Abstract
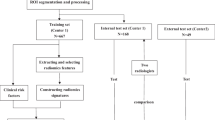
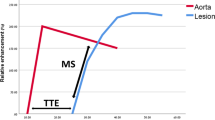
The performance of a support vector machine (SVM) algorithm was investigated to predict prostate tumour location using multi-parametric MRI (mpMRI) data. The purpose was to obtain information of prostate tumour location for the implementation of bio-focused radiotherapy. In vivo mpMRI data were collected from 16 patients prior to radical prostatectomy. Sequences included T2-weighted imaging, diffusion-weighted imaging and dynamic contrast enhanced imaging. In vivo mpMRI was registered with ‘ground truth’ histology, using ex vivo MRI as an intermediate registration step to improve accuracy. Prostate contours were delineated by a radiation oncologist and tumours were annotated on histology by a pathologist. Five patients with minimal imaging artefacts were selected for this study. A Gaussian kernel SVM was trained and tested on different patient data subsets. Parameters were optimised using leave-oneout cross validation. Signal intensities of mpMRI were used as features and histology annotations as true labels. Prediction accuracy, as well as area under the curve (AUC) of the receiver operating characteristics (ROC) curve, were used to assess performance. Results demonstrated the prediction accuracy ranged from 70.4 to 87.1% and AUC of ROC ranged from 0.81 to 0.94. Additional investigations showed the apparent diffusion coefficient map from diffusion weighted imaging was the most important imaging modality for predicting tumour location. Future work will incorporate additional patient data into the framework to increase the sensitivity and specificity of the model, and will be extended to incorporate predictions of biological characteristics of the tumour which will be used in bio-focused radiotherapy optimisation.







Similar content being viewed by others
References
AIHW (2013) Prostate cancer in Australia. AIHW, Canberra
Haas GP, Delongchamps N, Brawley OW, Wang CY, de la Roza G (2008) The worldwide epidemiology of prostate cancer: perspectives from autopsy studies. Can J Urol 15:3866–3871
Koukourakis G, Kelekis N, Armonis V, Kouloulias V (2009) Brachytherapy for prostate cancer: a systematic review. Adv Urol. doi:10.1155/2009/327945
Langley S et al (2012) Report of a consensus meeting on focal low dose rate brachytherapy for prostate cancer. BJU Int 109:7–16
Haworth A et al (2013) Validation of a radiobiological model for low-dose-rate prostate boost focal therapy treatment planning. Brachytherapy 12:628–636
Niaf E, Rouvière O, Mège-Lechevallier F, Bratan F, Lartizien C (2012) Computer-aided diagnosis of prostate cancer in the peripheral zone using multiparametric MRI. Phys Med Biol 57:3833–3851
Giannini V et al (2013) A prostate CAD system based on multiparametric analysis of DCE T1-w, and DW automatically registered images. Proc. SPIE 8670, Medical Imaging 2013: Computer-Aided Diagnosis, 86703
Vos PC, Barentsz JO, Karssemeijer N, Huisman HJ (2012) Automatic computer-aided detection of prostate cancer based on multiparametric magnetic resonance image analysis. Phys Med Biol 57:1527–1542
Barentsz JO et al (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22:746–757
Hoskin PJ et al (2007) Hypoxia in prostate cancer: correlation of BOLD-MRI with pimonidazole immunohistochemistry-initial observations. Int J Radiat Oncol Biol Phys 68:1065–1071
Matulewicz L et al (2013) Anatomic segmentation improves prostate cancer detection with artificial neural networks analysis of H magnetic resonance spectroscopic imaging. J Magn Reson Imaging 1421:1414–1421
Tiwari P, Kurhanewicz J, Rosen M, Madabhushi A (2010) Semi supervised multi-kernel (SeSMiK) graph embedding: identifying aggressive prostate cancer via magnetic resonance imaging and spectroscopy. Int Conf Med Image Comput Comput Interv 13:666–67
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, Margolis D, Schnall MD, Shtern F, Tempany CM, Thoeny HC (2015) PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Assoc Urol 69(1):16–40
