Abstract
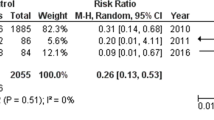
Alterations of intestinal microflora are involved in the pathogenesis and natural history of inflammatory bowel diseases (IBDs). Manipulation of human gut microbiota with probiotics may be a therapeutic option. In this retrospective cohort study, the benefits of probiotic use in reducing adverse events were analyzed. Data from clinical charts of IBD patients followed up for at least 36 months were retrieved. The occurrence of adverse events including the need for systemic steroids, hospitalization, and surgery related to IBD was analyzed according to age, gender, body mass index, treatments, IBD phenotype, disease duration, and probiotic use. The amount of probiotic use was calculated as the ratio of time under probiotic treatment to the disease duration starting from the date of the first probiotic administration and expressed as a percentage. Patients were stratified according to the percentage of probiotic use as ≤ 24%, 25–74%, and ≥ 75%, and the number of adverse events per patient-years was calculated. Results were adjusted for Crohn’s disease (CD) and ulcerative colitis (UC) by multivariate analysis including study variables. Data from 200 patients (78 CD, 122 UC; 117 females; mean age 40.6 ± 15.3 years; mean disease duration 12.1 ± 8.7 years) were available. CD patients taking probiotics for 25–74% of the disease duration experienced a 64% reduction in total adverse events. The need for systemic steroids, hospitalization, and surgery dropped to zero events per person-year in UC patients and decreased by 93% (p < 0.001) in CD patients taking probiotics for ≥ 75% of the disease duration. Our findings suggest that the use of probiotics may be an additional therapeutic tool in patients with IBD.

Similar content being viewed by others
References
Podolsky DK (2002) Inflammatory bowel disease. N Engl J Med 347:417–429. https://doi.org/10.1056/NEJMra020831
Shivashankar R, Tremaine WJ, Harmsen WS, Loftus EV Jr (2017) Incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol 15:857–863. https://doi.org/10.1016/j.cgh.2016.10.039
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG (2018) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390:2769–2778. https://doi.org/10.1016/S0140-6736(17)32448-0
Vermeire S, van Assche G, Rutgeerts P (2007) Altering the natural history of Crohn’s disease – evidence for and against current therapies. Aliment Pharmacol Ther 25:3–12. https://doi.org/10.1111/j.1365-2036.2006.03134.x
Beaugerie L, Kirchgesner J (2018) Balancing benefit vs risk of immunosuppressive therapy for individual patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2018.07.013
Fiocchi C (2015) Inflammatory bowel disease pathogenesis: where are we? J Gastroenterol Hepatol 30(Suppl 1):12–18. https://doi.org/10.1111/jgh.12751
Garrett WS, Lord GM, Punit S, Punit S, Lugo-Villarino G, Mazmanian SK et al (2007) Communicable ulcerative colitis induced by T-bet deficiency in the innate immune system. Cell 131:33–45. https://doi.org/10.1016/j.cell.2007.08.017
Elinav E, Strowig T, Kau AL, Henao-Mejia J, Thaiss CA, Booth CJ, Peaper DR, Bertin J, Eisenbarth SC, Gordon JI, Flavell RA (2011) NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell 145:745–757. https://doi.org/10.1016/j.cell.2011.04.022
Shukla PK, Meena AS, Manda B, Gomes-Solecki M, Dietrich P, Dragatsis I, Rao R (2018) Lactobacillus plantarum prevents and mitigates alcohol-induced disruption of colonic epithelial tight junctions, endotoxemia, and liver damage by an EGF receptor-dependent mechanism. FASEB J. https://doi.org/10.1096/fj.201800351R
Singh TP, Kaur G, Kapila S, Malik RK (2017) Antagonistic activity of Lactobacillus reuteri strains on the adhesion characteristics of selected pathogens. Front Microbiol 8:486. https://doi.org/10.3389/fmicb.2017.00486
Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, Doyle J, Jewell L, de Simone C (2001) Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 121:580–591. https://doi.org/10.1053/gast.2001.27224
Höltzel A, Gӓnzle MG, Nicholson GJ (2000) The first low molecular weight antibiotic from lactic acid bacteria: reutericyclin, a new tetramic acid. Angew Chem Int Ed Engl 39:2766–2768. https://doi.org/10.1002/1521-3773(20000804)39:15<2766::AID-ANIE2766>3.0.CO;2-G
Mukai T, Asasaka T, Sato E, Mori K, Matsumoto M, Ohori H (2002) Inhibition of binding of Helicobacter pylori to the glycolipid receptors by probiotic Lactobacillus reuteri. FEMS Immunol Med Microbiol 32:105–110. https://doi.org/10.1111/j.1574-695X.2002.tb00541.x
La Fata G, Weber P, Mohajeri MH (2018) Probiotics and the gut immune system: indirect regulation. Probiotics Antimicrob Proteins 10:11–21. https://doi.org/10.1007/s12602-017-9322-6
Elbanna K, El Hadad S, Assaeedi A (2018) In vitro and in vivo evidences for innate immune stimulators lactic acid bacterial starters isolated from fermented camel dairy products. Sci Rep 8:12553. https://doi.org/10.1038/s41598-018-31006-3
