almorexant in adult chronic insomnia: a randomized placebo-controlled trial with an active reference. Sleep Med 2017;36:86–94.
Herring WJ, Connor KM, Snyder E, et al. Suvorexant in Elderly Patients with Insomnia: Pooled Analyses of Data from Phase III Randomized Controlled Clinical Trials. Am J Geriatr Psychiatry 2017;25:791–802.
Herring WJ, Ceesay P, Snyder E, et al. Polysomnographic assessment of suvorexant in patients with probable Alzheimer’s disease dementia and insomnia: a randomized trial. Alzheimers Dement 2020;16:541–551.
Fronczek R, Overeem S, Lee SYY, et al. Hypocretin (orexin) loss in Parkinson’s disease. Brain. 2007;130:1577–1585.
Fronczek R, van Geest S, Frölich M, et al. Hypocretin (orexin) loss in Alzheimer’s disease. Neurobiol Aging 2012;33:1642–1650.
Czeisler CA, Allan JS, Strogatz SH, et al. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science. 1986;233:667–671.
Rubiño JA, Gamundí A, Akaarir M, Canellas F, Rial R, Nicolau MC. Bright Light Therapy and Circadian Cycles in Institutionalized Elders. Front Neurosci 2020;14:359.
Khalsa SBS, Jewett ME, Cajochen C, Czeisler CA. A phase response curve to single bright light pulses in human subjects. J Physiol 2003;549:945–952.
Kobayashi R, Kohsaka M, Fukuda N, Sakakibara S, Honma H, Koyama T. Effects of morning bright light on sleep in healthy elderly women. Psychiatry Clin Neurosci 1999;53:237–238.
Sloane PD, Figueiro M, Cohen L. Light as Therapy for Sleep Disorders and Depression in Older Adults. Clin Geriatr 2008 Mar 1;16:25–31.
Gfigueiro MG, Plitnick BA, Lok A, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging 2014;9:1527–1537.
Van Someren EJW, Kessler A, Mirmiran M, Swaab DF. Indirect bright light improves circadian rest-activity rhythm disturbances in demented patients. Biol Psychiatry 1997;41:955–963.
Fetveit A, Skjerve A, Bjorvatn B. Bright light treatment improves sleep in institutionalised elderly - An open trial. Int J Geriatr Psychiatry 2003;18:520–526.
Mishima K, Hishikawa Y, Okawa M. Randomized, dim light controlled, crossover test of morning bright light therapy for rest-activity rhythm disorders in patients with vascular dementia and dementia of alzheimer’s type. Chronobiol Int 1998;15:647–654.
Dowling GA, Mastick J, Hubbard EM, Luxenberg JS, Burr RL. Effect of timed bright light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. Int J Geriatr Psychiatry 2005;20:738–743.
Ancoli-Israel S, Martin JL, Kripke DF, Marler M, Klauber MR. Effect of light treatment on sleep and circadian rhythms in demented nursing home patients. J Am Geriatr Soc 2002;50:282–289.
Ancoli-Israel S, Gehrman P, Martin JL, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behav Sleep Med 2003;1:22–36.
Burns A, Allen H, Tomenson B, Duignan D, Byrne J. Bright light therapy for agitation in dementia: A randomized controlled trial. Int Psychogeriatr 2009;21:711–721.
Fontana Gasio P, Kräuchi K, Cajochen C, et al. Dawn-dusk simulation light therapy of disturbed circadian rest-activity cycles in demented elderly. Exp Gerontol 2003;38:207–216.
Graf A, Wallner C, Schubert V, et al. The effects of light therapy on mini-mental state examination scores in demented patients. Biol Psychiatry 2001;50:725–727.
Yamadera H, Ito T, Suzuki H, Asayama K, Ito R, Endo S. Effects of bright light on cognitive and sleep–wake (circadian) rhythm disturbances in Alzheimer-type dementia. Psychiatry Clin Neurosci 2000;54:352–353.
Riemersma-van Der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJG, Van Someren EJW. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: A randomized controlled trial. JAMA - J Am Med Assoc. 2008;299:2642–2655.
Barrick AL, Sloane PD, Williams CS, et al. Impact of ambient bright light on agitation in dementia. Int J Geriatr Psychiatry 2010;25:1013–1021.