Penzkofer T, Tempany-Afdhal CM (2014) Prostate cancer detection and diagnosis: the role of MR and its comparison with other diagnostic modalities—a radiologist’s perspective. NMR Biomed 27:3–15
Lemaître G et al (2015) Computer-Aided Detection and diagnosis for prostate cancer based on mono and multi-parametric MRI: a review. Comput Biol Med 60:8–31
Tofts PS, Brix G, Buckley DL, Evelhoch JL, Henderson E, Knopp MV, H. B. W. Larsson, Lee T-Y, Mayr NA, G. J. M. Parker, Port RE, Taylor J, Weiskoff R (1999) Estimating kinetic parameters from dynamic contrast-enhanced T1-weighted MRI of a diffusible tracer: Standardized quantities and symbols. J Magn Reson Imaging 10:223–232
Wang S, Burtt K, Turkbey B, Choyke P, Summers RM (2014) Computer aided-diagnosis of prostate cancer on multiparametric MRI: a technical review of current research. BioMed Res Int
Steenbergen P et al (2015) Prostate tumor delineation using multiparametric magnetic resonance imaging: Inter-observer variability and pathology validation. Radiother Oncol 115:186–190
Artan Y et al (2009) Prostate cancer segmentation with multispectral MRI using cost-sensitive conditional random fields. In: 2009 IEEE international symposium on biomedical imaging: from Nano to Macro, Boston, MA, pp 278–281
Liu P et al (2013) A prostate cancer computer-aided diagnosis system using multimodal magnetic resonance imaging and targeted biopsy labels. In: Proceedings of SPIE—the international society for optical engineering, vol 8670
Kelm BM, Menze BH, Zechmann CM, Baudendistel KT, Hamprecht FA (2007) Automated estimation of tumor probability in prostate magnetic resonance spectroscopic imaging: pattern recognition vs quantification. Magn Reson Med 57(1):150–159
Litjens G, Debats O, Barentsz J, Karssemeijer N, Huisman H (2014) Computer-aided detection of prostate cancer in MRI. IEEE Trans Med Imaging 33:1083–1092
Langer DL et al (2009) Prostate cancer detection with multi-parametric MRI: logistic regression analysis of quantitative T2, diffusion-weighted imaging, and dynamic contrast-enhanced MRI. J Magn Reson Imaging 30:327–334
Litjens GJS, Barentsz JO, Karssemeijer N & Huisman HJ (2012) Automated computer-aided detection of prostate cancer in MR images: from a whole-organ to a zone-based approach. In: Progress in biomedical optics and imaging—proceedings of SPIE, vol 8315
Parfait S, Walker PM, Créhange G, Tizon X, Mitéran J (2012) Classification of prostate magnetic resonance spectra using Support Vector Machine. Biomed Signal Process Control 7:499–508
Ampeliotis D, Antonakoudi A, Berberidis K, Psarakis EZ (2007) Computer aided detection of prostate cancer using fused information from dynamic contrast enhanced and morphological magnetic resonance images. In: IEEE international conference on signal processing and communications, 2007. ICSPC 2007, Dubai, pp 888–891
Karatzoglou A, Meyer D, Hornik K (2006) Support vector machines. R J Stat Softw 15:28
Pedregosa F et al (2011) Scikit-learn: Machine learning in Python. J Mach Learn Res 12:2825–2830
Chang C, Lin, C. LIBSVM (2011) A Library for Support Vector Machines. ACM Trans Intell Syst Technol 2:1–39
Reynolds HM et al (2015) Development of a registration framework to validate MRI with histology for prostate focal therapy. Med Phys 42:7078–7089
Tofts PS T1-weighted DCE imaging concepts: modelling, acquisition and analysis. Signal 500(450):400
Shen Y, Snyder C, Goerner F, Moritz R, Runge V (2013) Accurate T1 relaxivities (r1) of gadolinium-based magnetic resonance contrast agents (GBCAs) in human whole blood at 1.5 T and 3 T. Radiological Society of North America 2013 Scientific Assembly and Annual Meeting
Sourbron SP, Buckley DL (2011) On the scope and interpretation of the Tofts models for DCE-MRI. Magn Reson Med 66:735–745
Whitcher B, Schmid V, Thornton A (2011) oro. nifti: Rigorous-NIfTI input/output. R package version 0. 2:6