Kruis W, Fric P, Pokrotnieks J, Lukás M, Fixa B, Kascák M, Kamm MA, Weismueller J, Beglinger C, Stolte M, Wolff C, Schulze J (2004) Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 53:1617–1623. https://doi.org/10.1136/gut.2003.037747
Kruis W, Schütz E, Fric P, Fixa B, Judmaier G, Stolte M (1997) Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Aliment Pharmacol Ther 11:853–858. https://doi.org/10.1046/j.1365-2036.1997.00225.x
Matthes H, Krummenerl T, Giensch M, Wolff C, Schulze J (2010) Clinical trial: probiotic treatment of acute distal ulcerative colitis with rectally administered Escherichia coli Nissle 1917 (EcN). BMC Complement Altern Med 10:13. https://doi.org/10.1186/1472-6882-10-13
Petersen AM, Mirsepasi H, Halkjær SI, Mortensen EM, Nordgaard-Lassen I, Krogfelt KA (2014) Ciprofloxacin and probiotic Escherichia coli Nissle add-on treatment in active ulcerative colitis: a double-blind randomized placebo controlled clinical trial. J Crohns Colitis 8:1498–1505. https://doi.org/10.1016/j.crohns.2014.06.001
Kato K, Mizuno S, Umesaki Y, Ishii Y, Sugitani M, Imaoka A, Otsuka M, Hasunuma O, Kurihara R, Iwasaki A, Arakawa Y (2004) Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther 20:1133–1141. https://doi.org/10.1111/j.1365-2036.2004.02268.x
Sood A, Midha V, Makharia GK, Ahuja V, Singal D, Goswami P, Tandon RK (2009) The probiotic preparation, VSL#3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin Gastroenterol Hepatol 11:1202–1209. https://doi.org/10.1016/j.cgh.2009.07.016
Tamaki H, Nakase H, Inoue S, Kawanami C, Itani T, Ohana M, Kusaka T, Uose S, Hisatsune H, Tojo M, Noda T, Arasawa S, Izuta M, Kubo A, Ogawa C, Matsunaka T, Shibatouge M (2016) Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: a randomized, double-blinded, placebo-controlled multicenter trial. Dig Endosc 28:67–74. https://doi.org/10.1111/den.12553
Derwa Y, Gracie DJ, Hamlin PJ, Ford AC (2017) Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther 46:389–400. https://doi.org/10.1111/apt.14203
Koretz RL (2018) Probiotics in gastroenterology: how pro is the evidence in adults? Am J Gastroenterol 113:1125–1136. https://doi.org/10.1038/s41395-018-0138-0
Satta R, Pes GM, Rocchi C, Pes MC, Dore MP (2018) Is probiotic use beneficial for skin lesions in patients with inflammatory bowel disease? J Dermatol Treat 19:1–5. https://doi.org/10.1080/09546634.2018.1527998
Lambert D (1992) Zero-inflated Poisson regression, with an application to defects in manufacturing. Technometrics 34:1–14
Efron B, Tibshirani R (1993) An introduction to the bootstrap. Chapman & Hall, New York
Schultz M, Timmer A, Herfarth HH, Sartor RB, Vanderhoof JA, Rath HC (2004) Lactobacillus GG in inducing and maintaining remission of Crohn’s disease. BMC Gastroenterol 4:5. https://doi.org/10.1186/1471-230X-4-5
Malchow HA (1997) Crohn’s disease and Escherichia coli. A new approach in therapy to maintain remission of colonic Crohn’s disease? J Clin Gastroenterol 25:653–658
Ganji-Arjenaki M, Rafieian-Kopaei M (2018) Probiotics are a good choice in remission of inflammatory bowel diseases: a meta-analysis and systematic review. J Cell Physiol 233:2091–2103. https://doi.org/10.1002/jcp.25911
Willert RP, Peddi KK, Ombiga J, Bampton PA, Lawrance IC (2010) Randomised, double-blinded, placebo-controlled study of VSL#3 versus placebo in the maintenance of remission in Crohns disease. Gastroenterology 138:S-517. https://doi.org/10.1016/S0016-5085(10)62390-6
Bourreille A, Cadiot G, Le Dreau G, Laharie D, Beaugerie L, Dupas JL et al (2013) Saccharomyces boulardii does not prevent relapse of Crohn’s disease. Clin Gastroenterol Hepatol 11:982–987. https://doi.org/10.1016/j.cgh.2013.02.021
Guslandi M, Mezzi G, Sorghi M, Testoni PA (2000) Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci 45:1462–1464. https://doi.org/10.1023/A:1005588911207
Katz M (2012) Study design and statistical analysis: a practical guide for clinicians, 2006. In: Wanburg C (ed) The Oxford handbook of organizational socialization. https://doi.org/10.1017/CBO9780511616761
To N, Gracie DJ, Ford AC (2016) Systematic review with meta-analysis: the adverse effects of tobacco smoking on the natural history of Crohn’s disease. Aliment Pharmacol Ther 43:549–561. https://doi.org/10.1111/apt.13511
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from each patient enrolled. The study was approved by the Local Ethics Committee, Comitato di Bioetica, Azienda Ospedaliero Universitaria di Sassari, Italy (Prot. No. 2476/CE.), and the 1975 Declaration of Helsinki guidelines were followed.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dore, M.P., Rocchi, C., Longo, N.P. et al. Effect of Probiotic Use on Adverse Events in Adult Patients with Inflammatory Bowel Disease: a Retrospective Cohort Study. Probiotics & Antimicro. Prot. 12, 152–159 (2020). https://doi.org/10.1007/s12602-019-9517-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-019-9517-0