Abstract
Purpose
Depression and anxiety are highly comorbid psychiatric conditions and both are common in adult patients with migraine. This study aims to examine the unique associations between major depressive disorder (MDD) and generalized anxiety disorder (GAD) in a well-characterized group of older adolescents and college-age individuals with migraine.
Method
Participants (N = 227), between 15 and 20 years old, who were unmedicated or within 1 month of beginning antidepressant treatment underwent a comprehensive psychiatric assessment to establish the presence of MDD and GAD, according to the Diagnostic and Statistical Manual, Fourth Edition, Text Revision, and to rate their symptom severity using the Longitudinal Interval Follow-up Evaluation for Adolescents (A-LIFE). They then completed the ID-Migraine. The Student’s t test and chi-square test were used to compare continuous and categorical variables, respectively, across participants with vs. without migraine. Logistic regression analysis examined the association between the presence of migraine and psychopathology.
Results
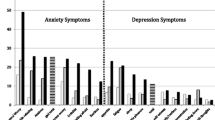
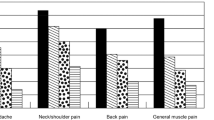
A diagnosis of MDD was associated with significantly increased risk of having migraine. Moreover, more severe and persistent ratings of depression were associated with an even higher likelihood of having migraine. A diagnosis of GAD was also significantly associated with the presence of migraine. The prevalence of comorbid MDD and GAD was significantly higher in participants with migraine than those without migraine (55 vs. 22%, p < 0.0001). When examined concurrently, GAD remained significantly associated with migraine, with a statistical trend for MDD to be associated with it.
Conclusion
The comorbidity of migraine, MDD, and GAD has important clinical and research implications. Patients who suffer from any of these problems should be screened for all three in order to receive comprehensive care. Shared psychological and biological vulnerabilities may be involved in the three conditions. Greater understanding of the shared vulnerabilities can lead to unified treatments.
Similar content being viewed by others
Notes
This study was launched in 2010, well before the DSM-5 became available, and new patient enrollment also ended before DSM-5 was released. The diagnostic criteria for major depression and GAD were not substantially modified in DSM-5.
Migraine is more prevalent in females than in males. The prevalence of migraine also varies by age. Thus, we adjusted for these two necessary variables. Adjusting for SSRI use was undertaken in the relevant analyses to confirm that migraine/SSRI-induced headaches were not conflated by this confounder.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, D.C.: American Psychiatric Association; 2000.
Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379:1056–67.
Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49:980–9.
Smitherman TA, McDermott MJ, Buchanan EM. Negative impact of episodic migraine on a university population: quality of life, functional impairment, and comorbid psychiatric symptoms. Headache. 2011;51:581–9.
Abu-Arafeh I, Razak S, Sivaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52:1088–97.
Antonaci F, Nappi G, Galli F, Manzoni GC, Calabresi P, Costa A. Migraine and psychiatric comorbidity: a review of clinical findings. The journal of headache and pain. 2011;12:115–25.
Radat F, Swendsen J. Psychiatric comorbidity in migraine: a review. Cephalalgia : an international journal of headache. 2005;25:165–78.
Bektas O, Ugur C, Gencturk ZB, Aysev A, Sireli O, Deda G. Relationship of childhood headaches with preferences in leisure time activities, depression, anxiety and eating habits: a population-based, cross-sectional study. Cephalalgia: an international journal of headache. 2015;35:527–37.
Lu SR, Fuh JL, Wang SJ, Juang KD, Chen SP, Liao YC, Wang YF. Incidence and risk factors of chronic daily headache in young adolescents: a school cohort study. Pediatrics. 2013;132:e9–e16.
Pakalnis A, Gibson J, Colvin A. Comorbidity of psychiatric and behavioral disorders in pediatric migraine. Headache. 2005;45:590–6.
Yacob D, Di Lorenzo C, Bridge JA, Rosenstein PF, Onorato M, Bravender T, Campo JV. Prevalence of pain-predominant functional gastrointestinal disorders and somatic symptoms in patients with anxiety or depressive disorders. J Pediatr. 2013;163:767–70.
Bellini B, Arruda M, Cescut A, Saulle C, Persico A, Carotenuto M, Gatta M, Nacinovich R, Piazza FP, Termine C, Tozzi E, Lucchese F, Guidetti V. Headache and comorbidity in children and adolescents. The journal of headache and pain. 2013;14:79.
Arruda MA, Bigal ME. Behavioral and emotional symptoms and primary headaches in children: a population-based study. Cephalalgia : an international journal of headache. 2012;32:1093–100.
Balottin U, Chiappedi M, Rossi M, Termine C, Nappi G. Childhood and adolescent migraine: a neuropsychiatric disorder? Med Hypotheses. 2011;76:778–81.
Kowal A, Pritchard D. Psychological characteristics of children who suffer from headache: a research note. Journal of child psychology and psychiatry, and allied disciplines. 1990;31:637–49.
Laurell K, Larsson B, Eeg-Olofsson O. Headache in schoolchildren: association with other pain, family history and psychosocial factors. Pain. 2005;119:150–8.
