Abstract
Background
Vitamin D plays a key role in gut immunity and maintenance of the mucosal barrier. Vitamin D deficiency (VDD) worsens ulcerative colitis (UC) and its supplementation ameliorates the disease in mouse models. The prevalence and predictors of VDD in UC are not known.
Methods
Consecutive patients with UC (n = 80) underwent clinical, endoscopic, and histological evaluation to assess the extent, severity using UC disease activity index (UCDAI) score, and duration of illness. An equal number of age and gender-matched healthy adults without any features of inflammatory bowel disease (IBD) living in the same latitude were identified as controls. The serum 25-hydroxy vitamin D3 level was estimated. The subjects were classified as deficient (< 20 ng/mL), insufficient (20–32 ng/mL), sufficient (32–80 ng/mL), and optimal (> 80 ng/mL) based on vitamin D levels. Chi-square test and Mann-Whitney U test were done to identify factors associated with vitamin D deficiency.
Results
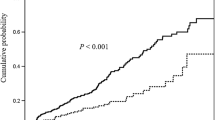
The patients and controls were similar in age and gender (40 ± 11.4 years, 51% male vs. 40 ± 12 years, 51% male; p = 1.000). Median vitamin D levels among patients were lower than the controls (18.1 ng/mL [IQR 14] vs. 32.5 ng/mL [IQR 36]; p < 0.001). Patients were more often VDD (56% vs. 40%) or insufficient (34% vs. 9%) and less often sufficient (9% vs. 40%) or optimal (1% vs. 11%), in contrast to controls (p < 0.001). Median vitamin D levels were lower in those with UCDAI > 6 (15 vs. 21 ng/mL; p = 0.01), having pancolitis (13 vs. 21 ng/mL, p = 0.01), and longer duration of illness > 2 years (13.8 vs. 20.8; p = 0.025). Vitamin D levels showed a negative correlation with frequency of stools (rho = − 0.244, p = 0.05), disease duration (rho = − 0.244, p = 0.007) and UCDAI score (r = − 0.348, p = 0.002).
Conclusion
VDD is highly prevalent among patients with UC. Patients with longer disease duration, more severe symptoms, and pancolitis are likely to have lower vitamin D levels.


Similar content being viewed by others
References
Bernstein CN, Leslie WD, Leboff MS. AGA technical review of osteoporosis in gastrointestinal diseases. Gastroenterology. 2003;124:795–841.
Cantorna MT, Zhu Y, Froicu M, Wittke A. Vitamin D status, 1,25-dihydroxyvitamin D3, and the immune system. Am J Clin Nutr. 2004;80 6 Suppl:1717S–20S.
Deluca HF, Cantorna MT. Vitamin D: its role and uses in immunology. FASEB J. 2001;15:2579–85.
Cantorna MT. Vitamin D and its role in immunology: multiple sclerosis, and inflammatory bowel disease. Prog Biophys Mol Biol. 2006;92:60–4.
Veldman CM, Cantorna MT, DeLuca HF. Expression of 1,25-dihydroxyvitamin D3 receptor in the immune system. Arch Biochem Biophys. 2000;374:334–8.
Gerd Bouma WS. The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol. 2003;3:521–33.
Froicu M, Weaver V, Wynn TA, McDowell MA, Welsh JE, Cantorna MT. A crucial role for the vitamin D receptor in experimental inflammatory bowel diseases. Mol Endocrinol. 2003;17:2386–92.
Froicu M, Zhy Y, Cantorna MT. Vitamin D receptor is required to control gastrointestinal immunity in IL-10 knockout mice. Immunology. 2006;117:310–8.
Cantorna MT, Munsick C, Bemiss C, Mahon BD. 1,25-dihydroxycholecalciferol prevents and ameliorates symptoms of experimental murine inflammatory bowel disease. J Nutr. 2000;130:2648–52.
Pappa HM, Grand RJ, Gordon CM. Report on the vitamin D status of adult and pediatric patients with inflammatory bowel disease and its significance for bone health and disease. Inflamm Bowel Dis. 2006;12:1162–74.
Vogelsang H, Klamert M, Resch H, Ferenci P. Dietary vitamin D intake in patients with Crohn’s disease. Wien Klin Wochenschr. 1995;107:578–81.
Jowett SL, Seal CJ, Phillips E, Gregory W, Barton JR, Welfare MR. Dietary beliefs of people with ulcerative colitis and their effect on relapse and nutrient intake. Clin Nutr. 2004;23:161–70.
Bartram SA, Peaston RT, Rawlings DJ, Francis RM, Thompson NP. A randomized controlled trial of calcium with vitamin D, alone or in combination with intravenous pamidronate, for the treatment of low bone mineral density associated with Crohn’s disease. Aliment Pharmacol Ther. 2003;18:1121–7.
Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults (update): American College of Gastroenterology, Practice Parameters Committee. Am Gastroenterol. 2004;99:1371–85.
Schroeder KW, Tremaine WJ, Illstrup DM. Coated oral 5ASA therapy for mildly to moderately active disease. N Engl J Med. 1987;317:1625–9.
Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805–6.
Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22:142–6.