Willis GL, John E, Turner D. Primary and secondary features of Parkinson's disease improve with strategic exposure to bright light: a case series study. Chronobiol Int 2007;24:521–537.
Willis GL, Moore C, Armstrong SM. A historical justification for and retrospective analysis of the systematic application of light therapy in Parkinson’s disease. Rev Neurosci 2012;23:199–226.
Paus S, Schmitz-Hübsch T, Wüllner U, Vogel A, Klockgether T, Abele M. Bright light therapy in Parkinson’s disease: A pilot study. Mov Disord 2007;22:1495–1498.
Videnovic A, Klerman EB, Wang W, Marconi A, Kuhta T, Zee PC. Timed light therapy for sleep and daytime sleepiness associated with Parkinson disease a randomized clinical trial. JAMA Neurol 2017;74:411–418.
O’Caoimh R, Mannion H, Sezgin D, O’Donovan MR, Liew A, Molloy DW. Non-pharmacological treatments for sleep disturbance in mild cognitive impairment and dementia: A systematic review and meta-analysis. Maturitas. 2019;127:82–94.
Mitolo M, Tonon C, La Morgia C, Testa C, Carelli V, Lodi R. Effects of light treatment on sleep, cognition, mood, and behavior in Alzheimer’s disease: A systematic review. Dement Geriatr Cogn Disord 2018;46:371–384.
Forbes D, Blake CM, Thiessen EJ, Peacock S, Hawranik P. Light therapy for improving cognition, activities of daily living, sleep, challenging behaviour, and psychiatric disturbances in dementia. Cochrane Database Syst Rev 2014;2:CD003946.
van Maanen A, Meijer AM, van der Heijden KB, Oort FJ. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med Rev 2016;29:52–62.
Smilowska K, Van Wamelen DJ, Schoutens AMC, Meinders MJ, Bloem BR. Blue Light Therapy Glasses in Parkinson’s Disease: Patients’ Experience. Parkinsons Dis 2019;2019:1906271.
van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin CM, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: A meta-analysis. Sleep Med Rev 2018;38:3–16.
Alessi CA, Martin JL, Webber AP, Kim EC, Harker JO, Josephson KR. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. J Am Geriatr Soc 2005;53:803–810.
Ouslander JG, Connell BR, Bliwise DL, Endeshaw Y, Griffiths P, Schnelle JF. A Nonpharmacological Intervention to Improve Sleep in Nursing Home Patients: Results of a Controlled Clinical Trial. J Am Geriatr Soc 2006;54:38–47.
Richards KC, Beck C, O’Sullivan PS, Shue VM. Effect of individualized social activity on sleep in nursing home residents with dementia. J Am Geriatr Soc 2005;53:1510–1517.
Connell BR, Sanford JA, Lewis D. Therapeutic effects of an outdoor activity program on nursing home residents with Dementia. J Hous Elder 2007; 21:194-209.
Naylor E, Penev PD, Orbeta L, et al. Daily social and physical activity increases slow-wave sleep and daytime neuropsychological performance in the elderly. Sleep. 2000;23:87–95.
Richards KC, Lambert C, Beck CK, et al. Strength training, walking, and social activity improve sleep in nursing home and assisted living residents: Randomized controlled trial. J Am Geriatr Soc 2011;59:214–223.
Alessi CA, Yoon E, Schnelle JF, Al-Samanai NR, Cruise PA. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: Do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–791.
McCurry SM, Lafazia DM, Pike KC, Logsdon RG, Teri L. Development and evaluation of a sleep education program for older adults with dementia living in adult family homes. Am J Geriatr Psychiatry 2012;20:494–504.
McCurry SM, Gibbons LE, Logsdon RG, Vitiello M V., Teri L. Nighttime Insomnia Treatment and Education for Alzheimer’s Disease: A randomized, controlled trial. J Am Geriatr Soc 2005;53:793–802.
McCurry SM, Pike KC, Vitiello M V., Logsdon RG, Larson EB, Teri L. Increasing walking and bright light exposure to improve sleep in community-dwelling persons with Alzheimer’s disease: Results of a randomized, controlled trial. J Am Geriatr Soc 2011;59:1393–1402.
