Abstract
Introduction
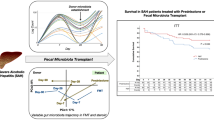
Alcohol-induced intestinal dysbiosis is central to the development of the severe alcoholic liver disease. We present the first study to compare outcomes in patients of severe alcoholic hepatitis (SAH) on nutritional therapy, corticosteroids, pentoxifylline, and healthy donor fecal transplantation (FMT) and discuss distinct microbial community and microbiome metabolic functional changes after FMT.
Methods
Out of 1271 liver disease patients, 809 (63.7%) were diagnosed to have the alcoholic liver disease, of which 51 patients (8 treated with corticosteroids, 17 with nutritional support only, 10 with pentoxifylline, 16 receiving FMT) were included. Clinical, biochemical parameters, liver disease, and alcoholic hepatitis severity scores at baseline and mortality at the end of 1 and 3 months were analyzed between groups. Stool microbiota (SM) analysis was performed for healthy controls (HC) and respective recipients after FMT.
Results
All the patients were male. The proportions of patients surviving at the end of 1 and 3 months in the steroids, nutrition, pentoxifylline, and FMT group were 63%, 47%, 40% and 75% [p = 0.179] and 38%, 29%, 30%, and 75% [p = 0.036], respectively. When compared with FMT, relative risk and hazard ratios for death were higher in all the other groups. Following FMT, distinct and beneficial modulation of SM and pathways of dysregulated metabolism, infections, inflammation, and oxidative stress in SAH patients were noted in tandem with improved clinical outcomes.
Conclusions
Healthy donor FMT for SAH improves survival beyond what is offered by current therapies and can function as a cost-effective bridge to liver transplant (LT) or for improving transplant-free survival. Larger studies and randomized trials are unmet needs.





Similar content being viewed by others
References
Crabb DW, Bataller R, Chalasani NP, et al. Standard definitions and common data elements for clinical trials in patients with alcoholic hepatitis: recommendation from the NIAAA Alcoholic Hepatitis Consortia. Gastroenterology. 2016;150:785–90.
Maddrey WC, Boitnott JK, Bedine MS, Weber FL Jr, Mezey E, White RI Jr. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–9.
Mathurin P, O’Grady J, Carithers RL, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60:255–60.
Vergis N, Knapp S, Maurice J, et al. In patients with severe alcoholic hepatitis, prednisolone increases susceptibility to infection and infection-related mortality, and is associated with high circulating levels of bacterial DNA. Gastroenterology. 2017;152:1068–77.
Addolorato G, Bataller R, Burra P, et al. Liver transplantation for alcoholic liver disease. Transplantation. 2016;100:981–7.
Hartl J, Scherer MN, Loss M, et al. Strong predictors for alcohol recidivism after liver transplantation: non-acceptance of the alcohol problem and abstinence of <3 months. Scand J Gastroenterol. 2011;46:1257–66.
Sidhu SS, Goyal O, Kishore H, Sidhu S. New paradigms in management of alcoholic hepatitis: a review. Hepatol Int. 2017;11:255–67.
Ferrere G, Wrzosek L, Cailleux F, et al. Fecal microbiota manipulation prevents dysbiosis and alcohol-induced liver injury in mice. J Hepatol. 2017;66:806–15.
Philips CA, Pande A, Shasthry SM, et al. Healthy donor fecal microbiota transplantation in steroid ineligible severe alcoholic hepatitis: a pilot study. Clin Gastroenterol Hepatol. 2017;15:600–2.
Llopis M, Cassard AM, Wrzosek L, et al. Intestinal microbiota contributes to individual susceptibility to alcoholic liver disease. Gut. 2016;65:830–9.
Moreno C, Deltenre P, Senterre C, et al. Intensive enteral nutrition is ineffective for patients with severe alcoholic hepatitis treated with corticosteroids. Gastroenterology. 2016;150:903–10.e8.
Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015;372:1619–28.
Zhu L, Baker SS, Gill C, et al. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH. Hepatology. 2013;57:601–9.
Nakahara T, Hyogo H, Ono A, et al. Involvement of Porphyromonas gingivalis in the progression of non-alcoholic fatty liver disease. J Gastroenterol. 2018;53:269–80.
Chen Y, Ji F, Guo J, Shi D, Fang D, Lib L. Dysbiosis of small intestinal microbiota in liver cirrhosis and its association with etiology. Sci Rep. 2016;6:34055.
Dam G, Vilstrup H, Watson H, Jepsen P. Proton pump inhibitors as a risk factor for hepatic encephalopathy and spontaneous bacterial peritonitis in patients with cirrhosis with ascites. Hepatology. 2016;64:1265–72.
Chen Y, Yang F, Lu H, et al. Characterization of fecal microbial communities in patients with liver cirrhosis. Hepatology. 2011;54:562–72.
Bajaj JS, Ridlon JM, Hylemon PB, et al. Linkage of gut microbiome with cognition in hepatic encephalopathy. Am J Physiol Gastrointest Liver Physiol. 2012;302:G168–75.
Bajaj JS, Hylemon PB, Heuman DM, et al. The cirrhosis dysbiosis ratio defines changes in the gut microbiome associated with cirrhosis and its complications. Hepatology. 2014;60:940–7.
Li SS, Zhu A, Benes V, et al. Durable coexistence of donor and recipient strains after fecal microbiota transplantation. Science. 2016;29:586–9.
Oikawa T. Alanine, aspartate, and asparagine metabolism in microorganisms. In: Wendisch VF. eds. Amino acid biosynthesis—pathways, regulation and metabolic engineering. Microbiology Monographs. Vol 5. 2006. Springer, Berlin, Heidelberg.
Calder PC. Branched-chain amino acids and immunity. J Nutr. 2006;136 1 Suppl:288S–93S.
Tajiri K, Shimizu Y. Branched-chain amino acids in liver diseases. World J Gastroenterol. 2013;19:7620–9.
Neuman MG, Maor Y, Nanau RM, et al. Alcoholic liver disease: role of cytokines. Biomolecules. 2015; 5: 2023–34.
Odena G, Chen J, Lozano JJ, et al. LPS-TLR4 pathway mediates ductular cell expansion in alcoholic hepatitis. Sci Rep. 2016;6:35610.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CAP, NP, KG, SR, and PA declare that they have no conflict of interest.
Ethics statement
All procedures performed in studies involving human participants were by the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Philips, C.A., Phadke, N., Ganesan, K. et al. Corticosteroids, nutrition, pentoxifylline, or fecal microbiota transplantation for severe alcoholic hepatitis. Indian J Gastroenterol 37, 215–225 (2018). https://doi.org/10.1007/s12664-018-0859-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-018-0859-4