Calarge CA, Butcher BD, Burns TL, Coryell WH, Schlechte JA, Zemel BS. Major depressive disorder and bone mass in adolescents and young adults. J Bone Miner Res. 2014;29(10):2230–7.
Coryell WH, Butcher BD, Dindo LN, Schlechte JA and Calarge CA. Fat distribution and major depressive disorder in late adolescence. J Clin Psychiatry. In Press.
Deumic E, Butcher BD, Clayton AD, Dindo LN, Burns TL, Calarge CA. Sexual functioning in adolescents with major depressive disorder. J Clin Psychiatry. 2016;77(7):957–62.
Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38.
Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–83.
Lipton RB, Dodick D, Sadovsky R, Kolodner K, Endicott J, Hettiarachchi J. Harrison W and study IDMv. A self-administered screener for migraine in primary care: The ID Migraine validation study Neurology. 2003;61:375–82.
Zarifoglu M, Karli N, Taskapilioglu O. Can ID Migraine be used as a screening test for adolescent migraine? Cephalalgia : an international journal of headache. 2008;28:65–71.
Bicakci S, Bozdemir N, Over F, Saatci E, Sarica Y. Prevalence of migraine diagnosis using ID Migraine among university students in southern Turkey. The Journal of Headache and Pain. 2008;9(3):159–63.
Oztora S, Korkmaz O, Dagdeviren N, et al. Migraine headaches among university students using id migraine test as a screening tool. BMC Neurol. 2011;11:103.
Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109:45–60.
McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: results from a nationally representative sample. Pain. 2004;111:77–83.
Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN guidelines for prevention of episodic migraine: a summary and comparison with other recent clinical practice guidelines. Headache. 2012;52(6):930–45.
Pringsheim T, Davenport W, Mackie G, Worthington I, Aubé M, Christie SN, Gladstone J, Becker WJ. Canadian headache society prophylactic guidelines development group. Canadian headache society guideline for migraine prophylaxis. Can J Neurol Sci. 2012;39(2 Suppl 2):S1–59.
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Quality standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the quality standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337–45.
Ozyalcin SN1, Talu GK, Kiziltan E, Yucel B, Ertas M, Disci R. The efficacy and safety of venlafaxine in the prophylaxis of migraine. Headache 45(2):144–152, 2005.
Tarlaci S. Escitalopram and venlafaxine for the prophylaxis of migraine headache without mood disorders. Clin Neuropharmacology. 2009;32(5):254–8.
Gelfand AA. Psychiatric comorbidity and paediatric migraine: examining the evidence. Curr Opin Neurol. 2015;28:261–4.
Buse DC, Andrasik F. Behavioral medicine for migraine. Neurol Clin. 2009;27:445–65.
Cahill CM, Murphy KC. Migraine: another headache for psychiatrists? Br J Psychiatry. 2004;185:191–3.
Bigal ME, Lipton RB. Modifiable risk factors for migraine progression. Headache. 2006;46:1334–43.
Breslau N, Lipton RB, Stewart WF, Schultz LR, Welch KM. Comorbidity of migraine and depression: investigating potential etiology and prognosis. Neurology. 2003;60:1308–12.
Merikangas KR, Angst J, Isler H. Migraine and psychopathology. Results of the Zurich cohort study of young adults Arch Gen Psychiatry. 1990;47:849–53.
Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–7.
Chiros C, O'Brien WH. Acceptance, appraisals, and coping in relation to migraine headache: an evaluation of interrelationships using daily diary methods. J Behav Med. 2011;34:307–20.
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25.
Dindo L, Recober A, Marchman J, O'Hara M, Turvey C. Depression and disability in migraine: the role of pain acceptance and values-based action. International journal of behavioral medicine. 2015;22:109–17.
Dindo L, Recober A, Marchman J, O'Hara MW, Turvey C. One-day behavioral intervention in depressed migraine patients: effects on headache. Headache. 2014;54:528–38.
Hayes SC, Pistorello J, Levin ME. Acceptance and commitment therapy as a unified model of behavior change. Couns Psychol. 2012;40:976–1002.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was funded by the National Institute of Mental Health (R01MH090072) and the National Center for Research Resources (2UL1TR000442-06) to the senior author C.C. It was also funded by the National Institute of Mental Health (K23MH097827) and was partially supported with resources and the use of facilities at the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN13-413) to the first author L.D.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies, the Department of Veterans Affairs, the US government, or Baylor College of Medicine. The funding agencies had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review or approval of the manuscript. The authors are grateful for the contributions of the participants and their families as well as for those of the research team.
Aspects of this work have been accepted for presentation at the Annual Meeting of the American Academy of Child and Adolescent Psychiatry, on October 29, 2015, in San Antonio, TX.
ClinicalTrials.gov Identifier: NCT02147184.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the University of Iowa Institutional Review Board.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Dindo, L.N., Recober, A., Haddad, R. et al. Comorbidity of Migraine, Major Depressive Disorder, and Generalized Anxiety Disorder in Adolescents and Young Adults. Int.J. Behav. Med. 24, 528–534 (2017). https://doi.org/10.1007/s12529-016-9620-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-016-9620-5