Lips P. Which circulating level of 25-hydroxy vitamin D is appropriate? J Steroid Biochem Mol Biol. 2004;89-90:611–4.
Leslie WD, Miller N, Rogala L, Bernstein CN. Vitamin D status and bone density in recently diagnosed inflammatory bowel disease: the Manitoba IBD cohort study. Am J Gastroenterol. 2008;103:1451–9.
Joseph AJ, George B, Pulimood AB, Seshadri MS, Chacko A. 25 (OH) vitamin D level in Crohn’s disease: association with sun exposure and disease activity. Indian J Med Res. 2009;130:133–7.
Harinarayan CV, Ramalakshmi T, Prashad UV, et al. High prevalence of low dietary calcium, high phytate consumption, and vitamin D deficiency in healthy south Indians. Am J Clin Nutr. 2007;85:1062–7.
Harinarayan CV, Joshi SR. Vitamin D status in India – its implications and remedial measures. J Assoc Physicians India. 2009;57:40–8.
Goswami R, Gupta N, Goswami D, Marwaha RK, Tandon N, Kochupillai N. Prevalence and significance of low 25-hydroxyvitamin D concentrations in healthy subjects in Delhi. Am J Clin Nutr. 2000;72:472–5.
Goswami R, Mishra SK, Kochupillai N. Prevalence and potential significance of vitamin D deficiency in Asian Indians. Indian J Med Res. 2008;127:229–38.
Agarwal KS, Mughal MZ, Upadhyay P, Berry JL, Mawer EB, Puliyel JM. The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi. India Arch Dis Child. 2002;87:111–3.
Saitoh O, Matsumoto H, Sugimori K, et al. Intestinal protein loss and bleeding assessed by fecal hemoglobin, transferrin, albumin, and alpha-1-antitrypsin levels in patients with colorectal diseases. Digestion. 1995;56:67–75.
Haddad JG. Plasma vitamin D-binding protein (Gc-globulin): multiple tasks. J Steroid Biochem Mol Biol. 1995;53:579–82.
Sahu M, Bhatia V, Aggarwal A, et al. Vitamin D deficiency in rural girls and pregnant women despite abundant sunshine in northern India. Clin Endocrinol. 2009;70:680–4.
Opstelten JL, Chan SSM, Hart AR, et al. Prediagnostic serum vitamin D levels and the risk of Crohn's disease and ulcerative colitis in European populations: a nested case-control study. Inflamm Bowel Dis. 2018;24:633–40.
Gubatan J, Mitsuhashi S, Zenlea T, Rosenberg L, Robson S, Moss AC. Low serum vitamin D during remission increases risk of clinical relapse in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2017;15:240–246.e1.
Sharifi A, Hosseinzadeh-Attar MJ, Vahedi H, Nedjat S. A randomized controlled trial on the effect of vitamin D3 on inflammation and cathelicidin gene expression in ulcerative colitis patients. Saudi J Gastroenterol. 2016;22:316–23.
Chatu S, Chhaya V, Holmes R, et al. Factors associated with vitamin D deficiency in a multicultural inflammatory bowel disease cohort. Frontline Gastroenterol. 2013;4:51–6.
Del Pinto R, Pietropaoli D, Chandar AK, Ferri C, Cominelli F. Association between inflammatory bowel disease and vitamin D deficiency: a systematic review and meta-analysis. Inflamm Bowel Dis. 2015;21:2708–17.
Frigstad SO, Høivik M, Jahnsen J, et al. Vitamin D deficiency in inflammatory bowel disease: prevalence and predictors in a Norwegian outpatient population. Scand J Gastroenterol. 2017;52:100–6.
Zheng SZ, Zhang DG, Wu H, et al. The association between vitamin D receptor polymorphisms and serum 25-hydroxyvitamin D levels with ulcerative colitis in Chinese Han population. Clin Res Hepatol Gastroenterol. 2017;41:110–7.
Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D and fluoride. Washington, DC: The National Academies Press; 1997.
Jorgensen SP, Agnholt J, Glerup H, et al. Clinical trial : vitamin D3 treatment in Crohn’s disease – a randomized double-blind placebo-controlled study. Aliment Pharmacol Ther. 2010;32:377–83.
Papaioannou A, Ferko NC, Adachi JD. All patients with inflammatory bowel disease should have bone density assessment. Inflamm Bowel Dis. 2001;7:158–62.
Khandgawat R, Makharia GK, Puri K. Evaluation of bone mineral density among patients with inflammatory bowel disease in a tertiary care setting in India. Indian J Gastroenterol. 2008;27:103–6.
Acknowledgments
We would like to acknowledge the efforts of Dr. Sharonjeet Kaur, Anu Sharma, and Neha Thakur for their assistance in data compilation and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ADL, UD, RK, CV, SK, TN, SB, and KS declare that they have no conflict of interest.
Ethical clearance
The authors declare that the study was performed in a manner conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Law, A.D., Dutta, U., Kochhar, R. et al. Vitamin D deficiency in adult patients with ulcerative colitis: Prevalence and relationship with disease severity, extent, and duration. Indian J Gastroenterol 38, 6–14 (2019). https://doi.org/10.1007/s12664-019-00932-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-019-00932-z