R Core Team (2014) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Boser BE, Guyon IM, Vapnik VN (1992) A training algorithm for optimal margin classifiers. In: Proceedings of the 5th annual ACM workshop on computing learning theory, pp 144–152
Pérez F, Granger BE, Hunter JD (2011) Python: An ecosystem for scientific computing. Comput Sci Eng 13:13–21
Hofmann T, Schölkopf B, Smola AJ (2006) A review of kernel methods in machine learning. Mac-Planck-Institut für biologische, Kybernetik, Tech. Rep, p 156
Hummels DM (1992) On the training of radial basis function classifiers. Neural Netw 5:595–603
Hsu CW, Chang CC, Lin CJ (2003) A practical guide to support vector classification
Kumar R, Indrayan A (2011) Receiver operating characteristic (ROC) curve for medical researchers. Indian Pediatr 48:277–287
Liaw A, Wiener M (2002) Classification and regression by random Forest. R news 2:18–22
Tiwari P, Viswanath S, Kurhanewicz J, Sridhar A, Madabhushi A (2012) Multimodal wavelet embedding representation for data combination (MaWERiC): integrating magnetic resonance imaging and spectroscopy for prostate cancer detection. NMR Biomed 25:607–619
Sung YS et al (2011) Prostate cancer detection on dynamic contrast-enhanced mri: computer-aided diagnosis versus single perfusion parameter maps. Am J Roentgenol 197:1122–1129
Liu X et al (2009) Prostate cancer segmentation with simultaneous estimation of markov random field parameters and class. IEEE Trans Med Imaging 28:906–915
DiFranco MD et al (2011) Ensemble based system for whole-slide prostate cancer probability mapping using color texture features. Comput Med Imaging Graph 35(7–8):629–645
Wu X et al (2008) Top 10 algorithms in data mining. Knowl Inf Syst 14(1):1–37
Gillies RJ, Kinahan PE, Hricak H (2016) “Radiomics: images are more than pictures, they are data”. Radiology 278(2):563–577
Chenevert TL et al (2011) Diffusion coefficient measurement using a temperature-controlled fluid for quality control in multicenter studies. J Magn Reson Imaging 34(4):983–987
Krynicki K, Green CD, Sawyer DW (1978) Pressure and temperature dependence of self-diffusion in water. Faraday Discuss Chem Soc 66(0):199–208
Jaffray DA et al (2015) Quantitative imaging in radiation oncology: an emerging science and clinical services. Semin Radiat Oncol 25(4):292–304
Haralick RM, Shanmugam K, Dinstein I (1973) Textural features for image classification. IEEE Trans Syst Man Cybern 6:610–621
Abdi H, Williams LJ (2010) Principal component analysis. Wiley interdisciplinary reviews. Computational Statistics 2:433–459
Rossi F et al (2015) A 3D voxel neighborhood classification approach within a multiparametric MRI Classifier for prostate cancer detection, pp 231–239
LeSage JP (2008) An introduction to spatial econometrics. Rev d’économie Ind 123:19–44
Dormann CF (2007) Assessing the validity of autologistic regression. Ecol Modell 207:234–242
Choi YJ et al (2007) Functional MR imaging of prostate cancer. Radiographics 27:63–75
Litjens GJS, Vos PC, Barentsz JO, Karssemeijer N, Huisman HJ (2011) Automatic computer aided detection of abnormalities in multi-parametric prostate MRI. Proc SPIE 7963:79630T–79630T–7
Acknowledgements
This research is supported by the Prostate Cancer Foundation of Australia, The University of Melbourne and Cancer Therapeutics CRC. The authors would also like to show their gratitude to Courtney Savill and Lauren Caspersz who have made substantial contributions during data collections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
Ethics in this article is approved by Human Research Ethics Committee (HREC).
Rights and permissions
About this article
Cite this article
Sun, Y., Reynolds, H., Wraith, D. et al. Predicting prostate tumour location from multiparametric MRI using Gaussian kernel support vector machines: a preliminary study. Australas Phys Eng Sci Med 40, 39–49 (2017). https://doi.org/10.1007/s13246-016-0515-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-016-0515-1