Cassidy-Eagle E, Siebern A, Unti L, Glassman J, O’Hara R. Neuropsychological Functioning in Older Adults with Mild Cognitive Impairment and Insomnia Randomized to CBT-I or Control Group. Clin Gerontol 2018;41:136–144.
Frazzitta G, Maestri R, Ferrazzoli D, et al. Multidisciplinary intensive rehabilitation treatment improves sleep quality in Parkinson’s disease. J Clin Mov Disord. 2015;2(1):11.
Nascimento CMC, Ayan C, Cancela JM, Gobbi LTB, Gobbi S, Stella F. Effect of a multimodal exercise program on sleep disturbances and instrumental activities of daily living performance on Parkinson’s and Alzheimer’s disease patients. Geriatr Gerontol Int 2014;14:259–266.
Xiao C-M, Zhuang Y-C. Effect of health Baduanjin Qigong for mild to moderate Parkinson’s disease. Geriatr Gerontol Int 2016;16:911–919.
Osawa C, Kamei Y, Nozaki K, Furusawa Y, Murata M. Brief Cognitive Behavioral Therapy for Insomnia in Parkinson’s Disease: A Case Series Study. Jpn Psychol Res 2020;4.
Coe S, Franssen M, Collett J, et al. Physical Activity, Fatigue, and Sleep in People with Parkinson’s Disease: A Secondary per Protocol Analysis from an Intervention Trial. Parkinsons Dis 2018;2018:1517807.
Amara AW, Wood KH, Joop A, et al. Randomized, Controlled Trial of Exercise on Objective and Subjective Sleep in Parkinson’s Disease. Mov Disord 2020;35:947–958.
Gibson RH, Gander PH, Dowell AC, Jones LM. Non-pharmacological interventions for managing dementia-related sleep problems within community dwelling pairs: A mixed-method approach. Dementia. 2017;16:967–984.
McCurry SM, Gibbons LE, Logsdon RG, Vitiello M, Teri L. Training caregivers to change the sleep hygiene practices of patients with dementia: The NITE-AD project. J Am Geriatr Soc 2003;51:1455–1460.
Pace-Schott EF, Spencer RMC. Age-related changes in the cognitive function of sleep. In: Progress in Brain Research 2011;191:75–89.
Cordone S, Annarumma L, Rossini PM, De Gennaro L. Sleep and β-amyloid deposition in Alzheimer disease: Insights on mechanisms and possible innovative treatments. Frontiers in Pharmacology. Frontiers Media S.A. 2019; 10:695.
Grimaldi D, Papalambros NA, Zee PC, Malkani RG. Neurostimulation techniques to enhance sleep and improve cognition in aging. Neurobiology of Disease Academic Press Inc 2020;141:104865.
Bellesi M, Riedner BA, Garcia-Molina GN, Cirelli C, Tononi G. Enhancement of sleep slow waves: Underlying mechanisms and practical consequences. Front Syst Neurosci 2014;8:208.
Marshall L, Mölle M, Hallschmid M, Born J. Transcranial direct current stimulation during sleep improves declarative memory. J Neurosci 2004;24:9985–9992.
Marshall L, Helgadóttir H, Mölle M, Born J. Boosting slow oscillations during sleep potentiates memory. Nature. 2006;444:610–613.
Cellini N, Shimizu RE, Connolly PM, et al. Short Duration Repetitive Transcranial Electrical Stimulation During Sleep Enhances Declarative Memory of Facts. Front Hum Neurosci 2019;13:123.
Westerberg CE, Florczak SM, Weintraub S, et al. Memory improvement via slow-oscillatory stimulation during sleep in older adults. Neurobiol Aging 2015;36:2577–2586.
Ladenbauer J, Külzow N, Passmann S, et al. Brain stimulation during an afternoon nap boosts slow oscillatory activity and memory consolidation in older adults. Neuroimage. 2016;142:311–323.
Sahlem GL, Badran BW, Halford JJ, et al. Oscillating square wave transcranial direct current stimulation (tDCS) delivered during slow wave sleep does not improve declarative memory more than sham: A randomized sham controlled crossover study. Brain Stimul 2015;8:528–534.
