Abstract
Objective
The aim of study was to determine the association between signs of temporomandibular disorders (TMD), occlusal support, and alterations in the craniofacial structure of elderly Vietnamese by using cephalometric analysis.
Methods
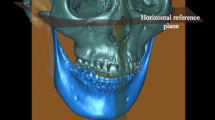
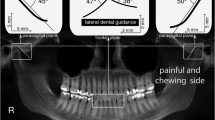
The cross-sectional study consisted of 244 participants aged 65–74 years. Participants were examined for signs of TMD, including limited mouth opening, temporomandibular joint (TMJ) crepitus, TMJ tenderness, and muscle tenderness. Dentition was divided into four occlusal support zones based on occluding pairs of posterior teeth by using Eichner’s classification: Class A = 4 support zones; Class B = 1–3 support zones or only contact in anterior teeth; Class C = 0 support zones. Fifteen angular and seven linear parameters were used for sagittal craniofacial skeleton analysis.
Results
10.3% of participants had limited mouth opening, 49.6% TMJ crepitus, 16.3% TMJ tenderness, and 24.2% muscle tenderness; 45.5% had Class A occlusal support, 38.5% Class B, and 16.0% Class C. Those with Class C had significantly smaller ramus inclination, articular angle, and angles formed by the mandibular plane and shorter facial height compared to Class A and Class B (P < .001). TMD signs were significantly associated with: angles formed by mandibular plane, gonial angle, cranial base angle, effective mandibular length, and anterior facial height (P < .05).
Conclusions
The alteration of craniofacial structures was significantly associated with TMD signs among elderly Vietnamese. The higher number of lost occlusal support zones, the more significant the changes to craniofacial structures.




Similar content being viewed by others
References
Ikebe K, Hazeyama T, Iwase K, Sajima H, Gonda T, Maeda Y et al (2008) Association of symptomless TMJ sounds with occlusal force and masticatory performance in older adults. J Oral Rehabil 35:317–323
Schmitter M, Rammelsberg P, Hassel A (2005) The prevalence of signs and symptoms of temporomandibular disorders in very old subjects. J Oral Rehabil 32:467–473
Gesch D, Bernhardt O, Alte D, Schwahn C, Kocher T, John U et al (1985) Prevalence of signs and symptoms of temporomandibular disorders in an urban and rural German population: results of a population-based Study of Health in Pomerania. Quintessence Int Berl Ger 2004(35):143–150
Moreno-Hay I, Okeson JP (2015) Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J Oral Rehabil 42:875–882
Hiltunen K, Vehkalahti M, Ainamo A (1997) Occlusal imbalance and temporomandibular disorders in the elderly. Acta Odontol Scand 55:137–141
Tavano KTA, Seraidarian PI, de Oliveira DD, Jansen WC (2012) Determination of vertical dimension of occlusion in dentate patients by cephalometric analysis–pilot study. Gerodontology 29:e297–e305
Brzoza D, Barrera N, Contasti G, Hernández A (2005) Predicting vertical dimension with cephalograms, for edentulous patients. Gerodontology 22:98–103
Huumonen S, Sipilä K, Haikola B, Tapio M, Söderholm A-L, Remes-Lyly T et al (2010) Influence of edentulousness on gonial angle, ramus and condylar height. J Oral Rehabil 37:34–38
Merrot O, Vacher C, Merrot S, Godlewski G, Frigard B, Goudot P (2005) Changes in the edentate mandible in the elderly. Surg Radiol Anat SRA 27:265–270
Uma M, Shetty R, Shenoy KK (2013) Cephalometric: evaluation of influence of edentulousness on mandibular morphology: a comparative study. J Indian Prosthodont Soc 13:269–273
Ahn SJ, Baek SH, Kim TW, Nahm DS (2006) Discrimination of internal derangement of temporomandibular joint by lateral cephalometric analysis. Am J Orthod Dentofacial Orthop 130:331–339
Chen S, Lei J, Fu KY, Wang X, Yi B (2015) Cephalometric analysis of the facial skeletal morphology of female patients exhibiting skeletal class II deformity with and without temporomandibular joint osteoarthrosis. PLoS ONE 10:e0139743
Emshoff R, Moriggl A, Rudisch A, Brunold S, Neunteufel N, Crismani A (2011) Cephalometric variables discriminate among magnetic resonance imaging-based structural characteristic groups of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112:118–125
Matsumoto R, Ioi H, Nishioka M, Goto TK, Nakata S, Nakasima A et al (2006) TMJ osteoarthritis/osteoarthrosis and dentofacial morphology in Japanese females. Orthod Waves 65:101–106
Matsuo Y, Kajii TS, Yasunaga M, Sakaguchi Y, Tamaoki S, Ishikawa H (2016) Characteristics of maxillofacial morphology of angle class II patients with temporomandibular disorders involving crepitus. Orthod Waves 75:27–34
Xie Q, Yang C, He D, Cai X, Ma Z, Shen Y et al (2016) Will unilateral temporomandibular joint anterior disc displacement in teenagers lead to asymmetry of condyle and mandible? A longitudinal study. J Cranio-Maxillofac Surg 44:590–596
Selaimen CMP, Jeronymo JCM, Brilhante DP, Lima EM, Grossi PK, Grossi ML (2007) Occlusal risk factors for temporomandibular disorders. Angle Orthod 77:471–477
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet J-P et al (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 28:6–27
Eichner K (1990) Renewed examination of the group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics. Stomatol DDR 40:321–325
Okşayan R, Asarkaya B, Palta N, Şimşek İ, Sökücü O, İşman E (2014) Effects of edentulism on mandibular morphology: evaluation of panoramic radiographs. Sci World J 2014:254932
Rosa WGN, de Lima Navarro R, de Castro Ferreira Conti AC, de Almeida MR, Oltramari-Navarro PVP (2015) Assessment of cephalometric characteristics in the elderly. Braz Oral Res 29:1–9
Shimizu T, Motegi E, Nomura M, Kaneko Y, Takeuchi F, Yamaguchi T et al (2006) Cephalometric study of elderly with nearly intact dental arches. Gerodontology 23:60–63
Türp JC, Schindler H (2012) The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil 39:502–512
Sipilä K, Näpänkangas R, Könönen M, Alanen P, Suominen AL (2013) The role of dental loss and denture status on clinical signs of temporomandibular disorders. J Oral Rehabil 40:15–23
Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A et al (2008) Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain 22:239–251
Krisjane Z, Urtane I, Krumina G, Neimane L, Ragovska I (2012) The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study. Int J Oral Maxillofac Surg 41:690–695
Ioi H, Matsumoto R, Nishioka M, Goto TK, Nakata S, Nakasima A et al (2008) Relationship of TMJ osteoarthritis/osteoarthrosis to head posture and dentofacial morphology. Orthod Craniofac Res 11:8–16
Acknowledgements
This study was supported by an Estonian Science Foundation Grant (No. 9255), the Estonian Research Council Grant IUT 20–46, and the European Social Fund’s Doctoral Studies and Internationalisation Programme DoRa, which is carried out by Archimedes Foundation. The authors would also like to thank the Unimed United Clinics, Estonia, for their support in analyzing occlusion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Nguyen, M.S., Saag, M., Voog-Oras, Ü. et al. Temporomandibular Disorder Signs, Occlusal Support, and Craniofacial Structure Changes Among the Elderly Vietnamese. J. Maxillofac. Oral Surg. 17, 362–371 (2018). https://doi.org/10.1007/s12663-017-1057-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-017-1057-0