Abstract
Aim-Background
The aim of the present review is to evidence the differences in the nature of PCS between open and laparoscopic cholecystectomy and also to examine how this condition has evolved over the years. In 5 to 40% of patients with cholelithiasis, regardless of the type of surgery, the symptoms persist postoperatively, leading to the development of the so-called postcholecystectomy syndrome (PCS). The time of the onset of symptoms ranges from 2 days to 25 years after cholecystectomy.
Methods
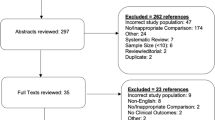
A total number of 926 articles were found as a literature reference pool. We searched English language articles published in Medline, Scopus and google scholar. Only review articles were retrieved because no comparative studies or prospective clinical trials were found to provide statistically significant conclusions. The final group of articles was reviewed, and a total of 57 papers were used for the present review.
Results
The literature is conflicting as concerns the pathophysiology and the aetiology of PCS. Regardless of the type of surgery, it seems that PCS is correlated to age and sex. The prevailing view is that retained or recurrent gallstones, gallbladder remnants and Sphincter of Oddi dysfunction are the primary causes. Moreover, systemic diseases of the gastrointestinal (GI) tract, cardiac disorders, autoimmune diseases, nervous system and psychological distress can mimic PCS symptoms. Nonetheless, there are many available techniques regarding diagnosis and treatment. Nowadays, the majority of researchers endorse ERCP as the gold standard for diagnosis and treatment.
Conclusion
The preoperative meticulous investigation of patients with cholelithiasis is mandatory in order to identify coexisting disorders related to PCS, achieve a better therapeutic approach, and principally reduce PCS incidence.
Περίληψη
Σκοπός
Σκοπός της παρούσας ανασκόπησης είναι να καταγράψει και να αναδείξει τις διαφορές στη φύση του μετά χολοκυστεκτομή σύνδρομο PCS μεταξύ της ανοικτής και λαπαροσκοπικής χολοκυστεκτομής καθώς επίσης να εξετάσει πώς αυτή η κατάσταση έχει εξελιχθεί με την πάροδο των ετών.
Εισαγωγή
Η χολοκυστεκτομή αποτελεί μια από τις συχνότερες επεμβάσεις στις ανεπτυγμένες χώρες. Η κυριότερη αιτία για την οποία πραγματοποιούνται είναι η χολολιθίαση. Τα τελευταία 20 χρόνια η πλειονότητα των επεμβάσεων πραγματοποιείται λαπαροσκοπικά. Σε ποσοστό 5 έως 40% των ασθενών με χολολιθίαση, ανεξάρτητα από τον τύπο του χειρουργείου, τα συμπτώματα επιμένουν μετεγχειρητικά ή αναπτύσσεται το «μετά χολοκυστεκτομή σύνδρομο» (PCS), ενώ ο χρόνος από την έναρξη των συμπτωμάτων κυμαίνεται από 2 ημέρες έως 25 χρόνια.
Υλικό-Μέθοδος
Από την αναζήτηση της διεθνούς βιβλιογραφίας ανακτήθηκαν 926 άρθρα ως βάση αναφοράς. Στη συνέχεια χρησιμοποιήθηκαν άρθρα ανασκόπησης της αγγλικής βιβλιογραφίας. Για την παρούσα μελέτη χρησιμοποιήθηκαν 57 δημοσιεύσεις ανασκόπησης στις οποίες προστέθηκαν κατά περίπτωση αναφορές σε χαρακτηριστικά του PCS.
