Abstract
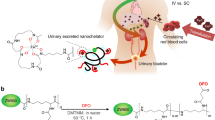
Iron chelation therapy is an effective approach to the treatment of iron overload conditions, in which iron builds up to toxic levels in the body and may cause organ damage. Treatments using deferoxamine, deferasirox and deferiprone have been introduced and despite their disadvantages, they remain the first-line therapeutics in iron chelation therapy. Our study aimed to compare the effectiveness of the iron chelation agent TLc-A, a nano chelator synthetized based on the novel nanochelating technology, with deferoxamine. We found that TLc-A reduced iron overload in Caco2 cell line more efficiently than deferoxamine. In rats with iron overload, very low concentrations of TLc-A lowered serum iron level after only three injections of the nanochelator, while deferoxamine was unable to reduce iron level after the same number of injections. Compared with deferoxamine, TLc-A significantly increased urinary iron excretion and reduced hepatic iron content. The toxicity study showed that the intraperitoneal median lethal dose for TLc-A was at least two times higher than that for deferoxamine. In conclusion, our in vitro and in vivo studies indicate that the novel nano chelator compound, TLc-A, offers superior performance in iron reduction than the commercially available and widely used deferoxamine.








Similar content being viewed by others
References
MacKenzie EL, Iwasaki K, Tsuji Y. Intracellular iron transport and storage: from molecular mechanisms to health implications. Antioxid Redox Signal. 2008;10:997–1030.
Jacobs A. Low molecular weight intracellular iron transport compounds. Blood. 1977;50:433–9.
Breuer W, Greenberg E, Cabantchik ZI. Newly delivered transferrin iron and oxidative cell injury. FEBS Lett. 1997;403:213–9.
Marsella M, Borgna-Pignatti C. Transfusional iron overload and iron chelation therapy in thalassemia major and sickle cell disease. Hematol/Oncol Clin N Am. 2014;28:703–27.
Mair SM, Weiss G. New pharmacological concepts for the treatment of iron overload disorders. Curr Med Chem. 2009;16:576–90.
Danjou F, Origa R, Anni F, Saba L, Cossa S, Podda G, et al. Longitudinal analysis of heart and liver iron in thalassemia major patients according to chelation treatment. Blood Cells Mol Dis. 2013;51:142–5.
Angelucci E, Baronciani D, Lucarelli G, Baldassarri M, Galimberti M, Giardini C, et al. Needle liver biopsy in thalassaemia: analyses of diagnostic accuracy and safety in 1184 consecutive biopsies. Br J Haematol. 1995;89:757–61.
Aessopos A, Berdoukas V, Tsironi M. The heart in transfusion dependent homozygous thalassaemia today–prediction, prevention and management. Eur J Haematol. 2008;80:93–106.
Ceci A, Felisi M, De Sanctis V, De Mattia D. Pharmacotherapy of iron overload in thalassaemic patients. Expert Opin Pharmacother. 2003;4:1763–74.
Keberle H. The biochemistry of desferrioxamine and its relation to iron metabolism. Ann N Y Acad Sci. 1964;119:758–68.
Zanninelli G, Glickstein H, Breuer W, Milgram P, Brissot P, Hider RC, et al. Chelation and mobilization of cellular iron by different classes of chelators. Mol Pharmacol. 1997;51:842–52.
Olivieri NF, Nathan DG, MacMillan JH, Wayne AS, Liu PP, McGee A, et al. Survival in medically treated patients with homozygous beta-thalassemia. N Engl J Med. 1994;331:574–8.
Baath JS, Lam WC, Kirby M, Chun A. Deferoxamine-related ocular toxicity: incidence and outcome in a pediatric population. Retina. 2008;28:894–9.
Anderson LJ, Wonke B, Prescott E, Holden S, Walker JM, Pennell DJ. Comparison of effects of oral deferiprone and subcutaneous desferrioxamine on myocardial iron concentrations and ventricular function in beta-thalassaemia. Lancet. 2002;360:516–20.
Otto-Duessel M, Brewer C, Gonzalez I, Nick H, Wood JC. Safety and efficacy of combined chelation therapy with deferasirox and deferoxamine in a gerbil model of iron overload. Acta Haematol. 2008;120:123–8.
Cohen AR, Galanello R, Piga A, De Sanctis V, Tricta F. Safety and effectiveness of long-term therapy with the oral iron chelator deferiprone. Blood. 2003;102:1583–7.
Henter JI, Karlen J. Fatal agranulocytosis after deferiprone therapy in a child with Diamond-Blackfan anemia. Blood. 2007;109:5157–9.
Hershko C, Link G, Konijn AM, Cabantchik ZI. Objectives and mechanism of iron chelation therapy. Ann N Y Acad Sci. 2005;1054:124–35.
Aslam N, Mettu P, Marsano-Obando LS, Martin A. Deferasirox induced liver injury in haemochromatosis. J Coll Physicians Surg-Pak: JCPSP. 2010;20:551–3.
Imran FS, Phatak P. Deferasirox induced liver injury in haemochromatosis. J Coll Physicians Surg-Pak: JCPSP. 2011;21:718 (author reply).
