Abstract
Objective
To improve the awareness and knowledge regarding Maternal Near Miss (MNM) among health service providers in the selected districts and women’s hospitals in Maharashtra, India.
Methods
A one-day training programme on MNM was conducted at four Family Welfare Training Centres in the state of Maharashtra, India, for the health service providers, viz. gynaecologists, pathologists, anaesthesiologists, medical officers, staff nurses, other paramedical workers of the selected 29 districts/women’s hospitals in Maharashtra. A total of 147 participants participated in the training programme. The participants filled a questionnaire before (pretest) and after the training (post-test) with the same set of questions pertaining to knowledge on the basic and operational aspects of MNM.
Results
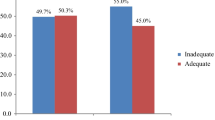
There was a significant improvement in the level of knowledge (post-test responses vs pretest responses) about the correct definition and classification of MNM, as per the instructions in the MNM-R guidelines by the Government of India. The service providers informed regarding the challenges in the implementation of the MNM-R guidelines at their hospitals such as shortage of manpower in terms of specialists and need of quality assurance.
Conclusion
The training programme improved the knowledge of the service providers about MNM, which would help them to implement the MNM-R guidelines effectively at their hospitals. This training effectively upgraded the knowledge level, and therefore, such trainings should be organized for all obstetricians, high-dependency unit (HDU) personnel and critical care teams.
Similar content being viewed by others
References
National Institution for Transforming India, Government of India. https://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births. Accessed 23 Sept 2018
Geller SE, Rosenberg D, Cox SM. The continuum of maternal morbidity and mortality: factors associated with severity. Am J Obstet Gynecol. 2004;191:39–944.
Evaluating the quality of care for severe pregnancy complications. The WHO near-miss approach for maternal health. World Health Organization; 2011. pp. 1–34
Oladapo OT, Sule-odu AO, Olatunj AO, et al. “Near miss” Obstetric events and maternal deaths in Sagamu, Nigeria: a retrospective study. Reprod Health J. 2005;2(9):1–9.
Souza JP, Cecatti JG, Parpineli MA, et al. Appropriate criteria for identification of near miss maternal morbidity in tertiary care facilities: a cross-sectional study. BMC Pregnancy Childbirth. 2007;7(20):1–8.
Operational Guidelines on Maternal Near Miss Review, Ministry of Health and Family Welfare. Government of India; 2014
Kumar R, Floor S, Tewari A. Burdwan district in West Bengal. Indian J Public Heal. 2018;62:235–43.
Kalhan M, Singh S, Punia A, et al. Maternal near-miss audit: Lessons to be learnt. Int J Appl Basic Med Res. 2017;7:85–7.
Chhabra P. Maternal near miss: an indicator for maternal health and maternal care. Indian J Community Med. 2014;39:132–7.
Lazzerini M, Richardson S, Ciardelli V, et al. Effectiveness of the facility-based maternal near-miss case reviews in improving maternal and newborn quality of care in low-income and middle-income countries: a systematic review. BMJ Open. 2018;8:e019787.
Liyew EF, Yalew AW, Afework MF, et al. Incidence and causes of maternal near-miss in selected hospitals of Addis Ababa. Ethiopia. PLoS ONE. 2017;12:e0179013.
De Pinho Maria, Da Silva J, Fonseca SC, Augusto M, Dias B, Izzo AS, Teixeira GP, et al. 7 REVIEW Concepts, prevalence and characteristics of severe maternal morbidity and near miss in Brazil: a systematic review. Rev Bras Saúde Mater Infant. 2018;18(1):7–35. https://doi.org/10.1590/1806-93042018000100002.