Αποτελέσματα
Από την ανασκόπηση της βιβλιογραφίας καταγράφονται αντικρουόμενα αποτελέσματα σχετικά με την παθοφυσιολογία και την αιτιολογία του PCS. Ανεξάρτητα από το είδος της χειρουργικής επέμβασης φαίνεται ότι το PCS συσχετίζεται με την ηλικία και το φύλο. Η κυρίαρχη άποψη είναι ότι τυχόν παραμείναντες λίθοι εντός του κυστικού πόρου ή του χοληδόχου πόρου ή υποτροπιάζουσα λιθίαση καθώς και η δυσλειτουργία του σφιγκτήρα του Oddi είναι οι κύριες αιτίες του συνδρόμου. Επίσης, συστηματικά νοσήματα του γαστρεντερικού σωλήνα, καρδιακές παθήσεις, αυτοάνοσα νοσήματα, παθήσεις του νευρικού συστήματος καθώς και ψυχολογικά αίτια μπορεί να μιμούνται τα συμπτώματα PCS. Στις μέρες μας υπάρχουν πολλά διαθέσιμα μέσα όσον αφορά στη διάγνωση και στη θεραπεία. Σήμερα η πλειοψηφία των ερευνητών υποστηρίζει ότι ο χρυσός κανόνας στη διάγνωση και θεραπεία είναι η ERCP. Η προεγχειρητική σχολαστική έρευνα των ασθενών με χολολιθίαση είναι υποχρεωτική προκειμένου να προσδιοριστούν συνυπάρχουσες διαταραχές που σχετίζονται με το μεταχολοκυστεκτομή σύνδρομο έτσι ώστε να επιτευχθεί μια καλύτερη θεραπευτική προσέγγιση αλλά κυρίως ελάττωση της συχνότητας εμφάνισης του μεταχολοκυστεκτομή συνδρόμου.
Similar content being viewed by others
References
Robinson TN, Biffl WL, Moore EE, Heimbach JK, Calkins CM, Burch JM. Predicting failure of outpatient laparoscopic cholecystectomy. American Journal of Surgery 2002;184:515–8; discussion 8-9.
Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 1999;117:632–9.
Halldestam I, Kullman E, Borch K. Incidence of and potential risk factors for gallstone disease in a general population sample. The British Journal of Surgery 2009;96:1315–22.
Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Current Gastroenterology Reports 2005;7:132–40.
Wang HH, Liu M, Clegg DJ, Portincasa P, Wang DQ. New insights into the molecular mechanisms underlying effects of estrogen on cholesterol gallstone formation. Biochimica et Biophysica Acta. 2009;1791:1037–47.
McKernan JB. Origin of laparoscopic cholecystectomy in the USA: personal experience. World Journal of Surgery 1999;23:332–3.
Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic cholecystectomy conversion rates two decades later. JSLS: Journal of the Society of Laparoendoscopic Surgeons/Society of Laparoendoscopic Surgeons. 2010;14:476–83.
Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. The Cochrane Database of Systematic Reviews. 2006:CD006231.
Murshid KR. The postcholecystectomy syndrome: a review. Saudi journal of gastroenterology: Official Journal of the Saudi Gastroenterology Association. 1996;2:124–37.
Womack NA, Crider RL. The Persistence of Symptoms Following Cholecystectomy. Annals of surgery. 1947;126:31–55.
Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). International Journal of Surgery. 2010;8:15–7.
Girometti R, Brondani G, Cereser L, et al. Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. The British Journal of Radiology. 2010;83:351–61.
Perera E, Bhatt S, Dogra VS. Cystic duct remnant syndrome. Journal of Clinical Imaging Science. 2011;1:2.
Shalimov AA. [Principles of treating the postcholecystectomy syndrome]. Klinicheskaia Khirurgiia 1989:6–10.
Comajuncosas J, Vallverdu H, Orbeal R, Pares D. [Trocar site incisional hernia in laparoscopic surgery]. Cirugia Espanola 2011;89:72–6.
Walsh RM, Ponsky JL, Dumot J. Retained gallbladder/cystic duct remnant calculi as a cause of postcholecystectomy pain. Surgical Endoscopy 2002;16:981–4.
Patel MI, Hardman DT, Nicholls D, Fisher CM, Appleberg M. The incidence of deep venous thrombosis after laparoscopic cholecystectomy. The Medical Journal of Australia. 1996;164:652–4, 6.
Koksoy C, Kuzu MA, Kurt I, et al. Haemodynamic effects of pneumoperitoneum during laparoscopic cholecystectomy: a prospective comparative study using bioimpedance cardiography. The British Journal of Surgery 1995;82:972–4.
Rajendra A, Cohen SA, Kasmin FE, Siegel JH, Leitman M. Surgical clip migration and stone formation in a gallbladder remnant after laparoscopic cholecystectomy. Gastrointestinal endoscopy 2009;70:780–1.
