Abstract
Background and goals
Liver fibrosis influences treatment and surveillance strategies in chronic hepatitis B (CHB). This multicenter study aimed to examine the accuracy of serum fibrosis models in CHB patients including those with low alanine aminotransferase (ALT) levels and serially in those undergoing treatment.
Method
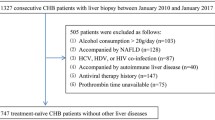
We examined noninvasive fibrosis models [Hepascore, Fibrotest, APRI, hepatitis e antigen (HBeAg)-positive and -negative models] in 179 CHB patients who underwent liver biopsy and fibrosis assessment by METAVIR and image morphometry. Serial Hepascore measurements were assessed in 40 subjects for up to 8.7 years.
Results
Hepascore was more accurate than Fibrotest [area under the curve (AUC) 0.83 vs. 0.72, P = 0.05] and HBeAg-positive model (AUC 0.83 vs. 72, P = 0.03) for significant fibrosis but was not significantly different to APRI or HBeAg-negative scores. Fibrosis area assessed by morphometry was correlated with Hepascore (r = 0.603, P < 0.001), Fibrotest (r = 0.392, P = 0.03), and HBeAg-positive (r = 0.492, P = 0.001) scores only. Among 73 patients with an ALT <60 IU/L, noninvasive models were useful to predict fibrosis (PPV 80–90%) or exclude significant fibrosis (NPV 79–100%). Hepascore increased significantly among patients monitored without treatment and reduced among patients undergoing therapy (0.05/year ± 0.03 vs. −0.04/year ± 0.02, P = 0.007).
Conclusions
Serum fibrosis models are predictive of fibrosis in CHB and assist in identifying subjects with low–normal ALT levels for treatment.




Similar content being viewed by others
References
Lee WM. Hepatitis B virus infection. N Engl J Med 1997;337:1733–1745
Sorrell MF, Belongia EA, Costa J, et al. National Institutes of Health Consensus Development conference statement: management of hepatitis B. Ann Intern Med 2009;150:104–110
Belongia EA, Costa J, Gareen IF, et al. NIH consensus development statement on management of hepatitis B. NIH Consens State Sci Statements 2008;25:1–29
McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology 1990;99:1396–1400
Van Thiel DH, Gavaler JS, Wright H, Tzakis A. Liver biopsy. Its safety and complications as seen at a liver transplant center. Transplantation 1993;55:1087–1090
Marcellin P, Asselah T, Boyer N. Fibrosis and disease progression in hepatitis C. Hepatology 2002;36:S47–S56
Kumar M, Sarin SK, Hissar S, et al. Virologic and histologic features of chronic hepatitis B virus-infected asymptomatic patients with persistently normal ALT. Gastroenterology 2008;134:1376–1384
Lai M, Hyatt BJ, Nasser I, Curry M, Afdhal NH. The clinical significance of persistently normal ALT in chronic hepatitis B infection. J Hepatol 2007;47:760–767
Zeng M, Lu LG, Mao Y, et al. Prediction of significant fibrosis in HBeAg-positive patients with chroic hepatitis B by a noninvasive model. Hepatology 2005;42:1437–1445
Mohamadnejad M, Montazeri G, Fazlollahi A, et al. Noninvasive markers of liver fibrosis and inflammation in chronic hepatitis B-virus related liver disease. Am J Gastroenterol 2006;101:2345–2537
Adams LA, Bulsara M, Rossi E, et al. Hepascore: an accurate validated predictor of liver fibrosis in chronic hepatitis C infection. Clin Chem 2005;51:1867–1873
Castera L, Vergniol J, Foucher J, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic Hepatitis C. Gastroenterology 2005;128:343–350
Chun-Tao W, Joel KG, Robert JF, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003;38:518–526
Goodman ZD, Stoddard AM, Bonkovsky HL, et al. Fibrosis progression in chronic hepatitis C: morphometric image analysis in the HALT-C trial. Hepatology 2009;50:1738–1749
Hu KQ, Schiff ER, Kowdley KV, et al. Histologic evidence of active liver injury in chronic hepatitis B patients with normal range or minimally elevated alanine aminotransferase levels. J Clin Gastroenterol 2010;44:510–516
Rossi E, Adams L, Prins A, et al. Validation of the FibroTest biochemical markers score in assessing liver fibrosis in hepatitis C patients. Clin Chem 2003;49:450–454
Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative study group. Hepatology 1996;24:289–293
Bottero J, Lacombe K, Guechot J, et al. Performance of 11 biomarkers for liver fibrosis assessment in HIV/HBV co-infected patients. J Hepatol 2009;50:1074–1083
Myers RP, Tainturier MH, Ratziu V, et al. Prediction of liver histological lesions with biochemical markers in patients with chronic hepatitis B. J Hepatol 2003;39:222–230
Afdhal NH, Curry M. Technology evaluation: a critical step in the clinical utilization of novel diagnostic tests for liver fibrosis. J Hepatol 2007;46:543–545
Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology 2009;50:661–662
Dienstag JL, Goldin RD, Heathcote EJ, et al. Histological outcome during long-term lamivudine therapy. Gastroenterology 2003;124:105–117
Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, et al. Long-term therapy with adefovir dipivoxil for HBeAg-negative chronic hepatitis B for up to 5 years. Gastroenterology 2006;131:1743–1751
Acknowledgements
The authors acknowledge the facilities, scientific and technical assistance of the Australian Microscopy and Microanalysis Research Facility at the Centre for Microscopy, Characterization and Analysis, The University of Western Australia, a facility funded by The University, State, and Commonwealth Governments. This study was sponsored by a Seeding Research Grant from the University of Western Australia, Faculty of Medicine, Dentistry and Health Sciences, and a Clinical Research Grant from Bristol Meyers Squibb Australia Pvt Ltd.
Conflict of interest
The University of Western Australia (employers of LAA, ER, GPJ, MB,) has a licensing agreement with Quest Diagnostics regarding Hepascore. JG is supported by a STREP grant from The Cancer Council NSW and the Robert W. Storr Bequest to the University of Sydney.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raftopoulos, S.C., George, J., Bourliere, M. et al. Comparison of noninvasive models of fibrosis in chronic hepatitis B. Hepatol Int 6, 457–467 (2012). https://doi.org/10.1007/s12072-011-9296-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-011-9296-5