Kontoghiorghes GJ. Introduction of higher doses of deferasirox: better efficacy but not effective iron removal from the heart and increased risks of serious toxicities. Expert Opin Drug Saf. 2010;9:633–41.
Peters R. The nanopore connection to cell membrane unitary permeability. Traffic. 2005;6:199–204.
Boyapalle S, Mohapatra S, Mohapatra S. Nanotechnology applications to HIV vaccines and microbicides. J Glob Infect Dis. 2012;4:62–8.
Lee ES, Gao Z, Bae YH. Recent progress in tumor pH targeting nanotechnology. J Controll Release: Off J Controll Release Soc. 2008;132:164–70.
Fakharzadeh S, Kalanaky S, Hafizi M, Goya MM, Masoumi Z, Namaki S, et al. The new nano-complex, Hep-c, improves the immunogenicity of the hepatitis B vaccine. Vaccine. 2013;31:2591–7.
Fakharzadeh S, Sahraian MA, Hafizi M, Kalanaky S, Masoumi Z, Mahdavi M, et al. The therapeutic effects of MSc1 nanocomplex, synthesized by nanochelating technology, on experimental autoimmune encephalomyelitic C57/BL6 mice. Int J Nanomed. 2014;9:3841–53.
Maghsoudi A, Fakharzadeh S, Hafizi M, Abbasi M, Kohram F, Sardab S, et al. Neuroprotective effects of three different sizes nanochelating based nano complexes in MPP(+) induced neurotoxicity. Apoptosis Int J Program Cell Death. 2015;20:298–309.
Nazaran MH. Chelate compounds. Google Patents US8288587; 2012.
Pantalone GR, Maggio A, Vitrano A, Capra M, Cuccia L, Gagliardotto F, et al. Sequential alternating deferiprone and deferoxamine treatment compared to deferiprone monotherapy: main findings and clinical follow-up of a large multicenter randomized clinical trial in -thalassemia major patients. Hemoglobin. 2011;35:206–16.
Spraul CW, Schicketanz C. Lang GE [Ocular side effects of deferoxamine therapy in aplastic anemia with transfusion-induced hemochromatosis]. Klin Monatsbl Augenheilkd. 1996;209:31–6.
Porter JB, Taher AT, Cappellini MD, Vichinsky EP. Ethical issues and risk/benefit assessment of iron chelation therapy: advances with deferiprone/deferoxamine combinations and concerns about the safety, efficacy and costs of deferasirox. Hemoglobin. 2008;32:601–7.
Kontoghiorghes GJ. Hemoglobin. 2008;32(1–2):1–15.
Payne KA, Rofail D, Baladi JF, Viala M, Abetz L, Desrosiers MP, et al. Iron chelation therapy: clinical effectiveness, economic burden and quality of life in patients with iron overload. Adv Ther. 2008;25:725–42.
Cario H, Janka-Schaub G, Janssen G, Jarisch A, Strauss G, Kohne E. Recent developments in iron chelation therapy. Klin Padiatr. 2007;219:158–65.
Liu G, Men P, Perry G, Smith MA. Nanoparticle and iron chelators as a potential novel Alzheimer therapy. Methods Mol Biol. 2010;610:123–44.
Bonda DJ, Liu G, Men P, Perry G, Smith MA, Zhu X. Nanoparticle delivery of transition-metal chelators to the brain: oxidative stress will never see it coming! CNS Neurol Disord: Drug Targets. 2012;11:81–5.
Liu G, Men P, Perry G, Smith MA. Chapter 5—Development of iron chelator-nanoparticle conjugates as potential therapeutic agents for Alzheimer disease. Prog Brain Res. 2009;180:97–108.
Seshadri R, Colebatch JH, Fisher R. Urinary iron excretion in thalassaemia after desferrioxamine administration. Arch Dis Child. 1974;49:195–9.
Musallam KM, Cappellini MD, Wood JC, Taher AT. Iron overload in non-transfusion-dependent thalassemia: a clinical perspective. Blood Rev. 2012;26(Suppl 1):S16–9.
Papastamataki M, Delaporta P, Premetis E, Kattamis A, Ladis V, Papassotiriou I. Evaluation of liver fibrosis in patients with thalassemia: the important role of hyaluronic acid. Blood Cells Mol Dis. 2010;45:215–8.
Hodges YK, Weinberger HD, Stephens J, Horwitz MA, Horwitz LD. Desferri-exochelin, a lipid-soluble, hexadentate iron chelator, effectively removes tissue iron. Transl Res: J Lab Clin Med. 2006;148:63–71.
Acknowledgments
All financial support was provided by the Department of Research and Development at the Sodour Ahrar Shargh Company. We are grateful to Etrat S Moghimi and Fakhrosadat Nasiri for their help in this project.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The other authors report no conflicts of interest in this work.
Additional information
M. H. Nazaran is the owner of Nanochelating technology and executive manager and chairman of the management board of Sodour Ahrar Shargh Company.
About this article
Cite this article
Kalanaky, S., Hafizi, M., Safari, S. et al. TLc-A, the leading nanochelating-based nanochelator, reduces iron overload in vitro and in vivo. Int J Hematol 103, 274–282 (2016). https://doi.org/10.1007/s12185-015-1932-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1932-8