Alper I, Ulukaya S, Yuksel G, Uyar M, Balcioglu T. Laparoscopic cholecystectomy pain: effects of the combination of incisional and intraperitoneal levobupivacaine before or after surgery. Agri: Agri. 2014;26:107–12.
Freud M, Djaldetti M, De Vries A, Leffkowitz M. Postcholecystectomy syndrome: a survey of 114 patients after biliary tract surgery. Gastroenterologia 1960;93:288–93.
Schofer JM. Biliary causes of postcholecystectomy syndrome. The Journal of Emergency Medicine 2010;39:406–10.
Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and Liver 2012;6:172–87.
Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. The British Journal of Surgery 2006;93:844–53.
Karmacharya A, Malla BR, Joshi HN, Gurung RB, Rajbhandari M. The predictive value of pre-operative symptoms including upper gastrointestinal endoscopy before laparoscopic cholecystectomy for elective symptomatic cholecystolithiasis. Kathmandu University Medical Journal 2013;11:300–4.
AbuFarsakh NA, Stietieh M, Abu Farsakh FA. The postcholecystectomy syndrome. A role for duodenogastric reflux. Journal of Clinical Gastroenterology 1996;22:197–201.
Sugawa C, Brown KL, Matsubara T, et al. The role of endoscopic biliary sphincterotomy for the treatment of type 1 biliary dysfunction (papillary stenosis) with or without biliary stones. American Journal of Surgery 2014;207:65–9.
Shaffer EA. Acalculous biliary pain: motility dysfunction and functional pain. Canadian journal of gastroenterology = Journal Canadien de Gastroenterologie 2001;15:358–9.
Jagannath S, Kalloo AN. Efficacy of biliary scintigraphy in suspected sphincter of oddi dysfunction. Current Gastroenterology Reports 2001;3:160–5.
Vijayakumar V, Briscoe EG, Pehlivanov ND. Postcholecystectomy sphincter of oddi dyskinesia—a diagnostic dilemma—role of noninvasive nuclear and invasive manometric and endoscopic aspects. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2007;17:10–3.
Osawa H, Saito M, Fujii M, Yamanaka T, Yaginuma T. Postcholecystectomy syndrome mimicking angina pectoris detected by the morphine provocation test. Internal Medicine 1995;34:51–3.
Stefaniak T, Vingerhoets A, Babinska D, et al. Psychological factors influencing results of cholecystectomy. Scandinavian Journal of Gastroenterology 2004;39:127–32.
Bennett E, Evans P, Dowsett J, Kellow J. Sphincter of Oddi dysfunction: psychosocial distress correlates with manometric dyskinesia but not stenosis. World Journal of Gastroenterology: WJG. 2009;15:6080–5.
Dancer JT, Hawley WD, Duval MK, Jr. The Intrinsic Contractile Activity of the Duodenum. Extrinsic Influences. Archives of Surgery 1964;88:984–7.
Larmi TK. Surgical Treatment of the Postcholecystectomy Syndrome. Annales Chirurgiae et Gynaecologiae Fenniae. 1963; 52:(suppl 126):1–24.
Stawowy M, Bluhme C, Arendt-Nielsen L, Drewes AM, Funch-Jensen P. Somatosensory changes in the referred pain area in patients with acute cholecystitis before and after treatment with laparoscopic or open cholecystectomy. Scandinavian Journal of Gastroenterology 2004;39:988–93.
Polymeneas G, Theodosopoulos T, Stamatiadis A, Kourias E. A comparative study of postoperative adhesion formation after laparoscopic vs open cholecystectomy. Surgical Endoscopy 2001;15:41–3.
Nagafuchi Y, Katuki M, Hisatome K, Higure A, Asami S, Itoh H. A traumatic neuroma associated with obstructive jaundice after laparoscopic cholecystectomy. Hepato-gastroenterology 1998;45:424–7.
Pernice LM, Andreoli F. Laparoscopic treatment of stone recurrence in a gallbladder remnant: report of an additional case and literature review. Journal of gastrointestinal surgery: Official journal of the Society for Surgery of the Alimentary Tract 2009;13:2084–91.
Karaliotas C, Sgourakis G, Goumas C, Papaioannou N, Lilis C, Leandros E. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surgical Endoscopy. 2008;22:1826–31.