Bueno-Lopez A, Eggert T, Dorn H, Danker-Hopfe H. Slow oscillatory transcranial direct current stimulation (so-tDCS) during slow wave sleep has no effects on declarative memory in healthy young subjects. Brain Stimul 2019;12:948–958.
Eggert T, Dorn H, Sauter C, Nitsche MA, Bajbouj M, Danker-Hopfe H. No effects of slow oscillatory transcranial direct current stimulation (tDCS) on sleep-dependent memory consolidation in healthy elderly subjects. Brain Stimul 2013;6:938–945.
Marshall L, Kirov R, Brade J, Mölle M, Born J. Transcranial electrical currents to probe EEG brain rhythms and memory consolidation during sleep in humans. PLoS One. 2011;6(2):e16905.
Koo PC, Mölle M, Marshall L. Efficacy of slow oscillatory-transcranial direct current stimulation on EEG and memory – contribution of an inter-individual factor. Eur J Neurosci 2018;47:812–823.
Göder R, Baier PC, Beith B, et al. Effects of transcranial direct current stimulation during sleep on memory performance in patients with schizophrenia. Schizophrenia Research Schizophr Res; 2013;144:153–154.
Ladenbauer J, Ladenbauer J, Külzowä N, et al. Promoting sleep oscillations and their functional coupling by transcranial stimulation enhances memory consolidation in mild cognitive impairment. J Neurosci 2017;37:7111–7124.
Ong JL, Lo JC, Chee NIYN, et al. Effects of phase-locked acoustic stimulation during a nap on EEG spectra and declarative memory consolidation. Sleep Med 2016;20:88–97.
Ngo HV V., Martinetz T, Born J, Mölle M. Auditory closed-loop stimulation of the sleep slow oscillation enhances memory. Neuron. 2013;78:545–553.
Leminen MM, Virkkala J, Saure E, et al. Enhanced Memory Consolidation Via Automatic Sound Stimulation During Non-REM Sleep. Sleep. 2017;40:zsx003.
Diep C, Ftouni S, Manousakis JE, Nicholas CL, Drummond SPA, Anderson C. Acoustic slow wave sleep enhancement via a novel, automated device improves executive function in middle-aged men. SLEEPJ. 2020;43:zsz197.
Papalambros NA, Santostasi G, Malkani RG, et al. Acoustic enhancement of sleep slow oscillations and concomitant memory improvement in older adults. Front Hum Neurosci 2017;11:109.
Debellemaniere E, Chambon S, Pinaud C, et al. Performance of an ambulatory dry-EEG device for auditory closed-loop stimulation of sleep slow oscillations in the home environment. Front Hum Neurosci 2018;12:88.
Henin S, Borges H, Shankar A, et al. Closed-loop acoustic stimulation enhances sleep oscillations but not memory performance. eNeuro. 2019;6:ENE URO.0306-19.
Ngo HV V., Seibold M, Boche DC, Mölle M, Born J. Insights on auditory closed-loop stimulation targeting sleep spindles in slow oscillation up-states. J Neurosci Methods 2019;316:117–124.
Cox R, Korjoukov I, De Boer M, Talamini LM. Sound asleep: Processing and retention of slow oscillation phase-targeted stimuli. PLoS One 2014; 9:e101567.
Weigenand A, Mölle M, Werner F, Martinetz T, Marshall L. Timing matters: open-loop stimulation does not improve overnight consolidation of word pairs in humans. Eur J Neurosci 2016;44:2357–2368.
Papalambros NA, Weintraub S, Chen T, et al. Acoustic enhancement of sleep slow oscillations in mild cognitive impairment. Ann Clin Transl Neurol 2019;6:1191–1201.
Acknowledgements
ZJV is supported by funding from the Asssociation of British Neurologists (G104701) and Alzheimer’s Research UK (RROU.GAAB). RAB is supported by the Medical Research Council and National Institute for Health Research. ASL is supported by a seed award in science from the Wellcome trust (207799/Z/17/Z).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised to correct errors submitted in the final proof the article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Voysey, Z.J., Barker, R.A. & Lazar, A.S. The Treatment of Sleep Dysfunction in Neurodegenerative Disorders. Neurotherapeutics 18, 202–216 (2021). https://doi.org/10.1007/s13311-020-00959-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-020-00959-7