Manjunatha G 2018 A study of maternal near miss at a district teaching hospital: a retrospective observational study. Int J Reprod Contracept Obs Gynecol. 7(4):1421–6. 10.18203/2320–1770.ijrcog20181328
Marwah G 2017 Maternal near miss review: a brief appraisal. Int J Reprod Contracept Obs Gynecol 6(5):1703–6. 10.18203/2320–1770.ijrcog20171928
Maswime S, Buchmann E. A systematic review of maternal near miss and mortality due to postpartum haemorrhage. Int J Gynaecol Obstet. 2017;137:1–7.
O’Malley EG, Popivanov P, Fergus A, et al. Maternal near miss: What lies beneath? Eur J Obstet Gynecol Reprod Biol. 2016;199:116–20.
Tura AK, Stekelenburg J, Scherjon SA, et al. Adaptation of the WHO maternal near miss tool for use in sub-Saharan Africa: an international Delphi study. BMC Pregnancy Childbirth. 2017;17:445.
Ps R, Verma S, Rai L, et al. “Near miss” obstetric events and maternal deaths in a tertiary care hospital: an audit. J Pregnancy. 2013. https://doi.org/10.1155/2013/393758.
Firdawek E, Worku A. Maternal near miss and still birth in developing countries: a systematic review with meta-analysis. J Pregnancy Child Health. 2015;2:209. https://doi.org/10.4172/2376-127X.1000209.
David E, Machungo F, Zanconato G, et al. Maternal near miss and maternal deaths in Mozambique: a cross-sectional, region-wide study of 635 consecutive cases assisted in health facilities of Maputo province. BMC Pregnancy Childbirth. 2014;14:401.
Bhutta ZA, Lassi ZS, Mansoor N. Systematic review on human resources for health interventions to improve maternal health outcomes: evidence from developing countries. www.who.int/pmnch/activities/human_resources/hrh_maternal_health_2010.pdf. Accessed 11 Jan 2018
Acknowledgements
We acknowledge the Ministry of Health and Family Welfare, Government of India and Government of Maharashtra, for providing funding support for the study through the Program Implementation Plan of the state. The authors acknowledge the encouragement received from ICMR (NIRRH/RA/713 /12–2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest:
None.
Ethical Approval
Ethical approval (expedited review) was taken from the institutional ethics committee.
Informed Consent
Waiver of informed consent was requested as the responses of the participants were completely anonymized.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Ragini Kulkarni is the Scientist E in the Department of Operational Research, National Institute for Research in Reproductive Health (NIRRH), Indian Council of Medical Research (ICMR), Mumbai, Maharashtra, India. Dr. Sanjay Chauhan is the Scientist G in the Department of Operational Research, National Institute for Research in Reproductive Health (NIRRH), Indian Council of Medical Research (ICMR), Mumbai, Maharashtra, India. Dr. Anushree Patil is the Scientist D in the Department of Clinical Research, National Institute for Research in Reproductive Health (NIRRH), Indian Council of Medical Research (ICMR), Mumbai, Maharashtra, India. Dr. Poonam Shivkumar is the Professor and Head in the Department of Obstetrics and Gynecology, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India. Dr. Surekha Tayade is the Professor in the Department of Obstetrics and Gynecology, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India. Dr. Namrata Dohate is the Consultant in the Department of Operational Research, National Institute for Research in Reproductive Health (NIRRH), Indian Council of Medical Research (ICMR), Mumbai, Maharashtra, India. Dr. Archana Patil is the Additional Director of Health Services in the State Family Welfare Bureau, Pune. Dr. Aniruddha Deshpande is the Assistant Director, Maternal Health & Training in the State Family Welfare Bureau, Pune. Dr. Madhusudan Karnataki is the Consultant Maternal Health in the State Family Welfare Bureau, Pune, India.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kulkarni, R., Chauhan, S., Patil, A. et al. Impact of Training on Awareness and Knowledge of Service Providers About Maternal Near-Miss Events in Maharashtra, India. J Obstet Gynecol India 69, 529–534 (2019). https://doi.org/10.1007/s13224-019-01259-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-019-01259-7