Parmeggiani D, Cimmino G, Cerbone D, et al. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. Il Giornale di Chirurgia. 2010;31:16–9.
Kozarek R, Gannan R, Baerg R, Wagonfeld J, Ball T. Bile leak after laparoscopic cholecystectomy. Diagnostic and therapeutic application of endoscopic retrograde cholangiopancreatography. Archives of Internal Medicine 1992;152:1040–3.
Brady AP, McGrath FP, Moote DJ, Malone DE. Post-laparoscopic cholecystectomy bilomas—preliminary experience. Clinical Radiology. 1992;46:333–6.
Lasson A. The postcholecystectomy syndrome: diagnostic and therapeutic strategy. Scandinavian Journal of Gastroenterology 1987;22:897–902.
Seetharam P, Rodrigues G. Sphincter of Oddi and its dysfunction. Saudi journal of gastroenterology: Official Journal of the Saudi Gastroenterology Association. 2008;14:1–6.
Filip M, Saftoiu A, Popescu C, et al. Postcholecystectomy syndrome- an algorithmic approach. Journal of Gastrointestinal and Liver Diseases: JGLD. 2009;18:67–71.
Coelho-Prabhu N, Baron TH. Assessment of need for repeat ERCP during biliary stent removal after clinical resolution of postcholecystectomy bile leak. The American Journal of Gastroenterology 2010;105:100–5.
Tanaka M, Ikeda S, Matsumoto S, Yoshimoto H, Nakayama F. Manometric diagnosis of sphincter of Oddi spasm as a cause of postcholecystectomy pain and the treatment by endoscopic sphincterotomy. Annals of Surgery 1985;202:712–9.
Toouli J. Biliary scintigraphy versus sphincter of Oddi manometry in patients with post-cholecystectomy pain: is it time to disregard the scan? Current Gastroenterology Reports. 2005;7:154–9.
Yavorski CC, Acosta JA, Ragland JJ. Precholecystectomy esophagogastroduodenoscopy: is it of value? The American Surgeon. 1995;61:1032–4.
Madacsy L, Velosy B, Lonovics J, Csernay L. Evaluation of results of the prostigmine-morphine test with quantitative hepatobiliary scintigraphy: a new method for the diagnosis of sphincter of Oddi dyskinesia. European journal of nuclear medicine 1995;22:227–32.
Baillie J. Sphincter of Oddi dysfunction. Current Gastroenterology Reports 2010;12:130–4.
Saadah HA. Post-cholecystectomy biliary pain and dyspepsia (response to 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors). The Journal of the Oklahoma State Medical Association. 1994;87:315–8.
Geenen JE, Hogan WJ, Dodds WJ, Toouli J, Venu RP. The efficacy of endoscopic sphincterotomy after cholecystectomy in patients with sphincter-of-Oddi dysfunction. The New England Journal of Medicine. 1989;320:82–7.
Tzovaras G, Rowlands BJ. Transduodenal sphincteroplasty and transampullary septectomy for sphincter of Oddi dysfunction. Annals of the Royal College of Surgeons of England 2002;84:14–9.
Vitale GC, Tran TC, Davis BR, Vitale M, Vitale D, Larson G. Endoscopic management of postcholecystectomy bile duct strictures. Journal of the American College of Surgeons 2008;206:918–23; discussion 24-5.
Cimaschi D, De Cesare V, Pulcini G, et al. [A case of amputation neuroma of the bile duct following video-laparoscopic cholecystectomy]. Il Giornale di Chirurgia 2006;27:31–6.58.
Vetrhus M, Soreide O, Eide, et al. Pain and quality of life in patients with symptomatic, non-complicated gallbladder stones: results of a randomized controlled trial. Scand J Gastroenterol 2004;39:270–6.
Oort F. Using structural equation modeling to detect response shifts and true change. Quality of Life Research 2005;14:587–98.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kouloura, A., Sgourakis, G., Lanitis, S. et al. Enriched view of postcholecystectomy syndrome: Nowadays and in former times. Hellenic J Surg 87, 156–164 (2015). https://doi.org/10.1007/s13126-015-0201-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13126-015-0201-x
Key words
- Postcholecystectomy syndrome
- laparoscopic cholecystectomy
- open cholecystectomy
- remnant stones
- sphincter of Oddi dysfunction